Abstract
Objective
To measure rate of subscription of common sleep medication and diagnoses of substance use disorder (SUD) before and after receiving a prescribed weighted blanket (WB) among patients with psychiatric diagnoses.
Materials and methods
Using register-based data of health-related factors in a Swedish region, a total of 1785 adult individuals with a psychiatric diagnosis, received a WB and resided in the region during the study period were identified. Using each individual as their own control, the rate of one-year prior prescription of WB or diagnosed SUD was compared to rate after a half year wash-out after prescription of WB for a full year.
Results
The number of patients without prescription of sleep medication increased by 3.3% (95% confidence interval (95%CI): 0.2–6.4, p=.04). Furthermore, the proportion without a prescription of benzodiazepine receptor agonist/antihistamines sleep medication increased by 5.5% (95%CI: 2.2–8.8, p=.001). Melatonin prescription increased after WB by 3.6% (95%CI: 1.1–6.2, p=.006). Younger age and unipolar-, anxiety-, attention-deficit/hyperactivity-, and post-traumatic stress disorder was associated with decreased use while psychotic-/bipolar- and personality disorder was not associated with a decrease in the use of sleep medication. The number of alcohol SUD diagnoses did not increase while sedative SUD rate increased statistically significantly by 0.7% (odds ratio = 1.63, p=.02). In a multivariate model, only younger age predicted discontinuation of sleep medication while psychotic-/bipolar- and personality disorder had statistically less decrease.
Conclusion
This observational register study found a statistically significant association between WB use and decreased use of common sleep medication except melatonin that increased slightly.
Introduction
Sleep problems are ubiquitous among patients with psychiatric disorders [Citation1]. There are several treatment methods used for insomnia including psychoeducation, pharmacological treatment and behavioral treatment [Citation2], with pharmacologic treatment being frequently used. In 2019, almost one in 10 above the age of 15 years received at least one prescription of hypnotics and sedatives, classified in the group N05C in the Anatomical Therapeutic Chemical Classification System (ATC) in Sweden [Citation3]. Since sleep problems are so common it is important to develop and utilize effective treatment modalities that have minimal risk of adverse events and are evidence-based.
Tactile stimulation, such as obtained through weighted blankets (WBs), is a non-invasive approach that has been gaining attention in recent years. The use of WB is mainly concerned with providing patients with external stimuli that may reduce anxiety and stress, most often included under the term deep pressure stimulation. The safety and effect of WB has been studied for adults and no risk for safety has been identified [Citation4–6]. In healthy participants, WBs used for five minutes did not have negative effects on oxygen saturation, pulse rate, blood pressure or stress levels measured with either skin conduction or self-report [Citation4]. Furthermore, a case series of 30 psychiatric in-patients using a similar experimental setup, showed comparable results with no adverse physiological responses and no increase in anxiety, albeit, when comparing WB to no blanket, both reduced anxiety to a similar degree [Citation5]. A more acute stress response during tooth extraction may be ameliorated by WB as shown by more stable heart rate variability in a randomized-controlled trial [Citation7].
Possible mechanisms that have been proposed for how tactile stimulation may alter well-being, is through pressure to the skin that modulates the automatic nervous system, ultimately affecting central parts, resulting in a calming effect [Citation8,Citation9]. Although the empirical basis for this theory is still mostly anecdotal, several studies have shown physiological responses to tactile stimulation. For example, by applying specific pressure stimulation of fingertips during day-time napping, no effect on the ability to perform a finger tap test was found; however, an altered pattern of recorded electro-encephalogram was found where slow oscillations and sleep spindles differed between sham and active stimulation of fingers during sleep [Citation10], indicating a physical effect of pressure stimulation.
Clinically, WBs seem to be generally accepted by adult patients with neurodevelopmental disorders [Citation11]. A controlled trial in Stockholm, Sweden, showed a significant improvement in insomnia symptoms among patients with diverse psychiatric diagnoses [Citation12] and another recent trial found positive effect of WB as an adjunct therapy for anxiety among oncological outpatients [Citation13]. A recent systematic review concluded that WB may be effective for anxiety but that there was limited evidence for treatment of insomnia [Citation14]; however, this review was published prior to the controlled trial from Stockholm. One associated field of interest is that WB can be to prescribed to those not responding to sleep medication or other treatments available but another indication might be to reduce the use of hypnotics that are generally not recommended for use longer than a few weeks which, however, is not followed in real life practice [Citation15]. That is, WBs may be prescribed as a treatment for patients with sedative use disorder or other substance use disorder (SUD) since sleep medication can be substances of abuse [Citation16] and sleep problems are common in SUDs [Citation17].
A major knowledge gap that should be addressed is the pattern of regular use and the effect on adult patients with psychiatric diagnoses using WB for insomnia. For more than a decade, WB has been prescribed to patients with insomnia by physical- and occupational therapists in the West coast region of Sweden, free of charge for the patients. This provides the possibility for an administrative register database of the use of WB in clinical practice and, furthermore, to investigate whether WB use is associated with SUD diagnoses.
Aims of the study
The aim of this study was to investigate the intra-individual changes in the use of sleep medication by medication category, age, sex and diagnosis, as well as the changes in prevalence of SUD after prescription of a WB. Furthermore, an analysis of the rate of diagnosed SUDs was conducted to control whether patients were mainly prescribed WB due to overconsumption of substances.
Materials and methods
Study design
This is a register-based, observational study using administrative data on the use of WB prescribed in the region of Västra Götaland, Sweden during May 2015 through December 2017. A within-individual comparison was used where each individual served as their own control. Pre-prescription measures were collected from register-data from 365 days prior to receiving a WB and post-prescription measures were collected from register-data during a 365-day period after a wash-out period of 180 days.
Study population
The Region Västra Götaland is on the west coast of Sweden with a population of 1,713,907 as registered from January through March 2019 [Citation18]. It contains both larger urban, as well as rural areas. All persons above 18 years of age who were registered with a psychiatric diagnosis (chapter F in ICD-10), and were prescribed and collected a WB were included in the study. Furthermore, they should be registered inhabitants in the region for at least one year after prescription to be included.
For the severe mental illnesses, a hierarchy was constructed, and an individual could only have one of these diagnoses in this order: psychotic-, bipolar- and unipolar disorder. Other diagnoses were non-exclusive of each other so any psychiatric diagnosis in the preceding year was considered a diagnosis in the analyses.
Measurements
Prescription of weighted blankets
WB is currently available as a prescribed medical-technical aid, free of charge for the patient, in the region of Västra Götaland, Sweden. It requires an assessment by a physical- or occupational therapist who then sends an application to the cost managers in the region. There are three different kinds of WB available: filled with balls, with chains or with fiber. The WB weight varies between 3 and 14 kg and is chosen by the prescribing therapist in agreement with the patient.
Sleep medication
Prescriptions of specific medications were registered in the national register of prescribed medication and the following commonly prescribed sleep medications were included under the following categories (ATC):
Benzodiazepine receptor agonists (BZRA): flunitrazepam (N05CD03), zolpidem (N05CF02) and zopiclone (N05CF01).
Antihistamines: alimemazine (R06AD01), levomepromazine (ATC code: N05AA02), promethazine (R06AD02) and propiomazine (N05CM06).
Melatonin (N05CH01).
Mirtazapine (N06AX11).
Prescriptions of BZRA and antihistamines were analyzed further for both discontinuation and new prescriptions since these were considered of special clinical importance. Furthermore, in the current paper, medication use and rate of prescription were used interchangeably but is by definition the registered prescription retrieval at a pharmacy. The selection of medications was decided in a consensus meeting by the research team in order to capture medication commonly used by clinicians to treat sleep problems. Other sedative medications such as antipsychotics were discussed but excluded since indication for use might be the primary disorder rather than for improvement of sleep.
Patient characteristics
Three patient variables were included:
Age was calculated at time of retrieving the WB and divided into three age categories: 18–24, >24–64, and <64 years. These three age categories were chosen based on the main diagnostic groups to be expected, i.e. young adults with newly debuted major mental disorders and diagnosed neurodevelopmental disorders, adults with mood disorders and longer treatment history as well as older individuals where dementia would be more prevalent.
Sex was defined by the unique personal identifier code issued to each individual at birth or at entrance into the Swedish administrative systems.
Diagnosis was made at a registered visit with health care services according to Chapter V – ‘Mental and behavioural disorders’ in the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) [Citation19]. Included categories were:
Major mental disorders. A hierarchy was constructed for these three categories so that schizophrenia excludes mood disorders and bipolar excludes unipolar and other:
Psychotic disorder including schizophrenia, schizotypal and delusional disorders = F20–F29.
Bipolar disorder = F30–F31.
Unipolar depressive disorder and other mood disorders = F32–F39.
Neurodevelopmental disorders
Autism spectrum disorder (ASD)=F84.
Attention deficit and hyperactivity disorder (ADHD)=F90.
Mental retardation = F70–F79.
Other developmental disorder = F80–F83 and F88–F89.
Other
Organic mental disorders (dementia)=F00–F09.
Anxiety disorders = F40–F41 and F44–F48.
Obsessive-compulsive disorder (OCD)=F42.
Post-traumatic stress disorder (PTSD) and other stress reaction = F43.
Eating disorders = F50.
Personality disorder = F60–F69.
Patients were included if they had received at least one of the above F diagnoses. The categories are based on clinical relevance and grouped together based on the exclusive criteria of major mental disorders within that category.
Substance use
An outcome measure of the rate of SUD, the year prior to WB and the year following inclusion period were defined per three substance categories: alcohol (ICD-10 diagnosis = F10), sedatives (F13) and other (F11–F12 and F14–F19).
Statistics
Pre-age and sex distribution as well as index diagnoses were described using counts and percentages. Pre and post index use of medication was compared using the difference in percentage together with a 95% confidence interval (95%CI) based on a normal approximation and a p value based from a Chi2 test. Pre and post index substance abuse were compared using a mixed logistic regression model with a random effect for each individual accounting for repeated measures. The association between age, gender and pre index diagnoses as independent variables and continued medication was evaluated using a multiple logistic regression model. The doses of those who continued prescription were calculated as the number of prescribed tablets multiplied by the strength of the medication in mg and divided by number of days.
All tests used 5% as the significance level and due to the explorative nature of the study there was no adjustment for multiple comparisons. All analyses were done in SAS® 9.4 (SAS Inc., Cary, NC).
Ethical considerations
The study protocol was reviewed and approved by the regional ethical committee (1122-18/2019-00620). All data used in the study were administrative registered variables collected in databases which were not considered to be harmful or could reveal an individual identity, especially since all analyses were performed using pseudonymized codes.
Results
Demographics
In total, 1785 individuals were included in the study (). There were 72% females and most of the participants were between 25 and 64 years old (69%). The three most common psychiatric diagnoses were anxiety, unipolar depression and ADHD for both sexes and ages up to 65 years (). For the oldest age group, organic mental disorders were most common (67%).
Table 1. Demographics of patients receiving a prescription of weighted blanket in the Region Västa Götaland from April 2015 to January 2018.
Main outcomes of sleep medication use and diagnosis of substance use disorder before and after weighted blanket prescription
Out of the 1785 patients, 1186 (66%) received at least one prescription of the medications included in the study in the year preceding WB (). There was a significant reduction in the rate of prescription for BZRA and antihistamines (p=.02 for both), and also a significant increase in the rate of melatonin prescription (p=.006), as well as in the number of participants without a prescription of the analyzed sleep medications (p=.04). When analyzing odds ratio of continuation of prescriptions, the same rate was observed except for mirtazapine use which was less prevalent ().
Table 2. Main outcomes of sleep medication use and substance use disorder prior and following prescription of weighted blanket (n = 1785).
The year before WB prescription 3.9% had a diagnosis of alcohol use disorder compared to 3.6% the year after, a non-significant difference (). However, there was a statistically significant increase in the proportion of patients with a diagnosis of sedative use disorder by 0.7% with an odds ratio of 1.6 (). Other SUDs were similar in proportion rate prior to and after WB.
Sleep medication use by sex, age and diagnostic category
Comparing between sexes, there was a reduction in the prescription of sleep medication for both women and men ( and Supplementary table 1). However, melatonin increased for women and BZRA was decreased but for men this applied only to antihistamines.
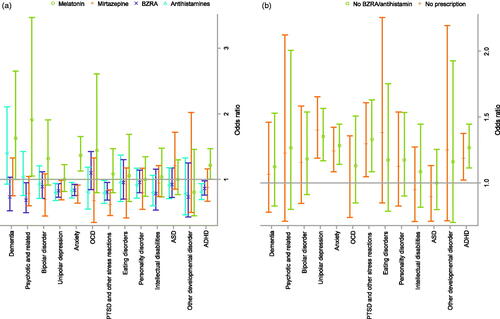
Figure 1. Forest plot of risk for continued prescription of sleep medication before and after weighted blanket by sex and age. (a) Prescribed medication after. (b) No prescription after.
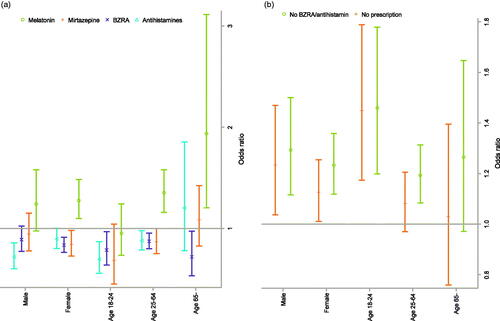
In the youngest age category (18–24 year), the prescription of BZRA and antihistamines decreased. For the middle age group (24–64), the prescription of melatonin increased significantly and higher proportion were without BZRA/antihistamines. For the oldest age group, there was a statistical increase in prescription of melatonin and decrease in BZRA ( and Appendix table 1).
Sleep medication use by diagnosis is presented in and Appendix Supplementary table 2. There was a significant increase in the proportion without a prescribed medication in the year following WB for the participants with unipolar depression, anxiety, ADHD and PTSD.
Multivariate analysis of discontinuation of sleep medication
When analyzing the rate of prescription of either BZRA or antihistamines, a total of 1011 patients received at least one prescription in the year prior to WB and of these 217 (21.5%) did not receive a prescription of these medications in the follow-up period. In a multivariate model, younger age was associated with lower medication use during follow-up, while the diagnoses psychotic disorder, bipolar disorder and personality syndrome were associated an increased risk for continuation of the medication ().
Table 3. Multivariate risk factor analysis for continuing of prescription of sedatives/hypnotics the year after weighted blanket.
Sleep medication doses for continued prescription
Comparing the doses as mg per day before and after the observation time is shown in . The patients who continued their sleep medication did not reduce their doses, rather for melatonin, propiomazine and zopiclone there was a statistically significant increase in dose.
Table 4. Change in amount of sleep medication prior and after prescribed weighted blanket among patients receiving a medical prescription in both periods.
Discussion
Main findings
This register study showed a modest reduction in the use of sleep medications following the prescription of WB, except for melatonin. The factors associated with lower prescription rate were younger age, unipolar depression, anxiety, ADHD and PTSD, while the diagnoses bipolar disorder, psychosis and personality syndrome were associated with a higher risk of continuing BZRA/antihistamines, albeit the rate did not increase in these groups.
Weighted blanket and sleep medication use
In the total population, the increase from 34% to 37% of persons without prescriptions of the studied substances was a significant reduction in the use of medication for sleep problems. This finding should be interpreted with care since the prescription of WB may have been started due to lack of effect or unwanted side-effects of the medication. However, this reduction supports the hypothesis that WB reduces the need for sleep medication. A recent randomized trial showed improved sleep in a population of psychiatric patients [Citation12], where 120 patients received a WB or a non-WB. The primary outcome was the insomnia severity index (ISI, a self-rating scale), that showed a significant reduction in insomnia severity for those receiving a WB, regardless of diagnosis [Citation12]. Furthermore, another recent study showed positive effects of WB on the general anxiety level in oncological patients receiving chemotherapy [Citation13]. The present study may suggest that prescription of WB reduces sleep medication use especially among younger adults, as well as among those diagnosed with unipolar depression, ADHD, PTSD and anxiety.
The reduction in medication use was found to be numerically similar between the sexes. However, melatonin increased significantly for women, while BZRA were reduced. For the men, only antihistamines were significantly reduced. A further difference was that younger patients seem to have reduced sleep medication use albeit numerically this does not increase in the other age groups which might indicate an effect even there. A recent survey showed that younger age and women were at increased risk of road accidents in combination with insomnia and sleep medication [Citation20], emphasizing how important it is to find methods that help these groups. Furthermore, the elderly group is of special importance since there is a lack of safe and effective interventions for insomnia [Citation21] and there is a possibility that the present study lacks power with regards to this age group; however, BZRA were reduced during follow-up.
An important perspective to consider was that the use of melatonin in the general population of the region increased significantly during the study period. The proportion of inhabitants receiving a prescription of melatonin went from 4.2/1000 inhabitants in 2014 to 16.7/1000 inhabitants in 2019 [Citation3]. At the same time, other sleep medications decreased, including BZRA and antihistamines. This might indicate that the reduction of sleep medication found in this study was a part of a general trend in the region, and probably in whole Sweden. Furthermore, one may speculate if WBs were associated with melatonin as a complement to chronotherapeutic way of thinking in clinical practice, that is circadian rhythm regulation. Our results of an increased use of melatonin might suggest such an association.
In the sub-analysis of risk for continued use of BZRA/antihistamines, it is important to note that patients with chronic disorders such as psychotic disorder, bipolar disorder and personality syndrome did not decrease their use, while younger patients did decrease the medication use. This might indicate that WB may be regarded as a possible add-on treatment in the case of patients with chronic disorders but may substitute medication for some patient groups such as anxiety disorders. That is, medication in the chronic disorders group can be part of a prophylactic treatment against severe worsening while for other disorders BZRA/antihistamines may be unnecessary over longer periods.
The outcome of the proportion of participants with SUD is perhaps not surprising. Alcohol SUD was numerically, but not statistically significantly, lower, while the rate of sedative SUD was significantly higher after the study period. The numbers were generally low, both before and after the introduction of a WB, and one can speculate that some patients were recommended WB in order to reduce overconsumption of BZRA, but that the diagnosis was only registered if the patient was unable to reduce the consumption. The increased prevalence of sedative SUD may also suggest that the use of a WB did not influence the patients experienced need for sedatives. Furthermore, the finding that doses tended to increase for those continuing medication use may support that WB might sometimes be prescribed as a treatment method for individuals with overconsumption of BZRA/antihistamines.
Implications
This is the first large epidemiological register study of WB and shows a possible association to a reduced number of participants using sleep medications, and specifically BZRA and antihistamines. In combination with recent controlled trials, the use of WB could be considered as a possibly effective treatment modality for insomnia. However, there is a need for further randomized controlled trials that also measure long-term effects on sleep on a more detailed level.
There is generally a need for research and development of non-invasive physical treatments for sleep disorders that could be used outside the physical health-care environment by the patients themselves. Other examples of non-pharmacological treatments for behavioral changes include neurofeedback, chronotherapy and passive sensing digital data for feedback [Citation22–25]. Perhaps the most established form of psychotherapy, delivered via digital means should even be included as a first-line treatment since it has been shown to have both short- and long-term effect [Citation26]. In this line of thinking, WB may be more seen as part of a general sleep hygiene spectrum or lifestyle that may affect sleep [Citation27].
In a larger sense, since sleep quality is a part of general well-being [Citation28] and if environmental factors such as the weight of nighttime covers can improve well-being, WB might be a cost-effective means of achieving better public health.
Limitations
This is the first large scale epidemiological study investigating the use of WB in a population of patients diagnosed with psychiatric disorder. There is a strength in using objective measures such as prescribed WB, patient characteristics and prescriptions; however, this is also a limitation since there is no possibility to ensure that the administrative data reflect actual medication use or valid diagnoses. This limitation should be interpreted with caution since the registered data reflects how the clinicians make assessments and changes will likely represent an actual trend in real life.
A further limitation is that the design of epidemiological studies cannot define causality. That is, the reason for prescription of WB may be due to lack of response to medication or adverse events which would reduce the use in the follow-up period due to the individual’s prior history.
Conclusion
In conclusion, in this register-based observational study, prescribed WB were associated with a reduced prescription rate of common sleep medications apart from an increase for melatonin. The reduction was especially prominent among younger patients and those diagnosed with unipolar depression, anxiety, PTSD or ADHD; however, younger age was the only factor that was significant in a multivariate model. Future research should focus on identifying which patient groups may gain from WB use and increase the level of evidence since this study and other recent studies are generally promising for this method of treating sleep problems.
Appendices.docx
Download MS Word (36.2 KB)Acknowledgements
The authors wish to thank Gothia Forum for the support and coordination of this project. Especially Emilie Pauli and Anneli Karlsmo, project coordinators. Furthermore, we express our gratitude to Bo Zetterlund and Jan Kilhamn for initiating the Regional process of evaluation weighted blankets as a medical intervention.
Disclosure statement
All authors declare no conflict of interest in the publication of this article.
Additional information
Funding
Notes on contributors
Steinn Steingrímsson
Steinn Steingrímsson, MD, PhD, docent and specialist in psychiatry at Sahlgrenska Academy, University of Gothenburg. Main research focus is on direct environmental effect on psychiatric outcomes with a specific emphasis on digital tools.
Ellen Odéus
Ellen Odéus, PhD student and holds a position as an occupational therapist at Queen Silvia’s Childrens hospital in Gothenburg. Research focus concerns sleeping habits and preconditions to health changes in sleep behaviors in children and adolescents with neuropsychiatric disorders.
Mats Cederlund
Mats Cederlund, MD, PhD, Specialist in Child Neurology and Child Psychiatry, Habilitation & Health, Region Västra Götaland, Sweden.
Stefan Franzén
Stefan Franzén, PhD, Senior statistician at the Centre for Registries, Region Västra Götaland, and adjunct lecturer at the Health Metrics Unit, School of public Heath Göteborg University.
Carina Helgesson
Carina Helgesson, OT, Head of Regional Primary Health Care Unit, Health Care Pharmacy and Medical Aid, Region Västra Götaland, Gothenburg, Sweden.
Kristina Nyström
Kristina Nyström, OT, Strategist Medical Aid, Habilitation & Health, Region Västra Götaland, Gothenburg, Sweden.
John Sondell
John Sondell, data analyst at the department of Data Management and Analysis, Head Office, Region Västra Götaland, Gothenburg, Sweden.
Arve Opheim
Arve Opheim, PT PhD, Head of research and development at Habilitation & Health, Region Västra Götaland, Sweden and leader of research group “Movement and function” at Sunnaas Rehabilitation Hospital, Norway. Main research interests in neurologic rehabilitation, disability and health care.
References
- Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105.
- Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700.
- The National Board of Health and Welfare; 2020. Available from: https://www.socialstyrelsen.se/en/
- Mullen B, Champagne T, Krishnamurty S, et al. Exploring the safety and therapeutic effects of deep pressure stimulation using a weighted blanket. Occup Ther Ment Health. 2008;24(1):65–89.
- Champagne T, Mullen B, Dickson D, et al. Evaluating the safety and effectiveness of the weighted blanket with adults during an inpatient mental health hospitalization. Occup Ther Ment Health. 2015;31(3):211–233.
- Danoff-Burg S, Rus HM, Cruz Martir L, et al. Worth the weight: weighted blanket improves sleep and increases relaxation. Sleep. 2020;43(Suppl. 1):A460.
- Chen HY, Yang H, Meng LF, et al. Effect of deep pressure input on parasympathetic system in patients with wisdom tooth surgery. J Formos Med Assoc. 2016;115(10):853–859.
- Chen HY, Yang H, Chi HJ, et al. Physiological effects of deep touch pressure on anxiety alleviation: the weighted blanket approach. J Med Biol Eng. 2013;33(5):463–470.
- Reynolds S, Lane SJ, Mullen B. Effects of deep pressure stimulation on physiological arousal. Am J Occup Ther. 2015;69(3):6903350010p1–6903350010p5.
- Pereira SI, Beijamini F, Weber FD, et al. Tactile stimulation during sleep alters slow oscillation and spindle densities but not motor skill. Physiol Behav. 2017;169:59–68.
- Lindstedt H, Umb-Carlsson O. Cognitive assistive technology and professional support in everyday life for adults with ADHD. Disabil Rehabil Assist Technol. 2013;8(5):402–408.
- Ekholm B, Spulber S, Adler M. A randomized controlled study of weighted chain blankets for insomnia in psychiatric disorders. J Clin Sleep Med. 2020;16(9):1567–1577.
- Vinson J, Powers J, Mosesso K. Weighted blankets: anxiety reduction in adult patients receiving chemotherapy. Clin J Oncol Nurs. 2020;24(4):360–368.
- Eron K, Kohnert L, Watters A, et al. Weighted blanket use: a systematic review. Am J Occup Ther. 2020;74(2):7402205010p1–7402205010p14.
- Sakshaug S, Handal M, Hjellvik V, et al. Long-term use of Z-hypnotics and co-medication with benzodiazepines and opioids. Basic Clin Pharmacol Toxicol. 2017;120(3):292–298.
- Istvan M, Caillet P, Rousselet M, et al. Change in the regulatory framework for zolpidem: what is the impact on the landscape of the prescription of sedative medications? The French national ZORRO study. Br J Clin Pharmacol. 2021.
- Chakravorty S, Vandrey RG, He S, et al. Sleep management among patients with substance use disorders. Med Clin North Am. 2018;102(4):733–743.
- Statistics Sweden; 2019. Available from: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/population/population-composition/population-statistics/pong/tables-and-graphs/quarterly-population-statistics-municipalities-counties-and-the-whole-country/quarter-1-2019/
- World Health Organisation. International statistical classification of diseases and related health problems. 10th ed. Geneva (Switzerland): World Health Organisation; 2015.
- Morin CM, Altena E, Ivers H, et al. Insomnia, hypnotic use, and road collisions: a population-based, 5-year cohort study. Sleep. 2020;43(8):zsaa032.
- Samara MT, Huhn M, Chiocchia V, et al. Efficacy, acceptability, and tolerability of all available treatments for insomnia in the elderly: a systematic review and network meta-analysis. Acta Psychiatr Scand. 2020;142(1):6–17.
- Steingrimsson S, Bilonic G, Ekelund A-C, et al. Electroencephalography-based neurofeedback as treatment for post-traumatic stress disorder: a systematic review and meta-analysis. Eur Psychiatry. 2020;63:e7.
- Ioannou M, Wartenberg C, Greenbrook JTV, et al. Sleep deprivation as treatment for depression: systematic review and meta‐analysis. Acta Psychiatr Scand. 2021;143(1):22–35.
- Adler DA, Ben-Zeev D, Tseng VW-S, et al. Predicting early warning signs of psychotic relapse from passive sensing data: an approach using encoder–decoder neural networks. JMIR Mhealth Uhealth. 2020;8(8):e19962.
- Steare T, O’Hanlon P, Eskinazi M, et al. Smartphone-delivered self-management for first-episode psychosis: the ARIES feasibility randomised controlled trial. BMJ Open. 2020;10(8):e034927.
- Blom K, Jernelöv S, Rück C, et al. Three-year follow-up of insomnia and hypnotics after controlled internet treatment for insomnia. Sleep. 2016;39(6):1267–1274.
- Kim H, Kim J, Ju HJ, et al. Effect of forest therapy for menopausal women with insomnia. Int J Environ Res Public Health. 2020;17(18):6548.
- Tang NKY, Fiecas M, Afolalu EF, et al. Changes in sleep duration, quality, and medication use are prospectively associated with health and well-being: analysis of the UK Household Longitudinal Study. Sleep. 2017;40(3):zsw079.