Abstract
Background
This study aims to determine the validity of self-reported hypertension and identify factors affecting the disagreement between self-reported hypertension and objective measures of blood pressure among adults in Vietnam.
Materials and Methods
A total of 4,219 people aged 18 and older reported their hypertension status and had their blood pressure measured. The inter-reliability between self-reported and measured hypertension was assessed using Cohen’s Kappa statistics. Univariate and multivariate logistic regressions were used to examine the affecting factors of disagreement.
Result
Self-reported hypertension prevalence was 13.2% (557/4,219), while measured hypertension was 20.9% (881/4,219). An agreement between self-reported and measured data was moderate for the hypertension of participants (κ = 0.39, 95% CI 0.36-0.43). Self-reported hypertension showed high specificity (93.9%) (95% CI 93.0-94.7) but low sensitivity (40.1%; 95 CI 36.8-43.4). The percentage of disagreement in hypertension (number of false positives and false negatives between self-reported and measured data) among adults in Vietnam was 17.3%.
Conclusion
Our findings showed there was a high disagreement percentage of hypertension between self-reported and measured data. This is the first report of this issue to warn of health risks if high blood pressure is not detected early. The disagreement of hypertension was observed more frequently in men, people older than 40, minority ethnic groups, farmers, and people with a BMI greater than 25 kg/m2.
Plain Language Summary
Researchers often ask people to answer questions about their own health problems, such as high blood pressure, to study the effects of these conditions. People often provide self-reported information in response to this inquiry. However, this information might not be accurate. Therefore, it is preferable to use biological data, which involves having blood pressure checked by a machine.
In this study, the self-reported hypertension of adults in Vietnam was compared to measured blood pressure data. We found that, whereas only 13.2% of respondents reported having high blood pressure, the measured blood pressure by machine revealed that 20.9% of respondents had the condition. The study also discovered that some elements, including age, gender, ethnicity, BMI, smoking status, and drinking, were associated with the discrepancy between self-reported and measured hypertension among participants.
This study demonstrates that it is unreliable to estimate the prevalence of high blood pressure in Vietnam using self-reported data. According to the study, including biological tests in social surveys can increase data accuracy and clarify societal health disparities. The study suggests that to avoid and identify these health issues early, people should obtain more health education and undergo routine physicals.
Introduction
Hypertension (HTN) characterized by persistently high blood pressure, poses a significant public health challenge as it substantially elevates the risks of stroke, myocardial infarction, heart failure, and renal failure [Citation1–4]. Worldwide, it is estimated that about 1.28 billion adults aged 30 to 79 years have been diagnosed with HTN, and two-thirds of those cases are reported in low-and middle-income countries [Citation1]. Furthermore, even though HTN is straightforward to detect and control with low-cost medications, approximately 580 million individuals with HTN (46%) are unaware of their condition because it has never been officially diagnosed [Citation5]. HTN stands as a primary contributor to premature mortality, and it is an integral part of the global targets to reduce the prevalence of non-communicable diseases, to achieve a 33% reduction between 2010 and 2030 [Citation1, Citation6].
International investigations showed that regularly checking blood pressure is the only way to diagnose and control hypertension early, especially self-measured, which is better associated with the appearance of complications [Citation7–9]. However, many people continue to have unrecognized or untreated hypertension, which leads to increased mortality from stroke and ischaemic heart disease [Citation10]. In Vietnam, recent studies revealed that hypertension among adults is becoming a public health issue with a prevalence of 21.1% based on a systematic review, and 18.4% based on a national survey [Citation11], and a high percentage of people are unaware that they have hypertension, resulting in a high proportion of untreated and uncontrolled hypertension cases [Citation12, Citation13]. Especially, self-control of blood pressure is popular in Vietnam today home blood pressure monitoring is very popular in Vietnam [Citation14]. This can lead to misdiagnosis of blood pressure, leading to unexpected health, mental, and economic risks to the population. Some previous studies revealed the disagreement between self-reported and objective measures or biomedical measurements of hypertension in different countries [Citation8, Citation15–17]. However, there is a substantial knowledge gap in the accuracy of self-reported hypertension in Vietnam. The purpose of the current study was to evaluate the validity of self-reported hypertension among people in Vietnam and pinpoint the variables influencing discrepancies between self-reported and measured hypertension.
Materials and methods
Data source
A national survey on non-communicable diseases, with a sample size of 4,219 respondents. Participants of this survey were: (1) Vietnamese citizens, age 18 and older; (2) have a permanent address in Vietnam; (3) be at home throughout the survey; and (4) not have any mental health issues that would have prevented them from responding to the questions.
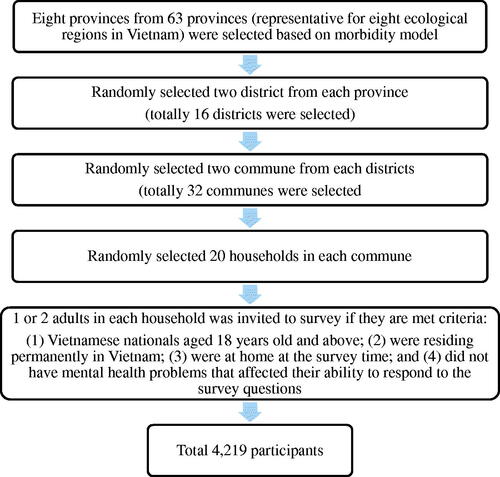
The survey was carried out and was conducted from 2013 to 2016 in eight provinces, representing the eight ecological areas of Vietnam. A multiple-stage stratified cluster sampling and a simple random sampling were used to recruit participants for the study ().
Data collection and measurements
An in-person interview and a hypertension test were the two information sources gathered: blood pressure examined by healthcare workers at the Community Health Station and self-reported hypertension of interviewees.
The “Do you have high blood pressure?’’ item on the questionnaire enabled the gathering of self-reported data on hypertension. Either yes or no is the appropriate response.
Healthcare workers working in the Community Health Station at the commune level were trained on how to use an electronic monitor (Omron model HEM 711), all of the machines were validated by manufacturers) and recorded the result. The average of three blood pressure results was used to assess the participant's hypertension condition. Hypertension was defined as having an average systolic blood pressure of at least 140 mmHg and/or an average diastolic blood pressure of at least 90 mmHg.
Measurements
Dependent variables
Disagreement (false positives and/or false negatives) between self-reported HTN and objectively measured hypertension.
Independent variables
Demographic variables included (1) sex (male and female); (2) age groups (i.e., 18–39, 40–59, and 60+); (3) educational level (primary or less, secondary, high school, and university/college); (4) occupation (senior officials and professionals, elementary occupations, farmers and others); and (5) economic status of the household, categorically measured based on an asset-based wealth index of “lower income”, “middle income”, and “higher income” as classified by local authorities. Behavioral risk factors for hypertension were also examined, including (1) smoking status (smoker and nonsmoker); (2) drinking status, categorized as a drinker (consumed at least one standard drink of alcohol in the past 30 days) and nondrinker; and (3) overweight status, categorized overweight for those who had a body mass index (BMI) equal to or greater than 25 kg/m2 and non-overweight for those with a BMI 25 kg/m2.
Data analysis
Means and proportions were used as descriptive statistics for qualitative and quantitative variables. The chi-square test was used to test the difference between the two proportions.
Sensitivity and specificity tests were used to evaluate the accuracy of self-reported hypertension. The formulas for sensitivity and specificity were (true positives)/(true positives plus false negatives) and (true negatives)/(true negatives plus false positives), respectively. The definitions of the positive and negative likelihood ratios were respectively given as sensitivity/(1-specificity) and (1-sensitivity)/specificity. Definitions of the positive and negative predictive values were, respectively, ‘‘true positives” (true positives) or “true positives plus false positives) and “true negatives” (true negatives plus false negatives).
Kappa statistics were used to assess the agreement between self-reported and measured blood pressure values. The κ coefficient (kappa coefficient) took into account the agreement occurring by chance, and since it is a more robust measure than simple percent agreement between self-reported questionnaire data and measurement data. The κ coefficient was divided into six categories, with values 0 indicating no agreement, from 0.01 to 0.20 as none to a slight agreement, 0.21 to 0.40 as fair agreement, 0.41 to 0.60 as moderate agreement, 0.61 to 0.80 as substantial agreement, and from 0.81 to 1.00 as almost perfect agreement.
Univariate and multivariate logistic regression were used to examine the role of demographic characteristics in the disagreement (false positives and/or false negatives) between self-reported and measured hypertension. A two-sided alpha level with p < 0.05 was considered statistically significant. All analyses used Stata version 14.0 (Stata Corp., TX, USA).
Result
A total of 4,219 adults participated in the study. The proportion of people from 18 to 39 years old, from 40 to 59 years old, and 60 years of age and above was 40.4%, 42.5%, and 17.0%, respectively, with a mean age of 44.9 years. The proportion of women was higher than that of men (54.7% vs. 45.3%). Over five in six participants were currently married (85%). About three-quarters of participants (75.6%) had an education level of secondary school or less, 17.5% had received a high school degree, and only 6.9% of them had earned a college degree or higher. More than half of the participants were farmers (63.6%). In terms of health behaviors, 22.5% were smokers, and 77.5% were non-smokers. About 29.1% were drinkers. Most participants had a BMI under 25 (91.8%). Half of the participants had lower incomes (50.5%).
presents the prevalence of hypertension by some sociodemographic factors, self-reported hypertension status, and measured hypertension status. A total of 557 participants (13.2%) reported having hypertension, and 881 (20.9%) were confirmed to have hypertension based on their measured blood pressure. Those with self-reported hypertension were more likely to be single, older, overweight or obese, have a lower educational level, and have a more professional occupation (p < 0.001). Similarly, those with measured hypertension were more likely to be male, were older, overweight or obese, had a lower educational level, and had a more professional occupation (p < 0.001). Additionally, being male and an ethnic minority was also associated with having measured hypertension (p < 0.001).
Table 1. Characteristics of respondents associated with self-reported and measured hypertension
presents the accuracy parameters of the self-reported hypertension status and the distribution of the accurate reports in the entire sample. Self-reported hypertension among Vietnamese adults had low sensitivities (40.1%) but high specificities that exceeded 90%.
Table 2. Validity of self-reported hypertension
reports odds ratios (ORs) and 95%CI from the multiple logistic regression analysis of relationships between the disagreement (positives and false negatives) and socio-demographic characteristics of participants. After adjusting for other factors in the model, gender, age, ethnicity, occupation, and BMI were significantly associated with disagreement. The results further confirmed that individuals aged ≥40 years were strongly and independently associated with having more disagreement between self-reported and measured hypertension: compared to individuals aged 18 to 39, the odds of disagreement are 60% higher for individuals aged 40 to 59 and 143% higher for those aged 60 or older. Individuals of the ethnic minority were more likely to have disagreement hypertension results than those of Kinh ethnicity (OR = 1.84, 95% CI: 1.41-2.41).
Table 3. Univariate and multivariate associations of disagreement between self-reported and measured hypertension
Working as farmers had higher odds of disagreement than those who worked as senior officials and professionals (OR = 1.58, 95% CI: 1.19–2.09). Overweight individuals are also more likely to have different hypertension statuses based on their self-reported and measured blood pressure results (OR = 1.58, 95% CI: 1.21-2.06). Female participants were less likely to have disagreement results than male participants (OR = 0.76; 95% CI 0.61-0.94).
Discussion
To the best of our knowledge, we are the first to analyze the accuracy of self-reported hypertension among adults in Vietnam with nationwide representatives. The self-reported prevalence of hypertension among participants was 13.2%, and after taking measurements of blood pressure, the prevalence was higher, at 20.9%. Our study adds to the evidence that the prevalence of hypertension by measure is higher than self-reported, which confirms previous findings in the literature on the accuracy of self-reported studies [Citation18]. The prevalence of hypertension by measure is also consistent with other studies in Vietnam [Citation12, Citation13, Citation19, Citation20]. Gender, age, occupation, education, and BMI were associated with both self-reported and measured hypertension. The difference between the prevalence of self-reported hypertension and measured hypertension was 7.7%.
In this study, we have measured the level of overall agreement between self-reported information on hypertension and measurement data, considered the gold standard for validation. Our study’s finding shows that the sensitivity of self-reported data for hypertension among Vietnamese adults was low, at 40.1%, indicating that approximately only 40% of true cases were detected by self-report; yet specificity was very high (93.9%), indicating that most people who self-reported they did not have current hypertension were found to not have hypertension by measured data, and moderate kappa coefficient (κ = 0.41). This trend, where lower sensitivity of self-reported hypertension accompanies higher specificity of such self-reports, is consistent with previous studies from other countries such as Korea, China, India, South Africa, and Ghana. Nevertheless, there are important differences. The 40.1% sensitivity of self-reported hypertension in this study is lower than that reported in Korea (73%) [Citation16], China (56.3%) [Citation21], and Iran (75.5%) [Citation8], but higher than in India (22.2%), South Africa (31.4%), and Ghana (13.7%) [Citation22]. Our study contributes to the existing idea that the validity of self-reported information depends on the quality of health services [Citation8]. The low sensitivity shows that a high percentage of people are not cognizant of their hypertension condition. This could be because people forgot or never had a diagnosis of hypertension. In Vietnam, only 37% of people hold wage jobs [Citation23], these people have medical examinations yearly according to the low but not sure for the others. Moreover, Vietnamese people prefer self-medication because the medicine can be legally and readily obtained at a lower cost compared to a hospital visit [Citation24]. This could have resulted in a low level of blood pressure screening and asymptomatic hypertension in the early phase that could not be identified. Other reasons, such as the failure of healthcare personnel to communicate with patients or the poor recall of participants, may also affect the accuracy of self-reported hypertension.
In terms of socio-demographic correlates of disagreement in self-reported hypertension among Vietnamese adults, our multiple logistic regression analysis shows that socio-demographic and behavioral factors are more likely to be significantly related to the accuracy of self-reported hypertension. There was no statistically significant difference in the accuracy of self-reported hypertension by marital status, education, income, smoking, or drinking; however, disagreement in self-reported hypertension was found to be associated with gender, age, ethnicity, occupation, and BMI. In our study, disagreement was more common in males than females, and in overweight individuals (BMI > 25) compared to non-overweight individuals, which is in line with other studies in Korea [Citation16], China [Citation21], and other countries [Citation22]. This situation may be related to higher hypertension awareness among women and non-overweight people. This was reported in previous studies, including in Vietnam [Citation13, Citation20]. Surprisingly, the increase in age appeared to cause more disagreement in self-reported hypertension. Previous studies show inconsistent results related to this factor [Citation16, Citation21, Citation22]. Initially, we thought that older people were in high-risk groups for hypertension, so they should be more accurate in their self-reported hypertension. This could imply that the healthcare system needs to give more consideration to the elderly with hypertension.
Smoking and drinking were found to be associated with the validity of self-reported hypertension at the univariate level of analysis. However, at the multivariate level, no relationship was found. This confirms the previous finding in Iran [Citation8].
The strength of this study lies in the large nationally representative sample, and the results of this study can be generalized to the whole Vietnamese adult population. Additionally, blood pressure was measured three times, and this repetition may be sufficient to reduce false-positive results of measured hypertension. Third, the study provides the first report on the accuracy of self-report hypertension in Vietnam.
We are aware that our research may have some limitations. Firstly, the white coat syndrome may lead to false positive hypertension. This may lead to biased estimates of the prevalence of hypertension. However, blood pressure was measured three times, and the mean of the three values was used for hypertension diagnosis. The second is an inaccuracy in the ability of subjects to recall or report the condition. We tried as much as possible to check information based on their medical record, if they have one, at commune health stations to correct their self-report.
Conclusion
In summary, the findings of this study support the idea that self-reported hypertension tends to be underestimated. As hypertension is asymptomatic in its early phases, our findings imply the importance of improving knowledge for the public that may influence the accuracy of reports. However, the intervention should address and focus on disadvantaged groups such as the elderly, farmers, and ethnic minorities.
Therefore, future studies on the current topic are required to identify more predictors, explore the contextual effects of inconsistency between self-reported hypertension and measurement data, and develop and implement public health interventions targeting appropriate subgroups of the population.
Ethics approval
The original research was approved by the Ethical Review Committee of Hanoi Medical University (Decision No 122/HĐĐĐ-ĐHYHN, 28th February 2013). All participants signed informed consent at the time of participation.
Acknowledgment
This article used the dataset of the National study ĐTĐL.2012-G/32 “Predicting and responding model to communicable and non-communicable diseases related to climate change in Vietnam” conducted from 2013 to 2016. This research was funded by a grant from the Ministry of Science and Technology, Vietnam.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Hoang Thi Hai Van
Hoang Thi Hai Van, MD, MPH, Ph.D., is a Chair of the Department of Global Health, School of Preventive and Public Health, Hanoi Medical University, Hanoi, Vietnam.
Dang Thi Huong
Dang Thi Huong, MD, MS, is a research assistant at the Center for Training and Research on Substance Abuse – HIV, Hanoi Medical University, Hanoi, Vietnam.
Tran Ngoc Anh
Tran Ngoc Anh is a student in Preventive Medicine Doctor at the School of Preventive and Public Health, Hanoi Medical University, Hanoi, Vietnam.
References
- Hypertension [internet]. 2023 [cited 2023 Nov 08]; Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.
- Karakayalı M, Püşüroğlu H, Altunova M, et al. Predictive Value of the SCORE, SCORE2, and Pooled Cohort Risk Equation Systems in Patients with Hypertension Turk Kardiyol Dern Ars. 2023 Sep;51(6):1–8. doi: 10.5543/tkda.2022.69570.
- Iqbal AM, Jamal SF. Essential hypertension. Available from: https://europepmc.org/article/NBK/nbk539859.
- Papadopoulos DP, Mourouzis I, Thomopoulos C, et al. Hypertension crisis. Blood Pressure. 2010 Dec;19(6):328–336. doi: 10.3109/08037051.2010.488052.
- High blood pressure now more common in low and middle-income countries, new report finds | UN News [internet]. 2023 [cited 2023 Nov 08]; Available from: https://news.un.org/en/story/2021/08/1098342.
- Kulkarni S. Hypertension management in 2030: a kaleidoscopic view. J Hum Hypertens. 2021 Sep;35(9):812–817. doi: 10.1038/s41371-020-00438-8.
- Douglas BM, Howard EP. Predictors of Self-Management Behaviors in Older Adults with Hypertension. Advances in Preventive Medicine. 2015 Aug;2015:e960263. doi: 10.1155/2015/960263.
- Najafi F, Pasdar Y, Shakiba E, et al. Validity of Self-reported Hypertension and Factors Related to Discordance Between Self-reported and Objectively Measured Hypertension: Evidence From a Cohort Study in Iran. J Prev Med Public Health. 2019 Mar;52(2);131–139. doi: 10.3961/jpmph.18.257.
- Schwartz CL, McManus RJ. What is the evidence base for diagnosing hypertension and for subsequent blood pressure treatment targets in the prevention of cardiovascular disease? BMC Med. 2015 Oct;13:256. doi: 10.1186/s12916-015-0502-5.
- Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013 Aug;3(8): e003423. doi: 10.1136/bmjopen-2013-003423.
- Meiqari L, Essink D, Wright P, et al. Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis. Asia Pac J Public Health. 2019 Mar;31(2):101–112. doi: 10.1177/1010539518824810.
- Hoang VM, Tran QB, Vu THL, et al. Patterns of Raised Blood Pressure in Vietnam: Findings from the WHO STEPS Survey 2015. International Journal of Hypertension. 2019 Dec;2019:e1219783. doi: 10.1155/2019/1219783.
- Son PT, Quang NN, Viet NL, et al. Prevalence, awareness, treatment and control of hypertension in Vietnam—results from a national survey. J Hum Hypertens. 2012 Apr;26(4). doi: 10.1038/jhh.2011.18.
- Huynh Van M, Nguyen Lan V, Van Huy T, et al. Asian management of hypertension: Current status, home blood pressure, and specific concerns in Vietnam. J Clin Hypertens (Greenwich). 2020 Jan;22(3):519–521. doi: 10.1111/jch.13780.
- Xie D, Wang J. Comparison of self-reports and biomedical measurements on hypertension and diabetes among older adults in China. BMC Public Health. 2020 Nov;20:1664. doi: 10.1186/s12889-020-09770-7.
- Chun H, Kim IIH, Min KD. Accuracy of Self-reported Hypertension, Diabetes, and Hypercholesterolemia: Analysis of a Representative Sample of Korean Older Adults. Osong Public Health and Research Perspectives. 2016 Apr;7(2):108–115. doi: 10.1016/j.phrp.2015.12.002.
- Guo H, Yu Y, Ye Y, et al. Accuracy of Self-Reported Hypertension, Diabetes, and Hyperlipidemia among Adults of Liwan, Guangzhou, China. Iran J Public Health. 2020 Sep;49(9):1622–1630.
- Gorber SC, Tremblay M, Campbell N, et al. The Accuracy of Self-Reported Hypertension: A Systematic Review and Meta-Analysis. Current Hypertension Reviews. 2008;4(1):36–62. doi: 10.2174/157340208783497192.
- Quoc Cuong T, Van Bao L, Anh Tuan N, et al. Associated Factors of Hypertension in Women and Men in Vietnam: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2019 Jan;16(23). doi: 10.3390/ijerph16234714.
- Hien HA, Tam NM, Tam V, et al. Prevalence, Awareness, Treatment, and Control of Hypertension and Its Risk Factors in (Central) Vietnam. International Journal of Hypertension. 2018 May;2018:e6326984. doi: 10.1155/2018/6326984.
- Ning M, Zhang Q, Yang M. Comparison of self-reported and biomedical data on hypertension and diabetes: findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open. 2016 Jan;6(1):e009836. doi: 10.1136/bmjopen-2015-009836.
- Tenkorang EY, Sedziafa P, Sano Y, et al. Validity of Self-Report Data in Hypertension Research: Findings From The Study on Global Ageing and Adult Health. The Journal of Clinical Hypertension. 2015;17(12):977–984. doi: 10.1111/jch.12616.
- Demombynes G, Testaverde M. Employment Structure and Returns to Skill in Vietnam: Estimates Using the Labor Force Survey. World Bank, Washington, DC. 2018.
- Hoai NT, Dang T. The determinants of self-medication: Evidence from urban Vietnam. Social Work in Health Care. 2017 Apr;56(4):260–282. doi: 10.1080/00981389.2016.1265632.