Abstract
Purpose
To identify modifiable risk factors in early midlife associated with incident hypertension 26 years later in women and men.
Materials and methods
We used data from 1025 women and 703 men in the community-based Hordaland Health Study examined at the mean age of 42 years (baseline) and after a 26-year follow-up. Patients with hypertension at baseline were excluded. Blood pressure (BP) was classified according to European guidelines. Factors associated with incident hypertension were identified in logistic regression analyses.
Results
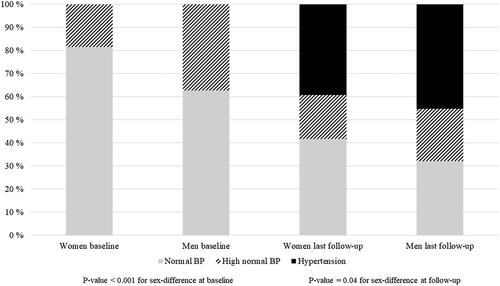
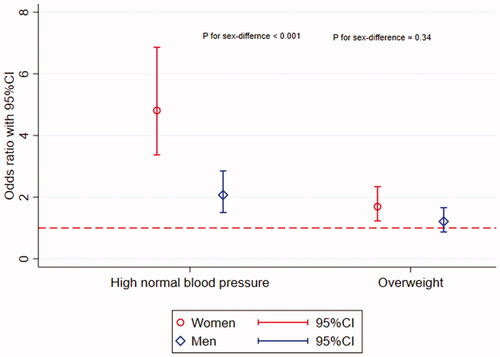
At baseline, women had a lower average BP and a lower prevalence of high-normal BP (19% vs 37%, p < .05). Overall, 39% of women and 45% of men developed hypertension during follow-up (p < .05). Among those with high-normal BP at baseline, 72% of women and 58% of men developed hypertension (p < .01). In multivariable logistic regression analyses, high-normal BP at baseline was a stronger predictor of incident hypertension in women (odds ratio, OR 4.8, [95% confidence interval, CI 3.4–6.9]) than in men (OR 2.1, [95% CI 1.5–2.8]), p < .01 for sex interaction. A higher baseline body mass index (BMI) was associated with incident hypertension in both sexes.
Conclusions
High-normal BP in midlife is a stronger risk factor for developing hypertension 26 years later in women than in men, independent of BMI.
Plain language summary
There is a knowledge gap regarding the understanding of sex differences in hypertension and cardiovascular disease. The World Health Organisation has identified hypertension as the leading cause of morbidity and mortality in women.
This manuscript focuses on sex differences in risk factors in early midlife associated with the development of hypertension 26 years later. We studied 1025 women and 703 men who participated in the community-based Hordaland Health Study at the age of 42 years, and after 26 years. Factors associated with hypertension were identified in statistical analyses.
Our main findings were that having a high-normal blood pressure (systolic blood pressure 130–139 mmHg or a diastolic blood pressure 85–89 mmHg) in midlife was a significantly stronger risk factor for the development of hypertension in women than in men during follow-up. Having a higher body mass index in midlife was associated with the development of hypertension in both sexes.
This study contributes to the understanding of sex differences in hypertension development and adds further knowledge regarding high-normal blood pressure as a particularly important risk factor for hypertension and cardiovascular disease in women.
Introduction
Hypertension is a major risk factor for cardiovascular disease (CVD) in both women and men, pointing to the importance of preventing hypertension [Citation1,Citation2]. Although BP is lower in young women than in men of similar age, all components of BP increase more steeply in women starting as early as in the third decade of life [Citation2]. The mechanisms behind this sex difference in the development of BP are incompletely understood but have been attributed to reproductive events in women such as hypertensive pregnancy complications and menopause [Citation3,Citation4]. However, hypertensive pregnancy disorders affect only 5%–10% of pregnancies [Citation5], and a rapid BP increase during the first year after menopause was found in only 35% of women in the Study across the Nation [Citation3,Citation6]. Furthermore, Cifkova et al. found that new-onset hypertension during the menopausal transition was particularly common in women with a clustering of metabolic risk factors [Citation7].
In studies that include both sexes, weight gain has been suggested to be the main cause of the development of hypertension [Citation8–10]. In the Framingham Heart Study, a 5% weight gain in midlife was associated with 20–30% increased odds of hypertension over 4 years [Citation9]. In normotensive, middle-aged participants in the Strong Heart Study, increased waist circumference, reflecting visceral obesity, was a main predictor of hypertension 8 years later [Citation10]. However, these studies had a relatively short follow-up time, and most did not report sex-specific results. Thus, there is a lack of sex-specific information on health factors in midlife associated with incident hypertension later in life. In this study population, we have previously shown that the development of hypertension during the first six years of follow-up was associated with high-normal BP at baseline in both sexes [Citation8]. The current study aimed to expand these findings with a follow-up period of up to 26 years.
Methods
Study population
The Hordaland Health study is a community-based study in Hordaland County in Western Norway, initiated as a collaboration between the National Health Screening Service, the University of Bergen, and local health services in 1992 (https://husk-en.w.uib.no/) [Citation11,Citation12]. Three surveys have been conducted within the Hordaland Health Study, in 1992/93, 1997/99 and 2018–2020, respectively. Participants were invited based on year of birth and site of residence. In total, approximately 36,000 residents of Hordaland County participated in the two first surveys. Participants born in 1950–51, who had participated in both previous surveys, were invited for the third survey. From a total of 4849 individuals born 1950–51 who participated in the first survey, 3733 participated also in the second survey. Of these, 3304 were still alive and living in Hordaland County in 2018. These participants received a personal invitation by mail, and 2252 accepted the invitation and signed electronic informed consent. Of these, 2183 (64%) showed up at the clinical visit.
The current study focuses on the 1194 women and 989 men born in 1950–51 who participated in both the first survey at age of 42 years (baseline) and in the follow-up surveys after 26 years. Participants who lacked data on BP (n = 8), body mass index (BMI) (n = 2), heart rate (n = 1), level of education (n = 7), and patients with hypertension or on antihypertensive medication at baseline were excluded (n = 380). Thus, a total of 1025 women and 703 men were eligible for the present analyses.
All participants provided their informed consent. The present study was carried out in accordance with the Declaration of Helsinki, and the study protocol was approved by the Regional Committee for Medical and Health Research Ethics (2017/294).
Baseline blood pressure measurements
Attended BP measurements were performed by trained nurses and bioengineers. Brachial BP was measured with calibrated sphygmomanometers and the appropriate cuff size using a Dinamap 845 XT or Dinamap 8100 sphygmomanometer (Critikon, Tampa, FL) at baseline and by an OMRON HEM-907 (OMRON Healthcare, Kyoto, Japan) at follow-up. Three measurements were performed at 1-minute intervals after a minimum of 5 min of initial rest in the seated position. The average of the two last measurements was taken as the clinic BP and used for the analyses. BP was classified according to the European Society of Cardiology/European Society of Hypertension guidelines[Citation13]. High-normal BP was defined as a systolic BP of 130–139 mmHg or a diastolic BP of 85–89 mmHg. Hypertension was defined as a systolic BP ≥140 mmHg or a diastolic BP ≥90 mmHg.
Other cardiovascular risk factors
Medical history, smoking, alcohol intake, education, menopausal status, drug use including contraceptive pills, hormone replacement therapy, antihypertensive medication, and time since last meal were collected in self-reported questionnaires in both surveys. Menopause was defined as 1 year since the last menstruation. Height was measured to the nearest centimetre, and weight with light clothing to the nearest half-kilogram on a calibrated scale. BMI was calculated as weight in kg/height2. Overweight was defined as a BMI ≥25 kg/m2. Smoking was defined as current daily smoking. Level of education was classified as (1) primary education/lower secondary school, (2) upper secondary school, and (3) higher education. Physical activity level was classified as sedentary or non-sedentary. Sedentary participants performed less than 4 h of moderate or physically vigorous activity a week. One alcohol unit is defined as one glass of wine, a half-litre of ordinary strength lager, or a single shot of spirits.
Outcome
Incident hypertension at follow-up after 26 years, defined as measured systolic BP ≥140 mmHg or diastolic BP ≥ 90 mmHg, or self-reported use of antihypertensive medication.
Statistical analyses
Analyses were done using the STATA statistical software package, version 17 (StataCorp, Texas, USA). Continuous variables are expressed as means and standard deviations (SD) or medians and interquartile ranges (IQR), and categorical variables as numbers and percentages. Comparisons between groups were done using the Student’s t-test, analyses of variance (ANOVA) with Tukey post hoc test, or by the Chi-square test, as appropriate. For non-normally distributed variables (serum triglycerides) comparisons between groups were done by quantile regression. Baseline health factors associated with incident hypertension after 26 years of follow-up were identified in uni- and multivariable logistic regression analyses. Results are reported as odds ratios (OR) with 95% confidence intervals (CI) and p-values. The main model included baseline BMI, high-normal BP, heart rate, physical activity, daily smoking, serum total cholesterol, serum triglycerides and level of education at baseline as covariates. We also ran this analysis, excluding participants who experienced a CVD event during follow-up. To assess the impact of the clinical condition ‘overweight’ we performed a secondary analysis where we replaced baseline BMI with overweight (BMI ≥25.0 kg/m2). A supplementary model aimed to identify associations between changes in metabolic factors (BMI, serum total cholesterol and serum triglycerides) over 26 years with incident hypertension in uni- and multivariable logistic regression analyses. This model was adjusted for heart rate, physical activity, daily smoking, level of education at baseline, and changes in BMI, serum total cholesterol, and serum triglycerides. To test for interactions between explanatory variables and sex in the total study population, we compared a model with an interaction term with a model without an interaction term, using the likelihood-ratio test. A two-tailed p-value of <.05 was considered statistically significant.
Results
At baseline, women had lower systolic and diastolic BP, and a lower prevalence of high-normal BP than men (all p < .001) (). Among participants with a high-normal BP at baseline, a larger proportion of men than women had high-normal systolic BP (94% vs 85% p = .002), while a larger proportion of women than men had high-normal diastolic BP (37% vs 28%, p = .04). The prevalence of combined high-normal systolic and high-normal diastolic BP did not differ by sex (p = .90). At baseline, women also had a lower BMI, serum triglycerides and serum total cholesterol, a higher heart rate, and a smaller proportion were overweight (all p < .001) (). No significant differences between sexes were found for physical activity or smoking (both p > .7), but men had a higher intake of alcohol (p < .001). At baseline, 1.1% of women reported having passed menopause. Five participants had diabetes at baseline, one woman and four men.
Table 1. Characteristics of the study population at baseline and 26-year follow-up.
When dividing women and men into groups with normal and high-normal BP at baseline, we found a higher proportion of overweight in women with a high-normal BP compared to those with normal BP, while this was not seen in men. ().
Table 2. Characteristics of women and men grouped according to BP categories at baseline.
Factors associated with incident hypertension after 26 years of follow-up
In total, 403 (39%) women and 318 (45%) men had developed hypertension after 26 years of follow-up (p < .05). Of these, 70% of women and 72% of men (p = .41) used antihypertensive medication. Among participants with normal BP at baseline, 32% of women and 38% of men developed hypertension (p < .001). Among participants with high-normal BP at baseline, 72% of women and 58% of men developed hypertension during follow-up (p < .001) (). Women and men who remained normotensive at the last follow-up were characterised by lower BMI and lower serum triglycerides than their hypertensive counterparts. Furthermore, women who remained normotensive also had higher serum total cholesterol and lower heart rate than women with hypertension at follow-up (Table S1).
Women
In univariate analyses, incident hypertension at the 26-year follow-up was associated with high-normal BP, overweight, higher BMI, and serum triglycerides at baseline and with lower education (all p < .02). No association was found with menopausal status at baseline. In multivariable analyses, incident hypertension was associated with high-normal BP and higher BMI at baseline (), and when BMI was replaced by overweight in the model, also with baseline overweight (all p < .001) (Table S2). Being a daily smoker was associated with a lower risk of incident hypertension in women, in both univariate and multivariable analyses (). Excluding women who experienced CVD during follow-up (1.6%) did not change the results for the association of high-normal BP with incident hypertension (OR 3.98 [95% CI 2.84–5.61], p < .001).
Table 3. Health factors in midlife associated with incident hypertension 26 years later.
In a secondary adjusted model, an increase in BMI over 26 years of follow-up was significantly associated with incident hypertension in women (Table S3). Furthermore, a decrease in serum total cholesterol and an increase in serum triglycerides were associated with incident hypertension in women (Table S3).
Men
In univariate analyses, incident hypertension was associated with baseline high-normal BP, lower education, overweight, as well as higher BMI, heart rate, serum triglycerides, and serum total cholesterol at baseline (all p < .05). In multivariable analyses, incident hypertension was associated with having a high-normal BP and higher BMI at baseline (both p < .02) (). Excluding men who experienced CVD during follow-up (6.8%) did not change the results for the association of high-normal BP with incident hypertension (OR 2.07 [95% CI 1.50–2.87], p < .001).
In a secondary adjusted model, an increase in BMI and a decrease in serum total cholesterol over 26 years of follow-up were significantly associated with incident hypertension in men (Table S2).
Sex-interaction analysis
Having a high-normal BP at baseline was a significant risk factor for incident hypertension at follow-up in both sexes, but the association was stronger for women (), as documented with a significant interaction test for sex (p < .001). Sex interaction remained significant (p = .001) in the model excluding participants who experienced CVD during follow-up. Being overweight at baseline was significantly associated with incident hypertension in the multivariable analysis for women only () (Table S3), but a significant interaction test for sex was not found (p = .34).
Figure 2. Associations of high-normal BP and overweight with risk of incident hypertension over 26 years in women and men. P for sex-difference is the p-value for sex-interaction in multivariable regression analyses.
No sex difference was documented in sex-interaction analyses for the association between change in metabolic variables during follow-up and incident hypertension (all p > .05).
Discussion
The present study adds sex-specific knowledge on the association of health factors in early midlife with incident hypertension in the subsequent 26 years. Women with high-normal BP in their early 40s had a significantly higher risk of developing hypertension during follow-up than their male counterparts, independent of the presence of overweight. Our findings expand the previous observation of a greater increase in BP in women than men during early midlife [Citation8] and demonstrates that high-normal BP in early midlife is particularly associated with increased long-term risk for hypertension in women.
It is well known that high-normal BP can progress to hypertension, especially when clustering of metabolic risk factors is present [Citation8–10]. However, sex-specific data are scarce. In the Framingham Heart Study, Vasan et al. found that the progression from high-normal BP to hypertension was twice as common in middle-aged subjects compared to older subjects [Citation9]. In American Indians participating in the Strong Heart Study, 38% of, on average 59 years old participants with high-normal BP, developed hypertension during 4 years of follow-up [Citation10]. The progression to hypertension was particularly associated with a higher baseline waist circumference and the presence of diabetes or left ventricular hypertrophy [Citation10].
High-normal BP in early midlife has emerged as a particularly important risk factor for CVD in women [Citation14–17]. In a recent meta-analysis of 47 studies, high-normal BP was associated with a 2-fold higher risk of CVD [Citation14]. Wang et al. found that this risk was limited to subjects younger than 70 years of age in the general population of the United States [Citation15]. In the Hordaland Health Study, we previously reported that high-normal BP in early midlife was associated with a 2-fold increased risk for hospitalisation for acute coronary syndromes in women before the age of 60 years, independent of the presence of other CVD risk factors, while this risk was not observed in men at similar age [Citation16]. Similar observations have been reported from the UK Biobank study, finding high-normal BP to carry a 40% higher risk for acute myocardial infarction in women than in men younger than 60 years [Citation17].
In a previous report from the Hordaland Health Study, a single unit higher BMI in 42-year-old subjects was associated with an 11% higher risk of hypertension in women and 10% in men over 6 years of follow-up [Citation8]. In the present study, higher BMI in early midlife remained associated with an increased risk of incident hypertension during 26 years of follow-up in both women and men. Despite overweight being more common in men than women at baseline, overweight was associated with incident hypertension during follow-up only in women after adjustment for other risk factors. This is in line with previous findings in the Strong Heart Study [Citation10]. The significant association of daily smoking with reduced risk of incident hypertension is in line with findings in previous observational studies [Citation18].
Dyslipidemia is highly prevalent in subjects with high-normal BP and is associated with atheromatosis and an increased risk of CVD [Citation19]. Previous publications have documented sex differences in the life course development of serum total cholesterol, as also reflected in our results [Citation20]. As expected, more men than women reported the use of lipid-lowering medication at follow-up. However, no significant associations between serum total cholesterol at baseline with incident hypertension was found in the adjusted analysis in either sex.
Study limitations
The Hordaland Health Study was performed in a limited geographical area in Western Norway and the study included primarily Caucasians. Generalisability to other ethnicities should be done with caution. Among patients with hypertension at the last follow-up, 53% were classified based on self-reported use of antihypertensive medication, pointing to the potential for improving the management of hypertension and preventing CVD. It is also possible that some of these participants were using these medications for other indications and thus could have been misclassified. However, fewer than 4% of participants experienced hospitalisation for myocardial infarction, angina pectoris, heart failure, or stroke during follow-up.
Hypertensive disorders complicate 5–10% of pregnancies and are associated with an increased risk of hypertension and increased arterial stiffness in midlife [Citation4,Citation21]. We did not have information on hypertensive disorders during pregnancy in our cohort. BP classification was based on BP measured in triplets at a single baseline visit, and therefore, the prevalence of hypertension at baseline may have been overestimated. Since fasting blood sugar was not measured at baseline, the prevalence of diabetes may have been underestimated. However, obesity at baseline was rare, 3.2% in our cohort, reducing the probability of type 2 diabetes. Finally, we did not have information regarding serum LDL and HDL cholesterol levels or the use of cholesterol-lowering drugs. The prospective design, the size of the study sample, the high participation rate above 64% in both surveys, and the length of follow-up are strengths of our study.
Conclusion
In the Hordaland Health study, having a high-normal BP in midlife was a stronger risk factor for the development of hypertension later in life in women than in men. Having a higher BMI in midlife was associated with incident hypertension in both sexes. Systematic follow-up of subjects with high-normal BP in their forties may improve early detection of hypertension in women.
Authors contributions
All listed Authors have contributed substantially to the manuscript and agreed to the final submitted version.
Supplemental Material
Download MS Word (23 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Participants in this study have not agreed to allow their data to be publicly shared, so supporting data are not available.
Additional information
Funding
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222.
- Ji H, Kim A, Ebinger JE, et al. Sex differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;5(3):19–26.
- Samargandy S, Matthews KA, Brooks MM, et al. Trajectories of blood pressure in midlife women: does menopause matter? Circ Res. 2022;130(3):312–322.
- Garovic VD, August P. Preeclampsia and the future risk of hypertension: the pregnant evidence. Curr Hypertens Rep. 2013;15(2):114–121.
- Riise HKR, Sulo G, Tell GS, et al. Hypertensive pregnancy disorders increase the risk of maternal cardiovascular disease after adjustment for cardiovascular risk factors. Int J Cardiol. 2019;282:81–87.
- Maas A, Rosano G, Cifkova R, et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: a consensus document from european cardiologists, gynaecologists, and endocrinologists. Eur Heart J. 2021;42(10):967–984.
- Cifkova R, Pitha J, Lejskova M, et al. Blood pressure around the menopause: a population study. J Hypertens. 2008;26(10):1976–1982.
- Kringeland E, Tell GS, Midtbo H, et al. Factors associated with increase in blood pressure and incident hypertension in early midlife: the Hordaland Health Study. Blood Press. 2020;29(5):267–275.
- Vasan RS, Larson MG, Leip EP, et al. Assessment of frequency of progression to hypertension in non-hypertensive participants in the framingham heart study: a cohort study. Lancet. 2001;358(9294):1682–1686.
- de Simone G, Devereux RB, Chinali M, et al. Risk factors for arterial hypertension in adults with initial optimal blood pressure: the strong heart study. Hypertension. 2006;47(2):162–167.
- Refsum H, Nurk E, Smith AD, et al. The Hordaland homocysteine study: a community-based study of homocysteine, its determinants, and associations with disease. J Nutr. 2006;136(6 Suppl):1731s–1740s.
- Nygård O, Vollset SE, Refsum H, et al. Total plasma homocysteine and cardiovascular risk profile. The Hordaland Homocysteine Study. JAMA. 1995;274(19):1526–1533.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
- Han M, Li Q, Liu L, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens. 2019;37(12):2325–2332.
- Wang Y. Stage 1 hypertension and risk of cardiovascular disease mortality in United States adults with or without diabetes. J Hypertens. 2022;40(4):794–803.
- Kringeland E, Tell GS, Midtbø H, et al. Stage 1 hypertension, sex, and acute coronary syndromes during midlife: the Hordaland Health Study. Eur J Prev Cardiol. 2022;29(1):147–154.
- Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK biobank participants. BMJ. 2018;363:k4247.
- Omvik P. How smoking affects blood pressure. Blood Press. 1996;5(2):71–77.
- O'Meara JG, Kardia SL, Armon JJ, et al. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164(12):1313–1318.
- Yan Y, Li S, Liu Y, et al. Associations between life-course lipid trajectories and subclinical atherosclerosis in midlife. JAMA Netw Open. 2022;5(10):e2234862.
- Honigberg MC, Zekavat SM, Aragam K, et al. Long-term cardiovascular risk in women with hypertension during pregnancy. J Am Coll Cardiol. 2019;74(22):2743–2754.