Abstract
Background and objectives
Schema group therapy is a potentially cost-effective treatment for borderline personality disorder (BPD). We piloted the feasibility and effectiveness of a 20-session schema group therapy without individual therapy among psychiatric BPD outpatients in a randomized pilot study registered as a clinical trial (ISRCTN76381242).
Methods
Altogether 42 psychiatric outpatients diagnosed with BPD were randomized 2:1 to a 20-session weekly schema group therapy plus treatment as usual (TAU) (n = 28) vs. a control group with TAU alone (n = 14). The primary outcome was decline of BPD symptoms in the short Borderline Symptom List (BSL-23) score. Secondary outcomes were decline in symptoms of anxiety, depression, alcohol use, and improvement in functioning and schema modes. Two external experts evaluated validity of the intervention based on videotaped sessions.
Results
Overall, 23 schema group therapy patients (82%) and 12 controls (86%) completed their treatment. Treatment validity good or very good. However, no significant differences emerged in the primary outcome mean BSL-23 decline (6.95 [SE 5.91] in group schema therapy vs. 12.55 [4.85] in TAU) or in any of the secondary outcome measures.
Limitations
Despite randomization, the TAU subgroup had non-significantly higher baseline scores in most measures. Small sample size predisposing to type II errors; reliance on self-reported outcomes.
Conclusions
Schema group therapy was feasible for psychiatric outpatients with BPD. However, in this small pilot study we did not find it more effective than TAU. Effectiveness of this short intervention remains open.
1. Introduction
Borderline personality disorder (BPD) is a severe mental disorder that sets a major burden on health care [Citation1]. Its prevalence is estimated to be 0.9–3% in the general population and 6% in primary health care patients [Citation2–5]. BPD is diagnosed in every fourth psychiatric outpatient [Citation6] and in up to 40% of psychiatric inpatients [Citation7]. BPD is highly comorbid with mood, anxiety and substance use disorders as well as with somatic illnesses, and confers significant risk for suicide (up to 10%) and non-suicidal self-injury [Citation4,Citation8–10]. BPD-specific therapies (dialectical behavior therapy, mentalization-based therapy, schema therapy, and transference-focused psychotherapy) have been shown to reduce BPD severity and depression and to enhance psychosocial functioning [Citation11,Citation12]. Despite the evidence, many patients miss the effective treatment due to the unavailability of trained psychotherapists [Citation13] and because individual psychotherapies require substantial resources [Citation14]. In the meta-analysis by [Citation11], the effectiveness of different therapies for BPD was not related to treatment duration. Shorter interventions would allow patients to participate in BPD-specific therapies. Accordingly, there is ongoing research on the effectiveness of brief interventions for BPD [Citation14].
Schema therapy, one of the most recent, promising psychotherapies for BPD [Citation15], targets BPD patients’ emotional instability. As postulated in schema therapy, patients learn to understand and manage their emotional reactions, modes, in which the patients’ unmet childhood or adolescence core needs activate in adulthood situations and cause patients to behave in a non-functional manner [Citation16,Citation17]. Schema therapy centers on fulfilling the unmet core needs by increasing patients’ insight into their reactions and providing emotional support in the form of limited re-parenting. It engages experiential techniques such as chairwork and imagery re-scripting. Schema therapy has been shown to reduce BPD symptom severity, suicide-related outcomes, and depression compared with treatment as usual or some other BPD-specific therapies [Citation18–20].
Group schema therapy was developed by Farrell to combine schema therapy with the benefits of group. These include peer support, learning from others and providing experiences of belongingness and acceptance [Citation21]. In a small controlled study by [Citation19], a group schema therapy of 8 months was found to be effective in reducing BPD symptoms. In this pioneering study, 94% of group schema therapy patients versus 15% of control patients no longer met the criteria for BPD after the intervention. This has been speculated to be due to the therapists being schema therapy experts and the study patients highly motivated [Citation22]. Further, two small uncontrolled studies with 1- to 2-year group schema therapy combined with individual care have suggested a reduction in BPD and general symptoms and maladaptive schema modes [Citation23,Citation24]. In addition, brief schema group therapy forms of 12–20 sessions with an individual treatment have in uncontrolled studies displayed a significant reduction in BPD and general symptoms as well as maladaptive schema modes [Citation25,Citation26]. The brief group form of 20 sessions has also shown a promising effect on mixed personality disorder patients’ general symptoms in uncontrolled studies [Citation27,Citation28]. However, insufficient research evidence exists for effectiveness of group schema therapy relative to treatment as usual, or of group format alone in BPD. An ongoing international multicenter RCT aims as investigating these issues [Citation29], but the results have not yet been published.
BPD patients set major requirements for psychiatric care in terms of both resources overall and specialized psychotherapy. With the limited capacity of psychiatric outpatient care, it is difficult to introduce new treatment options that require intensive individual therapy or prolonged treatment. This calls for investigating the applicability of schema therapy in group format and of a length within the capacity of psychiatric outpatient settings in the treatment of BPD patients. We therefore aimed at piloting the feasibility and effectiveness of a brief, 20-session schema group therapy for BPD patients. The study was conducted within the facilities of the Mood Disorder Division of the Department of Psychiatry, Helsinki University Hospital and took place locally at the Tikkurila Outpatient Clinic in the city of Vantaa. We hypothesized that a brief group schema therapy combined with usual psychiatric treatment would (1) result in greater decline in BPD symptoms than treatment as usual (TAU) alone and (2) mitigate symptoms of anxiety and depression, decrease alcohol usage and enhance patients’ overall functioning more than the usual care.
2. Methods
2.1. Trial design
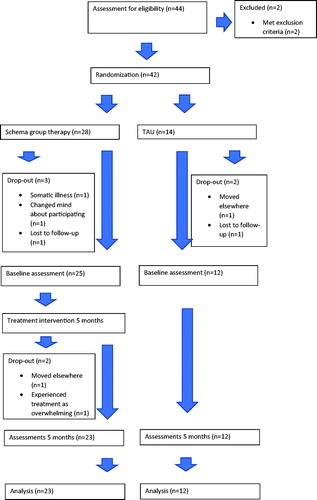
The study was a randomized, parallel-arm prospective intervention study comparing (1) brief group schema therapy plus usual psychiatric treatment with (2) usual psychiatric treatment alone in treatment of BPD. The study design is illustrated in . The study was accepted by the Helsinki and Uusimaa Hospital District (HUS) Ethics Committee, and thereafter registered as a clinical trial (ISRCTN76381242, acronym GST-BPD).
We aimed at recruiting altogether 64 patients in the study and randomizing them in a 1:1 ratio. However, we had a time frame of one year because of the limited work contract of the first author. Therefore, we had only a few months’ time to recruit patients from the local outpatient clinic and were unable to meet the objective by prolonging recruitment. The patient count was determined by the capacity of the outpatient clinic. The researchers provided the study schema group therapy as part of their normal clinical work. Due to the limited number of recruited volunteer patients, we had to change the randomization from 1:1 to 2:1 because the implementation of group therapy necessitates a group size of at least 6 patients. In smaller groups occasional illness absences and drop-outs can result in the group no longer working effectively and providing the necessary peer support.
Patients were recruited to the study at the end of the year 2017 and in spring 2018. We asked the personnel of the Tikkurila Outpatient Clinic to inform potentially suitable and volunteering BPD patients about schema group therapy. After this, we examined from these patients’ psychiatric records that they met the inclusion, but not the exclusion criteria. We invited the eligible patients for an interview and assessed clinically their suitability for the study. The personnel of the outpatient clinic routinely use Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) interviews for patients with symptoms of BPD to diagnose BPD, which has shown an excellent inter-rater reliability for BPD [Citation30]. In a few cases, the diagnostic interview had not been conducted, and the first author (H-M.H.) personally interviewed these patients with the SCID-II. The eligible patients received information on the study in verbal form as well as on an information sheet. All patients gave written informed consent. The last author (E.I.), who was blind to the participant list, then randomized the participants to the treatment groups and control group in a ratio of 2:1 in blocks of three using the Research Randomizer program.
The trial comprised four treatment groups and two parallel control groups divided into two phases (spring and fall) in 2018, each of which included 20 sessions over a 5-month period. Information was gathered from both treatment group and controls at the beginning and the end of the group intervention.
Participants were recorded as drop-outs if they expressed a wish to discontinue the study or if they withdrew from contact and did not respond to repeated contact efforts.
The study data were collected into a database in the Helsinki University Hospital data network in an anonymized form.
2.2. Participants
We recruited to the study patients with a clinical diagnosis of BPD from the Mood Disorder Division of the Department of Psychiatry, Helsinki University Hospital. All patients had been diagnosed with the DSM-IV SCID-II interview before study onset. We included in the study both recently referred and diagnosed patients, and those who had also previously received treatment for BPD.
We excluded from the study patients who had (1) psychotic symptoms, (2) imminent risk of suicide, (3) principal diagnosis of or uncontrollable substance use disorder, (4) any illness or symptoms that would hamper participation in treatment, or (5) other ongoing specific psychotherapy. As an example of the fourth category, we excluded two participants with marked dissociative symptoms precluding their treatment in group format. The participants in our study were not in imminent risk of self-harm, but had major difficulties in mood regulation or in their relationships. We excluded patients at imminent risk for suicide, as there is an ongoing dialectical behavior therapy treatment program at the outpatient clinic, which we considered to be the best option for these patients.
2.3. Interventions
The group schema therapy was adapted from the Farrell and Shaw group schema therapy manual for BPD patients [Citation21], but as a shorter version and with more emphasis on experiential than cognitive work because of cost-efficiency. The schema group therapy program is outlined in . All four groups followed the same manual.
Table 1. Program of the schema group therapy.
The treatment groups consisted of 5–7 participants. Each group comprised 20 weekly sessions of 90 min. The group structure consisted of a beginning session, 6 sessions on mode recognition and awareness, 12 experiential work sessions, about half of which included imagery re-scripting, and a finishing session (). Imagery re-scripting is an experiential technique in which the therapist aids the patient to visualize a meaningful and traumatic past experience and they work together to rewrite a new solution that answers to the patient’s unmet needs. The therapy group participants frequently wished to discuss with the group therapists issues related to their life situation or evoked by the treatment. Altogether four therapists participated in the intervention. Each group had two main therapists, with the other therapists substituting for the main therapists when needed. All therapists had 2–4 years’ cognitive or cognitive-analytic therapy training and schema therapy training of 6 days with at least 40 h schema therapy supervision in a group setting. In addition, the therapists were supervised during the interview by an ISST Group ST-certified therapist. One therapist left in the middle of two groups for maternity leave, and the other therapists continued with the groups. As the maternity leave was expected, patients were informed about it at the beginning of the intervention. All therapists participated in the group sessions from the beginning, the content of the sessions was unchanged, and the therapist on maternity leave participated in weekly planning of and reflection on the sessions.
2.4. Validity of treatment
To estimate the validity of the treatment, the treatment sessions were video-taped with the camera focused on therapists, not participants. Seven of the 80 therapy session video-tapes had technical errors. Of each of the four treatment groups, one mode recognition and awareness session, one imagery re-scripting session, and one other experiential work session were randomized for external evaluation by using the Research Randomizer program. Two external experts, supervisor-trainers in cognitive psychotherapy and schema therapy, rated the randomized therapy sessions with the Group Schema Therapy Assessment Scale (GSTRS-R), which is a specific instrument for group schema therapy. This instrument has shown substantial internal consistency and inter-rater reliability and adequate discriminative validity [Citation31]. It includes a 7-point scale: 0 = very poor, 1 = poor, 2 = unsatisfactory, 3 = adequate, 4 = good, 5 = very good and 6 =excellent.
The external experts rated all items from 4 to 6. The mean scores of the two external experts’ evaluation were 4.7 and 4.7 (weighted Cohen’s kappa for inter-rater reliability 1.00) for therapist behavior, 4.4 and 4.7 for reparenting (weighted Cohen’s kappa 0.87), 4.8 and 4.4 for structure (weighted Cohen’s kappa 0.91), 4.0 and 4.0 (weighted Cohen’s kappa 1.00) for mode awareness and change, 5.0 and 5.0 (weighted Cohen’s kappa 1.00) for cognitive interventions, and 5.0 and 5.0 (weighted Cohen’s kappa 1.00) for experiential interventions. The session topics in the randomized video-tapes did not cover all scales measured in the instrument.
2.5. Treatment as usual (TAU)
In the Mood Disorder Division of Helsinki University Hospital Department of Psychiatry, the usual treatment comprises visits with a psychiatrist or psychiatric resident, and therapy sessions of 45 min on average once a month with a psychiatric nurse. The treatment may also include periods of weekly therapy with a psychologist or other group treatment such as dialectical behavior therapy (1 patient). At the beginning of the study the participants in TAU had only infrequent visits with a psychiatric nurse, but during the study four patients started a more intensive individual therapy and one started a DBT group. Most patients receive both pharmacotherapy and some form of psychosocial support or psychotherapy. Most of the participants used antidepressants and many used medications for sleep or anxiety when needed. Some used low doses of antipsychotics (mainly quetiapine) for anxiety or depression.
2.6. Primary and secondary outcomes
The primary outcome measure was intra-individual change (expectedly decline) in borderline personality symptoms between the study baseline and the end, which was compared at group level between the two groups. To investigate this, we used the short Borderline Symptom List (BSL-23) –scale [Citation32]. The BSL-23 scale is a self-rating instrument of BPD symptomatology with a 23-item scale, also including a behavior scale of 11 items to evaluate BPD behavior. It derives from the original BSL-95 scale of 95 items and has shown good psychometric properties comparable to those of the BSL-95. In general, the BSL-23 score is interpreted as follows: 0-1 point refers to no, 2-23 points to mild, 24-69 points to moderate, and 70-92 points to severe BPD symptoms. In addition to the total symptom score as the predetermined primary outcome, we analyzed post hoc the BSL-23 behavior score. We did not determine a clinically relevant change in the BSL total score, as there is no clear evidence of what this would be in the Finnish patient population, but expected an apparent change in BPD symptoms.
As secondary outcome measures, we used the following self-report instruments to investigate intra-individual change during treatment: a) the Patient Health Questionnaire 9 (PHQ-9) is a 9-item instrument with a scale of 0-3 for depressive symptoms and a cut-off of 10 points [,Citation33]; b) the Overall Anxiety Severity and Impairment test (OASIS) consists of 5 items with a scale from 0 to 4 that measures anxiety symptoms with a cut-off of 8 points [Citation34]; c) the Alcohol Use Disorders Identification test (AUDIT) is a 10-item instrument with a 0-4 scale in each item to test alcohol use with a cut-off of 8 points [Citation35]; d) the Sheehan Disability Scale (SDS) measures functional impairment in the domains of work, family life or home responsibilities, and social or leisure activities with a visual analogue scale of 0-10 in each domain and a cut-off of 5 points in each domain [Citation36]; and e) the Schema Mode Inventory (SMI) consists of 118 items linked to 14 dysfunctional and healthy schema modes with a cut-off of 50% in each mode [Citation37]. PHQ-9, OASIS, AUDIT, and SDS have proved to be valid and reliable measures of depression, anxiety, alcohol use, and disability, respectively [Citation33–36]. SMI has shown acceptable internal consistency, test-retest reliability and construct validity to test schema modes [Citation37]. We analyzed change in BPD specific dysfunctional schema mode scores (vulnerable child mode, angry child mode, detached protector mode, and punishing parent mode).
In addition, we gathered general socio-demographic information such as age, gender, marital status, habitation, education, work status, whether participants had children, participants’ motivation for treatment, and their experience of the treatment relationship. We reviewed participants’ psychiatric records. The treatment group participants were also requested to provide informal written feedback on the group experience.
The sample size remained smaller than we had planned (total 64), and in the self-report measures there was a notable amount of missing data. Therefore, we decided to impute missing values in the statistical analysis.
2.7. Statistical analysis
We used SPSS 25 and R, version 3.5.1., for statistical analysis. When comparing socio-demographic factors between treatment group and controls, we used Chi-square for categorical and Welch t-test or Kruskal–Wallis test for continuous variables depending on the normality distribution. When comparing treatment group patients with controls in terms of change in study measures, we used Welch t-test or Kruskal–Wallis test for continuous variables depending on the normality distribution. To test inter-rater reliability in the assessment of therapy validation, we used weighted Cohen’s kappa.
We aimed at intention-to-treat (ITT) analyses. However, no meaningful data were available from those five consenting participants who dropped out between randomization and baseline evaluation. Therefore, we could form the ITT samples only by including participants who gave baseline data. Multiple imputation with chained equations (mice R-package version 2.30) was used for missing-data imputation, with moment-based statistics and an F reference distribution for testing [Citation38,Citation39], thereby providing an ITT analysis of our data [Citation40]. Altogether 35 data imputation chains were initiated and monitored to a well-mixed state. Linear models were used to test the effect of treatment group membership on the outcome score change from pre-treatment to post-treatment. The models were estimated in all 35 imputed data-sets and the estimates were combined using standard Rubin’s rules. This method takes into account the uncertainty in both individual estimates and imputed values. The imputation models were based on predictive mean matching and used a default algorithm (“quickpred”) to choose variables predictive of other variables (e.g. r –> 0.1 was required). The variables used to draw information on missingness were age, sex, treatment group status, individual BSL-23 items, and sum scores for OASIS, AUDIT, PHQ-9, all Sheehan scales, and four of the SMI schema mode scales, namely vulnerable child mode, angry child mode, detached protector mode, and punishing parent mode.
3. Results
3.1. Participants
Altogether 42 patients were recruited and randomized to intervention (group schema therapy plus TAU) or control (TAU alone) groups. Three participants who had given their consent for the study and were randomized to the intervention groups did not attend them. Two participants dropped out from the intervention groups: one moved to another city and the other perceived the treatment as too overwhelming. Two participants withdrew from the control groups. Altogether 23 participants remained in the schema therapy intervention groups and 12 in the control groups throughout the study. The drop-out rate was for the treatment group 15%, including those who did not start the intervention, and for the control group 14%.
During the intervention period the intervention group participants had on average 16.8 schema group therapy sessions of 90 min. The intervention group participants had on average 4.3 individual treatment visits (range 0–19, SD 4.4) of 45 min and the control group participants on average 10.3 individual treatment visits of 45 min (range 2–19, SD 5.4) at the outpatient clinic. The participants did not have hospital visits during the intervention. Of the 12 controls, four started weekly individual therapy and one started dialectical behavior therapy with weekly group and individual sessions during the intervention period.
Intervention group participants were on average 31 years old (±SD 8.8), whereas control group participants were on average 27 years old (±SD 3.7). The intervention and control group participants are compared in terms of socio-demographic and clinical factors in .
Table 2. Sociodemographic and clinical characteristics of intervention and control group patients.
All of the participants filled in the pre-treatment assessment forms, whereas the drop-out participants refused to fill in the post-treatment assessment forms. We included all assessments in the study, and imputed missing data.
3.2. Treatment outcomes
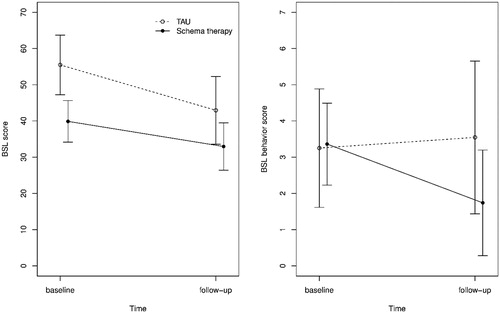
The primary outcome measure was intraindividual decline in the BSL-23 symptom score. Despite randomization, the controls were unexpectedly found to have numerically higher BSL-23 scores before and after treatment (, left panel). However, no statistically significant group difference emerged in the primary outcome; the average decline in BSL-23 scores was 6.95 in the schema therapy group (SE 5.91) and 12.55 (SE 4.85) in the TAU group.
Figure 2. Average BSL score (left panel) and BSL behavior score (right panel) in the TAU and Schema therapy groups at both baseline and follow-up. The whiskers denote 95% Wald’s confidence intervals.
The secondary outcome measures within-person changes in OASIS score for anxiety symptoms, PHQ score for depressive symptoms, AUDIT score for alcohol use, and SDS for general functioning. No significant differences were present between the treatment and control groups (). In addition, we analyzed change in BPD specific dysfunctional schema mode scores (vulnerable child mode, angry child mode, detached protector mode, and punishing parent mode). In three of the four dysfunctional schema modes, there was numerically more decline in the intervention group, but the difference was not significant.
Table 3. Treatment effects with multiple imputation of missing data.
In post-hoc analysis, the BSL-23 behavior subscale scores declined more in the schema therapy group (2.42, SE 0.96) than in TAU (0.36, SE 0.79). This was a statistically significant difference (p = 0.033).
3.3. Informal feedback from the treatment group
The treatment group participants had an opportunity to give written informal feedback on their group experience. The most common themes and the numbers of participants spontaneously mentioning the same theme were as follows: Therapists were considered as professional (11) and the groups as open (7), accepting (8), and safe (4). The participants felt that their emotional management (9) and insight (8) had increased during the group process, and they valued the peer support (13) and group spirit (8). As negative aspects, they noted that the groups should have continued longer (8) and that the group sessions were too short (4). Two participants also mentioned that some childhood memories or inner processes appeared at the end of the group, and they felt they were left alone to deal with these as the group ended. When asked about how strongly the participants would recommend the group on a 0-10 scale, 20 of 21 participants gave a recommendation of 8-10.
4. Discussion
This pilot study was conducted at the Department of Psychiatry of Helsinki University Hospital, Finland. A brief form of group schema therapy with no individual treatment other than TAU was chosen to test its feasibility for BPD patients in psychiatric outpatient care. The setting of this pilot study was a psychiatric outpatient clinic, enabling assessment of how the treatment would actually be delivered to typical psychiatric BPD outpatients. We found brief group schema therapy to be realistic to carry out in psychiatric outpatient care, and patient satisfaction was high. However, we were unable to show it to be more effective than usual care alone. The primary outcome of the study, a within-subject decrease in BSL-23 symptom score, was negative. Participants improved in both schema therapy and usual treatment, with no significant difference emerging between the groups. The same was true for the secondary outcomes, declines in PHQ-9, OASIS, AUDIT, and SDS. In post-hoc analysis, however, the BSL-23 behavior score suggested a potentially significant treatment effect.
Strengths of this pilot study include that it was registered, randomized, controlled, and conducted in typical psychiatric outpatient settings. All participants were diagnosed with SCID-II, a structured interview. The drop-out rate in the schema therapy group was low, and patient satisfaction with treatment was high. The validity of the schema therapy group intervention was rated as good to very good by external evaluators, indicating that the negative treatment outcome was not related to the quality of the treatment. The most important limitation of this pilot study is, that the sample size was small, making it vulnerable to type II errors and spurious findings. We were unable to recruit more patients in the brief time that we had before beginning the study. Nevertheless, the total sample size was actually larger than that of a pioneering RCT [Citation19] or the uncontrolled study by [Citation26]. To allocate sufficient numbers of patients to the schema therapy groups, we needed to randomize the participants in a ratio of 2:1, rendering the control group even smaller. Another limitation is that the primary and secondary outcome measures were all based on self-report. In addition, during the study five participants in the control group started weekly individual therapy, whereas the schema group participants had fewer individual sessions, complicating comparison of treatment outcomes. Despite the randomization, the controls unexpectedly had higher baseline scores on the BSL-23 and most other measures. Uneven distributions may occur when randomizing small samples. Another possible source of bias arises from timing of baseline assessment after randomization. Participants’ disappointment at being allocated to the TAU group may have inflated the (self-reported) baseline measures in this emotionally unstable patient group.
The negative primary and secondary outcomes likely indicate that the group schema therapy is not effective as a treatment, the study lacked sufficient statistical power, or the intervention was too brief and/or should have included individual sessions. Schema group therapy was found to be effective in BPD patients in a controlled study with a longer group therapy of 30 sessions [Citation18], whereas other brief schema group therapy studies have been uncontrolled [Citation25,Citation26]. The other studies had in addition weekly individual sessions, whereas participants in our study had individual sessions on average once a month, which is typical for the psychiatric outpatient setting [Citation18,Citation25,Citation26]. While the reasons for not finding significant differences remain open, we interpret our findings as not encouraging for the use of the 20-session group schema therapy format without individual sessions in psychiatric outpatient settings. We recommend future studies have a longer group therapy or, include also individual therapy, or both.
In general, specific therapies for BPD (dialectical behavior therapy, cognitive behavior therapy, mentalization-based therapy, transference-focused therapy, schema‐focused therapy, and acceptance and commitment therapy) have been found to be only slightly more effective than non-specific ones (other therapies and psychoeducation), and it is unclear whether this difference is due to the special attention afforded participants in these studies [Citation12]. Meta-analyses have also not found significant differences between the specific therapies for BPD [Citation11,Citation12]. In our study, TAU comprised individual sessions with a psychiatric nurse that had a therapeutic frame or psychoeducation content or for some patients a therapy period with a psychologist, which is similar to non-specific therapy. This can partially explain the results.
In our pilot study, we treated typical psychiatric outpatient care patients with a major psychiatric comorbidity, substance use, poor functioning, and commonly unemployment. By contrast, the participants in the study by [Citation18] had a psychotherapy contact with community psychotherapists and had a better socio-economic position. Patient characteristics of this kind can impact the treatment effect. Also, we included both new patients and those who had already received longer treatment within the facilities in the study. Patients with a longer treatment history may have a more chronic illness and benefit less from a short therapy.
5. Conclusions
In our pilot study, the schema group therapy was found to be feasible, but no more effective than TAU. It is essential that studies evaluating treatment outcome are randomized and controlled. In our study, participants improved in both the treatment and control groups. Without the control group, we might have concluded that the treatment was effective, given the observed improvement. Patient satisfaction with the treatment was not a guarantee of treatment effect. The 20-session group therapy without individual therapy may have been insufficient for this challenging patient group and we do not recommend repeating this study protocol. Instead, we suggest using a longer group schema therapy or adding individual sessions to the group format.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
Notes on contributors
Hanna-Mari Hilden
Hanna-Mari Hilden, MD, PhD, is Associate Chief Physician in Helsinki University Hospital, Psychiatry, Mood Disorders Department. Her research mainly focuses on medical ethics and social medicine. She has piloted the first schema therapy groups in Finland in 2017.
Tom Rosenström
Tom Rosenström, PhD (psychology), MSc (applied mathematics), docent, LP, is an Academy of Finland Research Fellow at the Department of Psychology and Logopedics, Faculty of Medicine, University of Helsinki, Helsinki, Finland. He has worked on academic questions of mental health research for more than 10 years.
Irma Karila
Irma Karila, LP, PhD, is a licensed psychotherapist (advanced). Her 40-year career has focused on psychotherapy training and supervision, specialized in the treatment of depression and personality disorders. She has co-authored Guide to Schema therapy and the Handbook of Cognitive psychotherapy (in Finnish).
Aila Elokorpi
Aila Elokorpi, BN, RN, is a psychiatric nurse in Helsinki University Hospital, Psychiatry, Mood Disorders Department. She works mainly with patients with borderline disorder, anxiety disorder, depression and bipolar disorders.
Mirka Torpo
Mirka Torpo, LP, works as a psychologist in Helsinki University Hospital, Psychiatry, Mood Disorders Department. She is a licensed psychotherapist.
Ritva Arajärvi
Ritva Arajärvi, MD, PhD, is Chief Physician in Helsinki University Hospital, Psychiatry, Mood Disorders Department. Her research mainly focuses on schizophrenia. She is a licensed psychotherapist.
Erkki Isometsä
Erkki Isometsä, MD, PhD, is Professor of Psychiatry at the University of Helsinki, Chair of the Finnish Task Force for Current Care Guidelines for Depression, and President of The Finnish Psychiatric Association. His research mainly focuses on clinical epidemiology, risk factors, pathogenesis and treatment of mood disorders and suicidal behaviour.
References
- Bohus M, Schmahl C. Psychopathologie und therapie der borderline-persönlichkeitsstörung. Deutsches Ärzteblatt. 2006;103:3345–3352.
- Gross R, Olfson M, Gameroff M, et al. Borderline personality disorder in primary care. Arch Intern Med. 2002;162(1):53–60.
- Samuels J. Personality disorders: epidemiology and public health issues. Int Rev Psychiatry. 2011;23(3):223–233.
- Tomko RL, Trull TJ, Wood PK, et al. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. J Pers Disord. 2014;28(5):734–750.
- Volkert J, Gablonski T-C, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):709–715.
- Korzekwa MI, Dell PF, Links PS, et al. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. 2008;49(4):380–386.
- Zimmerman M, Chelminski I, Young D. The frequency of personality disorders in psychiatric patients. Psychiatr Clin North Am. 2008;31(3):405–420.
- Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42(6):482–487.
- Leichsenring F, Leibing E, Kruse J, et al. Borderline personality disorder. Lancet. 2011;377(9759):74–84.
- Trull TJ, Freeman LK, Vebares TJ, et al. Borderline personality disorder and substance use disorders: an updated review. Borderline Personal Disord Emot Dysregul. 2018;5:15.
- Cristea IA, Gentili C, Cotet CD, et al. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(4):319–328.
- Storebø OJ, Stoffers-Winterling JM, Völlm BA, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5:CD012955.
- Hermens ML, van Splunteren PT, van den Bosch A, et al. Barriers to implementing the clinical guideline on borderline personality disorder in the Netherlands. Psychiatr Serv. 2011;62(11):1381–1383.
- McMain SF, Chapman AL, Kuo JR, et al. The effectiveness of 6 versus 12-months of dialectical behaviour therapy for borderline personality disorder: the feasibility of a shorter treatment and evaluating responses (FASTER) trial protocol. BMC Psychiatry. 2018;18(1):230.
- Oud M, Arntz A, Hermens ML, et al. Specialized psychotherapies for adults with borderline personality disorder: A systematic review and meta-analysis. Aust N Z J Psychiatry. 2018;52(10):949–961.
- Arnzt A, van Genderen H. 2009. Schema therapy for borderline personality disorders. Sussex: John Wiley.
- Young JE, Klosko JS, Weishaar ME. 2003. Schema therapy: a practitioner’s guide. (1st ed.). New York: The Guilford Press.
- Giesen-Bloo J, van Dyck R, Spinhoven P, et al. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs. transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63(6):649–658.
- Farrell JM, Shaw IA, Webber MA. A schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: A randomized controlled trial. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40(2):317–328.
- Mohamadizadeh L, Makvandi B, Pasha R, et al. Comparing of the effect of dialectical behavior therapy (DBT) and schema therapy (ST) on reducing mood activity and suicidal thoughts in patients with borderline personality disorder. Acta Medica Mediterranea. 2017;33:1025–1031.
- Farrell JM, Shaw IA. 2012. Group schema therapy for borderline personality disorder: A step-by-step treatment manual with patient workbook. New York: Wiley.
- Jacob GA, Arntz A. Schema therapy for personality disorders – a review. Inter J Cognitive Ther. 2013;6(2):171–185.
- Dickhaut V, Arntz A. Combined group and individual schema therapy for borderline personality disorder: a pilot study. J Behav Ther Exp Psychiatry. 2014;45(2):242–251.
- Fassbinder E, Schuetze M, Kranich A, et al. Feasibility of group schema therapy for outpatients with severe borderline personality disorder in germany: a pilot study with three year follow-up. Front Psychol. 2016;7:1851.
- Reiss N, Lieb K, Arntz A, et al. Responding to the treatment challenge of patients with severe BPD: Results of three pilot studies of inpatient schema therapy. Behav Cogn Psychother. 2014;42(3):355–367.
- Nenadić I, Lamberth S, Reiss N. Group schema therapy for personality disorders: a pilot study for implementation in acute psychiatric in-patient settings. Psychiatry Res. 2017;253:9–12.
- Renner F, van Goor M, Huibers M, et al. Short-term group schema cognitive-behavioral therapy for young adults with personality disorders and personality disorder features: associations with changes in symptomatic distress, schemas, schema modes and coping styles. Behav Res Ther. 2013;51(8):487–492.
- Skewes SA, Samson RA, Simpson SG, et al. Short-term group schema therapy for mixed personality disorders: a pilot study. Front Psychol. 2014;5:1592.
- Wetzelaer P, Farrell J, Evers SM, et al. Design of an international multicentre RCT on group schema therapy for borderline personality disorder. BMC Psychiatry. 2014;14(1):319.
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother. 2011;18(1):75–79.
- Bastick E, Bot S, Verhagen SJW, et al. The Development and Psychometric Evaluation of the Group Schema Therapy Rating Scale - Revised. Behav Cogn Psychother. 2018;46(5):601–618.
- Bohus M, Kleindienst N, Limberger MF, et al. The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32–39.
- Staples LG, Dear BF, Gandy M, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–18.
- Ito M, Oe Y, Kato N, et al. Validity and clinical interpretability of Overall Anxiety Severity and Impairment Scale (OASIS). J Affect Disord. 2015;170:217–224.
- Selin KH. Test-retest reliability of the alcohol use disorder identification test in a general population sample. Alcohol Clin Exp Res. 2003;27:1428–1435.
- Luciano JV, Bertsch J, Salvador-Carulla L, et al. Factor structure, internal consistency and construct validity of the Sheehan Disability Scale in a Spanish primary care sample. J Eval Clin Pract. 2010;16(5):895–901.
- Lobbestael J, van Vreeswijk MF, Spinhoven P, et al. Reliability and validity of the short schema mode inventory (SMI). Behav Cogn Psychother. 2010;38(4):437–458.
- Li KH, Raghunathan TE, Rubin DB. Large-sample significance levels from multiply imputed data using moment-based statistics and an F reference distribution. J Am Stat Assoc. 1991;86:1065–1073.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–399.
- Van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45:1–67.