Abstract
Purpose
Hypertension should be confirmed with the use of home BP measurement (HBPM) or 24h ambulatory BP measurement (ABPM). The aim of our study was to compare measurements obtained by OBPM, HBPM and ABPM in individuals with elevated OBPM participating in the population-based Swiss Longitudinal Cohort Study (SWICOS).
Material and Methods
Participants with OBPM ≥140/90 mmHg assessed their BP using HBPM and ABPM. The cut-off for hypertension was ≥135/85 mmHg for HBPM, ≥130/80 mmHg for ABPM. White-coat hypertension (WCH) was defined as normal HPBM and ABPM in participants not taking antihypertensive drugs. Uncontrolled hypertension was defined as hypertension in HBPM or ABPM despite antihypertensive treatment.
Results
Of 72 hypertensive subjects with office BP ≥140/90 mmHg and valid measurements of HBPM and ABPM, 39 were males (aged 62.8 ± 11.8y), 33 were females (aged 57.4 ± 14.2y). Hypertension was confirmed with HBPM and ABPM in 17 participants (24%), with ABPM only in 24 further participants (33%), and with HBPM only in 2 further participants (3%). Participants who had hypertension according to ABPM but not HBPM were younger (59 ± 11 y versus 67 ± 16 y; p < 0.001) and more frequently still working (83% versus 23%; p < 0.001). The prevalence of WCH was 28%. Among the 32 subjects taking antihypertensive drugs, uncontrolled hypertension was found in 49%.
Conclusion
This population-based study found a high prevalence of WCH and potential uncontrolled hypertension among individuals with elevated OBPM. This study, therefore, supports the ESH recommendations of complementing OBPM by ABPM or HBPM. The use of HBPM instead of ABPM for the confirmation of hypertension in individuals with elevated OBPM might lead to underdiagnosis and uncontrolled hypertension, in particular in the younger working population. In these individuals, this study suggests using ABPM instead of HBPM.
PLAIN LANGUAGE SUMMARY
What is already known?
Comparing blood pressure measurements in the doctor’s office or clinic (OBPM) with out-of-office measurements (either self-measurement at home (HBPM) or ambulatory over 24 hours during both day and night times (ABPM)) improves the accuracy of hypertension diagnosis.
Why was the study done?
This study was done to provide additional information by comparing HBPM and ABPM in individuals with elevated OPBMs (≥140/≥90mmHg), who participated in the Swiss Longitudinal Cohort Study (SWICOS)
What was found?
Our study confirmed differences between office and out-of-office measurements. In 60% of the study participants, ABPM or HBPM confirmed the elevated OBPM but only around half of these participants were treated with antihypertensive drugs. A high proportion of the participants (28%) had white coat hypertension.
What does this study add?
Our study adds to the literature already available on this issue by reporting on data obtained from a cohort of individuals living in a countryside area of Southern Switzerland.
This study also showed that HBPM might underestimate BP in the younger working population.
How might this impact on clinical practice?
The findings of this population-based study support the European Society of Hypertension recommendations for wider use of out-of-office blood pressure measurement for the confirmation of hypertension in individuals with elevated OBPM to avoid underdiagnosis and uncontrolled hypertension.
In the young working population, ABPM should be used instead of only HBPM to confirm hypertension.
Introduction
Accurate blood pressure (BP) measurement is essential for hypertension diagnosis, adequate hypertension control, prevention of adverse drug effects, and to avoid under- or over-treatment. The European Society of Hypertension (ESH) Working Group on BP Monitoring and Cardiovascular Variability recently published updated practice guidelines for office and out-of-office BP measurements [Citation1].
Previously it was considered that the repeated office BP measurement is the cornerstone of diagnostic approach to hypertension [Citation2,Citation3]. However, they also emphasise the importance of combining office BP measurements (OBPM) with out-of-office BP measurements, the latter obtained in the individual’s normal environment. Easy and reliable self-measurement of BP at the patient’s home allows BP monitoring over a long period of time, in either treated or untreated individuals [Citation4,Citation5]. The increasingly frequent combination of OBPM and out-of-office BP measurements has improved the accuracy of hypertension diagnosis and permitted the identification of specific BP phenotypes, such as sustained normotension and sustained hypertension when both office and out-of-office BP are normal or elevated, respectively, as well as white-coat- (WCH) or masked hypertension if there is a discrepancy between office and out-of-office BP values. These measurements are more closely associated with preclinical organ damage and cardiovascular events risk than office measurements [Citation6,Citation7]. This also improves the diagnosis and BP control of hypertensive patients.
Currently, out-of-office BP monitoring can be obtained through either self-BP measurements at home (home BP monitoring, HBPM) or 24h-ambulatory BP monitoring (ABPM). HBPM in the patient’s normal environment can provide multiple BP values, is patient-friendly, easy to perform, inexpensive and recommended as the best method for long-term follow-up of treated hypertensive subjects [Citation1,Citation4]. ABPM offers multiple BP values over 24 h taken during both day and night times, and is reported in guidelines as the most accurate method for hypertension diagnosis and cardiovascular risk stratification [Citation18]. However, it may be of limited availability and can be uncomfortable. While there are several studies on either office, home or ambulatory BP measurement, limited evidence is available on the comparison of these different methods in population-based cohorts [Citation9–11].
Our study aimed to provide additional information on this issue by comparing BP measurements obtained at home and ambulatory in individuals with elevated OBPM participating in the Swiss Longitudinal Cohort Study (SWICOS). We further aimed to evaluate the extent of hypertension-mediated organ damage (HMOD) using central hemodynamic parameters.
Methods
Study design and participants
The protocol of the prospective, population-based SWICOS study has been previously published [Citation12]. Participants were mostly recruited in Cama/Lostallo (GR), two Swiss municipalities. All residents aged 18 years and older were eligible for participation. There were no exclusion criteria. All participants provided written informed consent. The study was approved by the ‘Ethikkommission Nordwest- und Zentralschweiz (EKNZ)’ (approval no. EKNZ 2014-209) and the ‘Kantonale Ethikkommission Kanton Zürich’ (approval no. 2014-0265) in August 2014, and the study complied with the Declaration of Helsinki. It is registered at ClinicalTrials.gov (NCT02282748).
Measurements
All participants completed a questionnaire on medical history, daily life habits, and prescribed medication. Participants also underwent a physical examination, including OBPM. OBPM was recorded using an automated oscillometric upper-arm cuff device (OMRON 705IT, Omron Corporation, Shiokoji Horikawa, Shimogyo-ku, Kyoto 600–8530 Japan), validated according to an established protocol [Citation13]. All participants were in rest for a least 10 min before the first measurement. BP was measured twice on each arm, with a 2 min interval. The mean value of those four measurements was used for the analyses.
Individuals with OBPM ≥140 and/or ≥90mmHg were invited to also assess their BP through HBPM and ABPM. Both HBPM and ABPM were performed according to ESH practice guidelines [Citation1,Citation3,Citation4]. For HBPM, all participants received an automated oscillometric upper-arm cuff device (OMRON IM HEM 7322 U) and were instructed in the proper use of the device. In the present study, we used the average of all BP measurements taken over at least 5 days (two in the morning and two in the evening), excluding the first day. Twenty fourhour ABPM was performed using an automated and validated oscillometric device (Arteriograph 24, TensioMed Ltd., Budapest, Hungary) [Citation14,Citation15]. Only recordings with at least 20 valid readings during the daytime and at least 7 readings during the night-time were included in the study data analysis.
For the evaluation of HMOD, the following central hemodynamic parameters were measured. Pulse wave velocity (PWV) was assessed after the completion of OBP measurements at baseline: pulse wave velocity (PWV) and central aortic BP were measured by a validated operator-independent, non-invasive device (Arteriograph®; Tensiomed Ltd., Budapest, Hungary) based on a validated oscillometric occlusive technique (Arteriograph, TensioMed Ltd., Budapest, Hungary) [Citation14]. After 5 min of rest, supine brachial systolic and diastolic BP, heart rate and central hemodynamics parameters were simultaneously obtained. The arteriograph software estimates PWV by considering the timing of wave reflections and specifically the time interval between the peaks of the ejected (first) and reflected (second) systolic wave in relation to the jug between both waves. To ensure the quality of measured pulse wave velocity, only measurements of aortic PWV with a standard deviation of beat-to-beat variation ≤1.0 m/sec were included.
Definitions
The ESH/ESC definition of hypertension according to the levels of office, ambulatory and home BP is as follows: conventional office BP ≥140 and/or ≥90 mmHg; ambulatory BP daytime or awake mean ≥135 and/or ≥85 mmHg, night-time or asleep mean ≥120 and/or ≥70 mmHg; 24h mean ≥130 and/or ≥80 mmHg; home BP mean ≥135 and/or ≥85 mmHg. WCH was defined as normal out-of-office BP in untreated individuals with OBPM ≥140 and/or ≥90 mmHg. Sustained hypertension was defined as confirmation of elevated OBPM by both ABPM and HBPM. Uncontrolled hypertension was defined as hypertension in HBPM or ABPM despite a prescription of antihypertensive drugs.
Cardiovascular risk assessment
Further, the cardiovascular (CV) risk was calculated for each participant according to the ESH/ESC recommendation for assessing the 10-year risk of CV disease using the SCORE2 and SCORE2OP algorithms (www.heartscore.org). The SCORE2 tool includes the following parameters: age, sex, systolic BP, total cholesterol, LDL and smoking. Cardiovascular risk was divided into three score categories: low/moderate risk below 5%, high risk 5–10% and very high risk 10% and above [Citation16].
Statistical analysis
Descriptive statistics were used to determine the baseline characteristics of the participants. The normality of the continuous variables distribution was analysed using either the Shapiro-Wilk or Kolmogorov-Smirnov test. Normally distributed variables are presented as means with ± 1 standard deviation (SD) and non-normally distributed variables are expressed as medians and interquartile ranges. Categorical variables are presented as percentages. Comparison of the BP measurement values obtained with the above three BPM methods was performed using one simple Student t test, ANOVA with adequate correction of the minimum statistical significance level or the Kruskal-Wallis test as appropriate. To assess which covariates are related to sustained hypertension a univariate, as well as multivariate regression analyses including age, gender, smoking, overweight were performed. The Results are presented as odds ratio (OR) and 95% confidence interval (95% CI). All analyses were performed using IBM SPSS Statistics software (Version 26, IBM Corp., Armonk, NY).
Results
Among the 474 adult SWICOS participants (206 males and 268 females), 113 (23.8%) had systolic OBPM ≥140 mmHg and/or diastolic OBPM ≥90 mmHg. Of these, 15 participants refused to perform HBPM and/or ABPM resulting in 98 participants who underwent HBPM and/or ABPM. All 98 participants had HBPM (95 with utilisable readings) and 81 ABPM (with at least 74 utilisable readings). Overall, 72 subjects had utilisable HBPM and ABPM and were included in this analysis. Among these 72 participants, 17 (24%) had high BP in both out-of-office measurements (in HBPM and in ABPM). Partial high BP was seen either in ABPM or in HBPM in 24 (33%) and in 2 (3%), respectively. Normal BP in both HBPM and ABPM was found in 29 (40%) participants.
The BP values measured with the three methods were significantly different. Mean systolic OBPM was highest (151.7 ± 15.5 mmHg) and was significantly higher than daytime ABPM (136.9 ± 13.5 mmHg) or HBPM (130.0 ± 13.5 mmHg) (p < 0.001 for both). The systolic 24-hour ABPM was also significantly higher compared to systolic HBPM (p < 0.001) (). Diastolic BP was also the highest with OBPM (89.3 ± 8.0 mmHg) and significantly different compared to ABPM daytime (80.8 ± 11.2 mmHg) and HBPM (81.6 ± 6.6 mmHg) (both p < 0.001). The lowest values of diastolic BP were found in ABPM over 24 h and at night-time (). The central pulse pressure was significantly higher in participants with sustained hypertension compared to those with partial hypertension and participants with normal BP (). For sustained hypertension age was significant in univariate (OR per additional year 1.07 (95%CI 1.01–1.12; p = 0.014), as well as an independent predictor of it (OR per additional year 1.09 (95%CI 1.02–1.15; p = 0.007)) after adjustment for sex, smoking and overweight. None of other covariates was significant predictor of sustained hypertension, which could be due to low numbers.
Table 1. Blood pressure and central hemodynamic values of SWICOS-cohort participants with office blood pressure ≥140 and/or ≥90mmHg at baseline) according to out-of-office BP measurements.
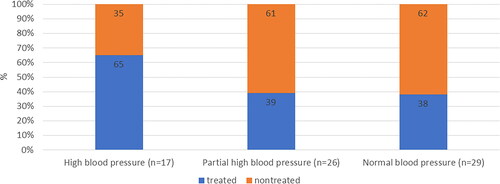
Among the 72 study participants, 29 (40%) had normal BP as measured by ABPM and HBPM and for 43 (60%) elevated OBPM was confirmed by ABPM and/or HBPM. Of all 72 study participants, 32 (44%) were on a prescription of antihypertensive drugs. Among the 40 participants who were not taking any antihypertensive drugs, 11 (28%) had normal ABPM and HPBM, thus having WCH (). Among the 32 participants taking antihypertensive drugs, only 10 participants (31%) had controlled hypertension (i.e. normal ABPM and HBPM). Among the 43 participants with confirmed hypertension, 22 (51%) were not treated with antihypertensive drugs and 21 (49%) were on a prescription of antihypertensive drugs.
Figure 1. Antihypertensive therapy in SWICOS participants with OBPM ≥140/90 mmHg according to out-of-office measurements.
High blood pressure -> by HBPM: SBP ≥135mmHg and/or DBP ≥85mmHg AND by ABPM: SBP ≥130mmHg and/or DBP ≥80mmHg; Partial high blood pressure -> by HBPM: SBP ≥135mmHg and/or DBP ≥85mmHg OR by ABPM: SBP ≥130mmHg and/or DBP ≥80mmHg; Normal blood pressure -> by HBPM: SBP <135mmHg and DBP <85mmHg AND by ABPM: SBP <130mmHg and DBP <80mmHg.
The baseline characteristics of the participants according to BP measurements are shown in . Participants with sustained hypertension compared with normotensive participants were 10 years older, had higher BMI, were less likely to work, were frequently treated with lipid-lowering drugs and antidiabetics and had more than a two-fold higher risk score for premature CV events. They also had higher HbA1c and creatinine than normotensive subjects (). Subjects with partial hypertension were the same age as normotensive, more frequently males, had a higher BMI and were more often actively working ().
Table 2. Baseline characteristics of SWICOS cohort participants (with office blood pressure ≥140 and/or ≥90mmHg) according to out-of-office BP measurements.
The subjects who had hypertension according to ABPM but not HBPM (n = 24) were 10 years younger (59 ± 11 y versus 67 ± 16 y; p < 0.001) and frequently still working (83% versus 23%; p < 0.001) compared with those with concordance between ABPM and HBPM (n = 17).
Subjects, who were still working compared to those who were not-working had higher diastolic BP during daytime 83.9 ± 11.4 mmHg versus 75.6 ± 9.1 mmHg (p = 0.002) and lower systolic BP during night time 116.6 ± 16.9 mmHg versus 126.3 ± 19.7 mmHg (p = 0.024).
Out of 29 subjects with normotensive values in out-of-office measurement, 13 (45%) had a high or very high risk of a premature cardiovascular event, whereas 13 (77%) out of 17 with sustained hypertension had a high/very high risk (p = 0.036). Aortic pulse pressure ≥60 mmHg, a sign of HMOD, was found in 65% of subjects with sustained or partial hypertension and in 25% of subjects with normal BP (p = 0.013). Aortic pulse wave velocity ≥10 m/s was detected in 41% of the hypertensive subjects and in 29% of normotensive (p = 0.52).
Discussion
The results of this analysis of out-of-office BP measurements in participants of the population-based SWICOS study with high OBPM at baseline could be summarised as follows: (a) elevated OBPM was not confirmed by ABPM and HBPM in a relevant proportion of 40% of all study participants; (b) a high proportion of the participants (28%) had WCH; (c) in 60% of study participants, elevated OBPM was confirmed by ABPM or HBPM and only around half of these participants were treated with antihypertensive drugs, suggesting a high proportion of potential uncontrolled hypertension; and (d) the problem of uncontrolled hypertension is underscored by the finding that BP was controlled in only 31% of the subjects on drug treatment.
Our findings were consistent with previous studies. Previous studies proved that BP values obtained by OBPM are up to 15 mmHg higher for systolic BP and 10 mmHg higher for diastolic BP than BP values measured by ABPM and HBPM [Citation17]. Our study confirmed that differences between office and out-of-office measurements may be that high. The Swiss population-based study on Genes in Hypertension in 2015 found significant heritability for OBPM and ABPM, justifying the ongoing search for genetic determinants of BP [Citation18].
The prevalence of WCH found in our study was high but corresponded with previous findings [Citation19,Citation20]. The probability of being diagnosed with sustained hypertension using ABPM or HBPM in persons with elevated OBPM has been reported to range between 35–95%. In our study, the probability was 60% and corresponded to these previous findings.
This study showed that there are not only relevant differences between office and out-of-office BP measurements but that there are also relevant differences between the two out-of-office BP measurements (i.e. ABPM and HBPM) [Citation21]. ABPM is usually performed during routine daily activities and at night-time, whereas HBPM is usually performed at rest at home. Our finding that BP might be underestimated by HBPM in the young working population is therefore plausible and it is relevant. In the authors’ opinion, HBPM, as the only out-of-office BP measurement method, should probably not be recommended for younger working patients to exclude a hypertension diagnosis, because diastolic BP during working may be relevantly underestimated.
The development of new technology, such as automated, smartphone application app-assisted HBPM might improve reliability and widespread use of HBPM. However, the AMUSE-BP study demonstrated that app-assisted HBPM substantially overestimates 24-h ABPM. However, as app-assisted HBPM showed sensitivity and negative predictive value for diagnosing sustained and masked hypertension it could be used as a screening test for these diagnoses [Citation22].
In accordance with current guidelines, our study underlines the importance of confirming suspected hypertension based on OBPM by out-of-office BP measurements. Current guidelines favour ABPM over HBPM for this purpose [Citation1,Citation20]. Both methods have their advantages and disadvantages. Both methods may be used for hypertension diagnosis, treatment titration and long-term follow-up, but ABPM is better suited for the initial evaluation and HBPM for the long-term follow-up of treated subjects [Citation1,Citation4]. A new study showed the modest superiority of home BP compared to ambulatory BP to predict cardiovascular prognosis [Citation23]. Ideally, if available and feasible, both ABPM and HBPM should be used, as they may provide complementary information [Citation1,Citation24]. For example, different hypertension phenotypes may be determined based on the comparison between the in-the-office and out-of-office measurements, namely WCH and sustained hypertension. It has been showed that WCH exhibits a cardiovascular risk greater than that of normotensive controls [Citation25], even without organ damage [Citation26].
The identification of these phenotypes may help to optimise hypertension therapy and to avoid over- and undertreatment.
ABPM and HBPM also provide prognostic information on cardiovascular mortality and morbidity above and beyond that of OBPM in a general Western population [Citation9,Citation27,Citation28]. When comparing ABPM and HBPM for the prediction of cardiovascular events or mortality, in a systematic review Shimbo et al. showed that both methods are similar [Citation29]. In our population-based study, more than half of the hypertensive participants were at high or very high cardiovascular risk of a premature cardiovascular event within 10 years. Implementing out-of-office BP measurement might help to reduce the cardiovascular risk level over time, in spite of comorbidities [Citation30]. A meta-analysis showed that in participants without previous cardiovascular disease at baseline, the incidence rate for developing a major cardiovascular event per 1000 person-years was 31.9%, and in participants with previous cardiovascular disease the incidence was 39.7% [Citation31]. Given that a reduction of 5 mmHg of systolic BP reduces the risk of major cardiovascular events by about 10% [Citation31], reliable strategies to detect treatment-induced BP changes are necessary, and this study provides evidence to support the use of out-of-office BP in the clinical setting.
Approximately a quarter of the participants with normal BP measurements in ABPM and HBPM had elevated aortic pulse pressure and/or pulse wave velocity as a sign of potential HMOD. Our results, therefore, underline that the measurement of central hemodynamics may provide additional information to complement regular BP measurement. Potentially, subjects with abnormal central hemodynamics despite normal ABPM and HBPM might benefit from tighter cardiovascular risk prevention.
Limitations and strengths
One limitation of our study is the small number of participants. Another limitation might be selection bias, which could not be completely excluded given the non-randomly selected study population in the two municipalities. However, comparison of our findings with those from previous studies showed a high level of agreement. Furthermore, demographic data of the adult study population (e.g. age and sex distribution, prevalence of cardiovascular risk factors) was similar to the Swiss population according to Swiss federal statistics [Citation32]. We therefore think that the generalisability of our findings is not limited to a high degree. Another limitation of our study results from the inclusion of participants with elevated OBPM; thus, this study is not suited to evaluate the usefulness of HBPM for the detection of masked hypertension.
To the best of our knowledge, this is the first study to include all three BP measurement methods which is a strength of this study. In spite of the above-mentioned limitations, our data provide the first comparative evaluation of how to implement OBPM, ABPM and HBPM in the real world to favour a reliable diagnosis and treatment of hypertension in daily clinical practice. Our study adds to the literature already available on this issue by reporting on data obtained from a cohort of individuals living in a countryside area of Southern Switzerland.
Conclusions
In this population-based cohort of participants with OBPM ≥140/90 mmHg, BP measurement values were significantly different between OBPM, ABPM and HBPM. In general, ABPM and HBPM provided lower BP values than OBPM. WCH had a high prevalence of 28% among untreated participants. Well-controlled hypertension was found in only 26% of treated participants, whereas sustained hypertension was confirmed by ABPM and/or HBPM in a high percentage of the participants. Thus, our study revealed a high risk of potential uncontrolled hypertension. This study also showed that HBPM may underestimate BP in the younger working population suggesting using ABPM instead of HBPM in these individuals. The findings of this study support the ESH recommendations of complementing OBPM using HBPM or ABPM given the high prevalence of WCH and undertreatment.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Stergiou GS, Palatini P, Parati G, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1–10.
- Whelton PK, Chen J, Krousel-Wood M. Lessons learned from systolic blood pressure intervention trial. Curr Opin Cardiol. 2017;32(4):1–10. doi: 10.1097/HCO.0000000000000396.
- Parati G, Agostoni P, Basnyat B, et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the european society of cardiology, the council on hypertension of the European society of cardiology, the European society of hypertension, the international society of Mountain medicine, the Italian society of hypertension and the Italian society of Mountain medicine. Eur Heart J. 2018;39(17):1546–1554. doi: 10.1093/eurheartj/ehx720.
- Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the working group on blood pressure monitoring and cardiovascular variability of the European society of hypertension. J Hypertens. 2021;39(9):1742–1767. doi: 10.1097/HJH.0000000000002922.
- Iemitsu M, Maeda S, Otsuki T, et al. Arterial stiffness, physical activity, and atrial natriuretic peptide gene polymorphism in older subjects. Hypertens Res. 2008;31(4):767–774. doi: 10.1291/hypres.31.767.
- O’Brien E, Parati G, Stergiou G. Ambulatory blood pressure measurement: what is the international consensus? Hypertension. 2013;62(6):988–994. doi: 10.1161/HYPERTENSIONAHA.113.02148.
- Parati G, Stergiou GS, Asmar R, et al. European society of hypertension guidelines for blood pressure monitoring at home: a summary report of the second international consensus conference on home blood pressure monitoring. J Hypertens. 2008;26(8):1505–1526. doi: 10.1097/HJH.0b013e328308da66.
- Parati G, Stergiou G, O’Brien E, et al. European society of hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32(7):1359–1366. doi: 10.1097/HJH.0000000000000221.
- Hansen TW, Jeppesen J, Rasmussen S, et al. Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study. Am J Hypertens. 2006;19(3):243–250. doi: 10.1016/j.amjhyper.2005.09.018.
- Myers MG, Kaczorowski J. Are automated office blood pressure readings more variable than home readings? Hypertension. 2020;75(5):1179–1183. doi: 10.1161/HYPERTENSIONAHA.119.14171.
- Drawz PE, Abdalla M, Rahman M. Blood pressure measurement: clinic, home, ambulatory, and beyond. Am J Kidney Dis. 2012;60(3):449–462. doi: 10.1053/j.ajkd.2012.01.026.
- Schoenenberger AW, Muggli F, Parati G, et al. Protocol of the Swiss longitudinal cohort study (SWICOS) in rural Switzerland. BMJ Open. 2016;6(11):e013280. doi: 10.1136/bmjopen-2016-013280.
- Topouchian J, Agnoletti D, Blacher J, et al. Validation of four devices: Omron M6 comfort, Omron HEM-7420, withings BP-800, and polygreen KP-7670 for home blood pressure measurement according to the European society of hypertension international protocol. Vasc Health Risk Manag. 2014;10:33–44. doi: 10.2147/VHRM.S53968.
- Horvath IG, Nemeth A, Lenkey Z, et al. Invasive validation of a new oscillometric device (arteriograph) for measuring augmentation index, central blood pressure and aortic pulse wave velocity. J Hypertens. 2010;28(10):2068–2075. doi: 10.1097/HJH.0b013e32833c8a1a.
- Baulmann J, Schillings U, Rickert S, et al. A new oscillometric method for assessment of arterial stiffness: comparison with tonometric and piezo-electronic methods. J Hypertens. 2008;26(3):523–528. doi: 10.1097/HJH.0b013e3282f314f7.
- Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–3337. doi: 10.1093/eurheartj/ehab484.
- Pappaccogli M, Di Monaco S, Perlo E, et al. Comparison of automated office blood pressure with office and out-off-office measurement techniques. Hypertension. 2019;73(2):481–490. doi: 10.1161/HYPERTENSIONAHA.118.12079.
- Alwan H, Ehret G, Ponte B, et al. Heritability of ambulatory and office blood pressure in the Swiss population. J Hypertens. 2015;33(10):2061–2067. doi: 10.1097/HJH.0000000000000681.
- de la Sierra A, Vinyoles E, Banegas JR, et al. Prevalence and clinical characteristics of white-coat hypertension based on different definition criteria in untreated and treated patients. J Hypertens. 2017;35(12):2388–2394. doi: 10.1097/HJH.0000000000001493.
- Karnjanapiboonwong A, Anothaisintawee T, Chaikledkaew U, et al. Diagnostic performance of clinic and home blood pressure measurements compared with ambulatory blood pressure: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20(1):491. doi: 10.1186/s12872-020-01736-2.
- Ntineri A, Niiranen TJ, McManus RJ, et al. Ambulatory versus home blood pressure monitoring: frequency and determinants of blood pressure difference and diagnostic disagreement. J Hypertens. 2019;37(10):1974–1981. doi: 10.1097/HJH.0000000000002148.
- Groenland EH, Vendeville JAC, Bemelmans RHH, et al. Smartphone application-assisted home blood pressure monitoring compared with office and ambulatory blood pressure monitoring in patients with hypertension: the AMUSE-BP study. Hypertension. 2022;79(10):2373–2382. doi: 10.1161/HYPERTENSIONAHA.122.19685.
- Narita K, Hoshide S, Kario K. Association of home and ambulatory blood pressure with cardiovascular prognosis in practice hypertensive outpatients. Hypertension. 2023;80(2):451–459. doi: 10.1161/HYPERTENSIONAHA.122.20178.
- Townsend RR. Out-of-office blood pressure monitoring: a comparison of ambulatory blood pressure monitoring and home (self) monitoring of blood pressure. Hypertension. 2020;76(6):1667–1673. doi: 10.1161/HYPERTENSIONAHA.120.14650.
- Briasoulis A, Androulakis E. Is white-coat hypertension associated with increased cardiovascular and mortality risk? Reply. J Hypertens. 2016;34(8):1658–1659. doi: 10.1097/HJH.0000000000000984.
- Mancia G, Facchetti R, Quarti-Trevano F, et al. Antihypertensive drug treatment in white-coat hypertension: data from the plaque HYpertension lipid-lowering Italian study. J Hypertens. 2022;40(10):1909–1917. doi: 10.1097/HJH.0000000000003176.
- Banegas JR, Ruilope LM, Williams B. Ambulatory blood pressure and mortality. N Engl J Med. 2018;379(13):1287–1288. doi: 10.1056/NEJMc1809851.
- Yang WY, Melgarejo JD, Thijs L, et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA. 2019;322(5):409–420. doi: 10.1001/jama.2019.9811.
- Shimbo D, Abdalla M, Falzon L, et al. Studies comparing ambulatory blood pressure and home blood pressure on cardiovascular disease and mortality outcomes: a systematic review. J Am Soc Hypertens. 2016;10(3):224–234 e17. doi: 10.1016/j.jash.2015.12.013.
- Sheppard JP, Nicholson BD, Lee J, et al. Association between blood pressure control and coronavirus disease 2019 outcomes in 45418 symptomatic patients with hypertension: an observational cohort study. Hypertension. 2021;77(3):846–855. doi: 10.1161/HYPERTENSIONAHA.120.16472.
- Blood Pressure Lowering Treatment Trialists C. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–1636.
- BFS. BfS. Schweizerische Gesundheitsbefragung 2017. Neuchâtel: BFS; 2018.
