Abstract
Background
The societal shutdown due to the Covid-19 pandemic involved mental health services for personality disorder (PD) and was introduced from 12 March 2020 in Norway. Rapid implementation of treatment modifications was required for patients typically characterized by insecure attachment and vulnerability to separation.
Aim
To investigate immediate reactions to the shutdown of services; alternative treatment received; and differences related to age in a clinical sample of patients with PD.
Design
A survey performed from June to October 2020 (after the first Covid-19 wave) among 1120 patients from 12 units offering comprehensive group-based PD programs.
Results
The response-rate was 12% (N = 133). Negative feelings of anxiety, sadness, and helplessness were noteworthy immediate reactions, but the dominating attitude was accommodation. Younger patients (<26 years) reported more skepticism and less relief. Modified treatment was mainly telephone therapy. Digital therapy was less available, but was more frequent among younger patients. A minority received digital group therapy. Most patients rated the frequency and quality of modified treatments as satisfactory in the given situation, but also worried about own treatment progress, lack of group therapy, and 47% missed seeing the therapist when having telephone consultations.
Conclusion
The survey confirms a radical modification from comprehensive group-based PD programs to telephone consultations, low availability of digital consultations and group treatments. Taking a short-term, first wave perspective, the survey indicates a noteworthy capacity among poorly functioning patients for accommodating to a clearly challenging situation, as well as considerable concern about treatment progress.
Introduction
The coronavirus (Covid-19) outbreak, defined in March 2020 as global pandemic, was rapidly followed by international reports demonstrating considerable challenges to mental health [Citation1] as well as mental health services [Citation2]. Specific concern has been raised about patients with poor personality functioning and enhanced risk of self-destructive behaviors [Citation3]. Within Norwegian mental health services, the first Covid-19 wave led to an abrupt shutdown of face-to-face outpatient consultations and an urgent need for organizing new formats of contact. The present study is based on a sample of patients with personality disorders (PDs) within specialized mental health services and investigates the implementation of alternative contact forms after the official shutdown on March 12.
Features of PD are conceptualized within dimensions of self and interpersonal personality functioning [Citation4,Citation5]. Emotional and relational difficulties like the capacity to trust and connect to other people, may impede regular treatment attendance and a stable treatment alliance [Citation6–10]. In long-term therapies and treatments for PD, the alliance and management of alliance ruptures in early phases of treatment impact adherence and outcomes [Citation11,Citation12]. Studies of adolescents and young adults with PD have in particular, demonstrated considerable attachment insecurity [Citation13,Citation14].
Evidence-based treatments for patients with PD are often multicomponent, encompassing psychoeducation, group- and individual therapies [Citation15–18]. Positive effects of such treatments include emotional stabilization and reduction of destructive behaviors [Citation19]. Therapeutic alliance is an important factor in the change process in PD treatments [Citation20–23]. Due concern is therefore raised about the consequences of Covid-19 and associated discontinuation of treatments [Citation24]. The authors point to the need for sustainable adaptations of delivery systems for mental health care.
Telephone- and digital delivery of treatment represent alternative channels for communication [Citation25] and the pandemic has rapidly expanded the clinical relevance of remote therapy formats. Few clinical studies have focused on PD patients during the Covid-19 restrictions and their response to the transition of treatment formats. However, the transition from ongoing face-to-face therapies to remotely delivered sessions was outlined from the perspective of mentalization-based treatment [Citation26,Citation27]. The authors emphasized adjustments involving several levels; patients, clinicians and teams, to ensure the continuation of treatment. A crucial question is to which extent the treatment context allows further development of the alliance between patient and therapist – the creation of a meaningful therapy process in an extraordinary situation. In this respect, patients’ immediate reaction to abrupt changes of the treatment framework and contact with therapists or groups may be decisive.
A small pilot study of older adults (N = 4), described the transformation of schema-therapy [Citation28], to an intensive online program during the Covid-19 crises [Citation29]. Results indicated therapist satisfaction, acceptable patient adaptation, and adherence to nonverbal online formats, online groups and homework delivered by email. These preliminary results were positively encouraging regarding the potentials of remote interventions. Positive first impressions were also conveyed in a small French study (N = 7) of online adjusted dialectical behavioral therapy [Citation30]. Therapy was delivered by videoconferences and telephone calls, aided by an already established online skills training program [Citation31]. Experiences before and during the eight weeks of Covid-19 confinement were compared. The results indicated that maladaptive behaviors did not increase, despite enhanced mental distress among patients. Therapists and patients were familiar with computerized tools and use of telephone consultations before the pandemic. The authors suggest that this may have facilitated the transition.
An Australian survey was based on clinicians (N = 28) delivering dialectical behavioral therapy when ordinary face-to-face group skills programs were closed [Citation28]. Clinicians experienced a deterioration among patients and increased use of crises services. The authors indicate a need for therapist coaching in use of telehealth interventions, and point out that many patients lacked internet access or privacy at home.
In a larger Spanish study of PD patients in schema therapy (N = 50), the transition to remote therapy implied a considerable reduction of treatment intensity. Digital systems were not available [Citation29]. The study compared clinical severity before the outbreak of Covid-19 and after 2.5 months of alternative treatment. Twenty-minute telephone consultations were given weekly to every second week. Therapists addressed the current situation and used cognitive techniques such as active listening, problem-solving skills, and psychoeducation. Patients’ compliance was high, and after 2.5 months, their severity of condition had not increased. Although the study does not provide detailed investigation of patients’ experiences or longer-term effects, the results signal possible utility of quite simple interventions.
Recent Norwegian studies investigating patients with PD (N = 133) at the time of the first Covid-19 wave, demonstrate considerable mental and social distress among patients [Citation30,Citation31]. More intensive therapist contact after the shutdown was associated with having self-harming behaviors before the shutdown, depression, and more severe personality problems. In line with the previously referred studies, self-destructive behaviors did not increase in the investigation period after the shutdown of regular services [Citation30].
The current study is based on the same survey [Citation30] and focuses on the maintenance of therapy during the first Covid-19 wave. It includes patients with PD in a specialized treatment situation at the time of the shutdown of services in Norway. The primary aim was to investigate patients’ immediate reactions to the shutdown of services and the alternative treatment received. Secondarily, as treatment alliance may be more vulnerable among younger patients, the study also aimed to investigate differences associated with younger age.
Materials and methods
This quantitative study is based on a cross-sectional survey performed in June–October 2020 among patients at treatment units on a secondary, specialist mental health service level. Data collection was finally closed in November 2020. The survey covers the first Covid-19 wave in Norway where the restriction period started on March 12. Health services were to a large extent opened up again from mid-May, although society had several remaining restrictions.
Treatment units, assessment procedures and treatment approaches
All patients invited to the survey had been referred to a treatment unit providing specialized treatment for PD. These units were a part of the Norwegian Network for Personality Disorders (The Network) – an ongoing clinical and research collaboration within specialist mental health services in Norway [Citation32]. Currently, the network includes 17 treatment units from all health regions in Norway, the largest representation within southern regions. Altogether, 12 units agreed to participate in this survey. The network units include patients with a broad range of PDs. All therapists are trained in systematic interviews for diagnostic evaluation; MINI for symptom disorders [Citation33] and for PDs, SCID-5-PD [Citation34]. The network provides a standard collection of self-reports for clinical evaluation and advises open feedback procedures to patients on self-reports and diagnostic assessments. The units comprise multidisciplinary therapist teams (psychiatric nurses, social workers, occupational therapists, psychologists, and psychiatrists). Under regular circumstances, specialized approaches include manualized PD treatment programs combining modalities (individual, group and psychoeducation) and more individualized combinations of groups and individual therapies ().
Table 1. Overview of treatment within the Norwegian Network for Personality Disorders.
The survey
The survey was developed in a multidisciplinary work group with researchers, clinicians, and users. It is basis for several studies, qualitative and quantitative [Citation30,Citation31,Citation35]. demonstrates all topics and instruments included in the survey. The main focus in the present study was the treatment situation.
Table 2. Overview of the survey.
Survey-specific items:
Treatment before March 12 (answer options: initial assessment, in psychotherapy, planning to end treatment), duration (months) and type of treatment (answer options: individual, psychotherapy, group psychotherapy, medication).
Diagnoses received on initial assessment before starting PD treatment (answer options: avoidant PD, borderline PD, other PD, unknown). The answer options were based on data from the network concerning the most frequently accounted PDs [Citation40]. Symptom disorders were first confirmed or rejected (yes/no). If yes, specification included options of mood disorders, anxiety disorders, OCD, eating disorders, PTSD, substance use disorder, autism, psychosis, other, and unknown.
Immediate emotional reactions to the shut-down of regular treatment (answer options included a list of emotional states (), and enquiry about change in negative emotional reactions (answer options: reduced, the same, stronger).
Treatment after March 12: (a) telephone consultations (answer option yes/no), time until first telephone (weeks). (b) Digital consultations, individual/group (answer option yes/no), and time until first individual/group digital consultation (weeks). (c) Physical face-to-face consultations, individual/group (answer option yes/no), and time until first individual/group physical face-to-face (weeks).
Not received any consultations after March 12 (answer option yes/no).
Experiences of therapy:
Frequency of contact (answer options: no contact, less than once a month, once a month, every second week, once a week, twice a week or more), regularity/quality/purpose of sessions, and comparison to before March 12 (options: less frequent/worse, unchanged, more frequent/better).
Experience of telephone calls (options: intruding, all right, supportive), and not seeing the therapist (options: difficult, all right, an advantage).
Privacy concerns in remote therapies (options: no, not always, usually).
Satisfaction (options: dissatisfied, acceptable in the current situation, very satisfied).
Missing group therapy (options: no, quite a bit, a lot), thinking about group members (options: a little, quite a bit, very often), worrying about group members (options: a little, quite a bit, a lot).
Concerned about own treatment (options: not worried, quite a bit, very).
Table 3. Patients’ immediate emotional reaction to the changed treatment situation.
Subjects
Twelve treatment units from the network of personality disorders participated by distributing questionnaires to 1120 patients mainly by mail. A total of 133 patients responded by sending a filled in questionnaire by prepaid mail to the research center (response rate 12%). The survey was independent from other assessment routines within the network and anonymous. Data from survey responders could not be linked to other data collected within the network.
Survey responders as compared to the recruitment sample as a whole
To investigate how well survey responders (the study sample, N = 133) represented a clinical sample of patients with PD, we compared information from the study sample to former pretreatment assessments of network patients (data collected 2017–2019, N = 1609) (). Both samples consisted of adults with considerable occupational impairment, the majority were females, avoidant and borderline PD were the two dominating PDs, and comorbid symptom disorders were frequent. The differences in sum-scores of LPFS-BF [Citation41], measuring level of personality functioning, were non-significant (p> .05). On a global 0–100 score of health-related life-quality (EQ-5D [Citation39], survey patients rated themselves at a low, but somewhat higher level than the network sample. The study sample also recruited somewhat older patients, more females, larger proportions living in a close relationship, more frequent diagnoses of borderline PD and/or PTSD, and less frequent mood and substance use disorders (all p< .05).
Ethics
Procedures for data collection were approved by the Norwegian Regional Ethics Committee, given local approvals from all contributing units, and approval of data security procedures at the survey center (Oslo University Hospital). Patients received written information on the project. Participants filled in the questionnaire and returned it directly, in anonymous form, to the project center.
Statistics
Statistics were performed with the IBM SPSS Statistics for Windows, Release 27 (Armonk, NY) [Citation42]. Descriptive data are given as percentages (%) and mean values with standard deviations (SD). Pearson's chi-squared test was performed for comparison of categorical variables and independent samples t-tests for continuous variables. A dichotomous variable differentiated between patients 18 and 25 years of age and 26 years or older. In the presentation of immediate reactions (), a mean sum-score combining the responses ‘clearly’ and ‘partly’ was calculated for positive responses (12 items) and negative responses (three items). Positive and negative mean sum-scores were compared by paired samples t-tests.
Table 4. Clinical status before 12 March 2020.
Results
Sample description
The study sample consisted of mainly females, 31% were less than 26 years (). More than half the sample had less than 50% work/study activity six months before March 12. Scores of personality functioning reflected a majority with personality problems indicative of PD (81% rating LPFS-BF ≥12). The study recruited patients in different phases of referral/treatment (). Fourteen percent were in an introductory phase of pretreatment assessment, 83% in an ongoing treatment process, and 20% had current plans for treatment termination. A larger proportion of patients in the younger age group (<26 years) reported being in treatment for PD on March 12 (98% versus 77%, p= .004). Before March 12, the mean number of months in contact with the treatment unit was 16 (SD 14, range 0–96), 27% reported 6 months or less (mean months in contact: 3, SD 2). Eighty-one percent had received individual psychotherapy, 69% had received group psychotherapy, and 51% had received pharmacological treatment before March 12. At the time of the survey, 19% reported less medication, 68% unchanged and 12% received more.
Patients’ emotional reactions when regular outpatient treatment was shut down
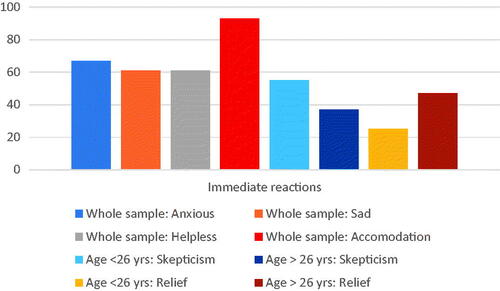
Dominating negative feeling states in the whole sample (confirmed clearly or partly) were ‘anxious’ (67%), ‘sad’ (61%) or ‘helpless’ (61%). The most highly recognized reaction in the sample was an ‘accommodating’ attitude – clearly or partly confirmed in 93%. Only 30% confirmed a reaction of anger, partly or clearly. The mean sum-score of the 12 negative feelings (0.39, SD 0.3) was significantly lower than the mean sum-score of the 3 positive feelings (0.55, SD 0.3) (p= .001). The overall distribution of positive, indifferent, and negative feelings was irrespective of age (p> .05). Feelings of skepticism were more acknowledged in the younger age group (p= .05) and fewer reported feelings of relief (p= .02). At the time of the survey, 37% reported that the immediate reaction was unchanged, while 61% reported a decline. Five patients did not answer this part of the survey (total N = 128). All answer options and ratings are demonstrated in and main results illustrated in .
The modified treatment alternatives
Frequency of contact
Compared to before March 12, 29% reported less frequent contact with their therapist, 14% more frequent, and 57% unchanged. After March 12, 63% percent of the sample had received consultations (any format) with a therapist every week or more, 28% every second week and 9% monthly or less. Seven percent had more than weekly sessions. Four patients reported no contact with a therapist. Frequencies of contact after March 12 did not differ by age groups (p> .05).
Implementation of telephone consultations
Telephone was the main and most rapidly implemented form of alternative contact, and was given to 95% of the sample (89% accepted) after a mean of 2.2 weeks (median 2, SD 1.8, minimum 0, maximum 10) (). Thirty-two percent of the total sample had received a telephone within a week. The proportion patients receiving telephone consultation, and the number of weeks before receiving the first telephone consultation, did not differ by age group (p> .05).
Figure 2. Implementation of alternative therapy formats. The different formats of therapy available to patients before and after March 12, blue and red columns indicate proportions within the two age groups and significant differences in face-to-face and digital therapies (p<.05). Green columns indicate individual and group therapy received.
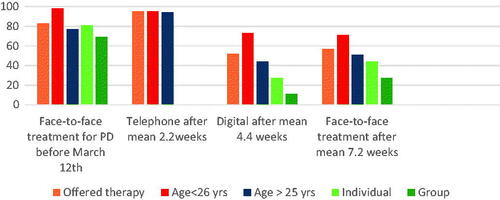
Implementation of digital consultations
Digital consultations took longer time to implement, were not available to all, but offered to a total of 52% in the investigation period (75% accepted) (). Digital consultations were more frequently offered to the younger age group (p= .002) ().
Twenty-seven percent of the total sample confirmed digital individual sessions after a mean of 3.9 weeks (median 3, SD 2.6, minimum 1, maximum 11). Five percent of the total sample had an individual digital session within a week. Digital group consultations were infrequent. Only 11% (15 patients) confirmed digital group therapy sessions after a mean of 4.8 weeks (median 5, SD 2.7, minimum 1, maximum 10). Two percent of the total sample had a digital group session within a week. The number of weeks before receiving the first digital consultation did not differ by age group (p> .05). Fourteen of the 15 patients reporting digital group therapy, had also received telephone consultations in the investigation period and eight of the patients reported a combination of digital individual and group therapy.
Face-to-face consultations at the clinics
Fifty-seven percent of the sample was offered physical, face-to-face sessions at the clinic in the investigation period after March 12 (97% accepted) (). Outpatient individual sessions at the clinic were given to 44% after a mean of 6.6 weeks (median 7, SD 3.3, minimum 0, maximum 15). Two percent of the total sample (three patients) reported a face-to-face, individual session at the clinic within a week. Twenty-seven percent attended group psychotherapy at the clinic after a mean of 7.8 weeks (median 8, SD 2.8, minimum 1, maximum 12). One patient reported having received a group session at the clinic within a week after March 12. Physical face-to-face sessions were more frequent among younger patients (p= .04) ().
Two patients did not answer any questions in this part of the survey (total N = 131).
Patients’ experience of the modified, alternative treatment format
Satisfaction with therapists’ management after March 12 () was rated ‘acceptable in the current situation’ among 58%, high for 37% and low for 5%. These trends were evident across age groups (p> .05). Patients who had been in treatment less than 6 months reported less satisfaction (p= .04). Few patients (8%) had consistent difficulties finding private, undisturbed settings for telephone or digital sessions. The majority reported seldom or no privacy concerns. Results were evident across age groups (p> .05).
Figure 3. Experience of alternative formats. Patients’ overall satisfaction with therapist contact and treatment (intermediate = acceptable), experienced quality and purpose (intermediate = unchanged), privacy concerns (intermediate = yes, sometimes), the remote telephone-format (intermediate = acceptable), and worry about continuity of group-based treatment (intermediate = yes, partly).
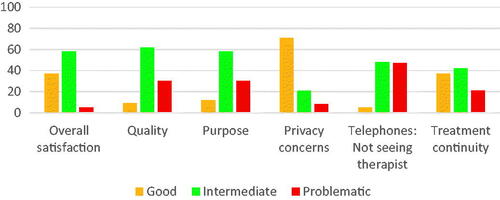
Telephone calls from the therapist were experienced as acceptable in the current situation by 46% and supportive by 48%. Most patients (88%) preferred being called up by the therapist as compared to telephoning the therapists themselves. Although many (73%) felt compelled/quite compelled to answer such telephone calls, few experienced them as intrusive (7%). Forty-seven percent reported that not seeing the therapist during the telephone session was difficult (). Results were irrespective of age (p> .05).
Sixty-nine percent reported that the regularity of individual sessions was unchanged, and 55% had sessions on preset days and times. Fifty-six percent stated that having sessions regularly was important to them. A majority experienced unchanged quality (62%) and purpose (58%) of the individual sessions (). Thirty percent reported deteriorated quality, and 9% described improved quality. Thirty percent experienced the sessions as less meaningful and 12% as more. Results were consistent across age groups (p> .05).
Sixty-one percent of patients participating in group therapy before March 12 were partly or clearly worried about their own treatment and the discontinuation of group sessions (). Large proportions reported; missing the group (70%); thinking about group members often (70%); and worrying about group members (57%). These trends were irrespective of differences in age (p> .05).
A total of 126 patients who had experienced telephone or digital sessions answered this part of the survey.
Discussion
This study recruited patients from specialized PD treatment units within mental health services. As demographic data demonstrate, the sample carries a high burden of distress and impairment of personality functioning – comparable to other descriptions of poorly functioning patients with PD [Citation43]. Such burden represents considerable clinical and personal vulnerability [Citation44] effecting treatment processes [Citation45–47] and treatment ruptures [Citation12]. As one of few PD specific studies, the present investigation addresses the extraordinary situation of treatment interruption inflicted by the global Covid-19 pandemic. The main findings are:
Immediate reactions were mixed, including noteworthy anxiety, sadness, and helplessness as well as high levels of accommodation. Younger patients reported more skepticism and less relief.
Therapist contact was largely maintained by telephone consultations. Digital sessions took longer time to implement and were not generally available. Few received digital group therapy or physical face-to-face consultations. Digital and physical, face-to-face consultations were more frequent among younger patients.
Irrespective of age, a large proportion found therapy quality and purpose satisfactory in the given situation. Privacy concerns were seldom reported. The majority also expressed concern about their treatment progress and the lack of group therapy, and nearly half the sample missed seeing the therapist when having telephone consultations.
Anxiety, sadness, and helplessness coupled with accommodating attitudes
Affective instability, emotional negativity, and persistent feelings of sadness and anxiety are central self-aspects of PD [Citation48–50]. Relational problems may include dependency of others or sensitivity to rejection [Citation51,Citation52]. As could be anticipated, such vulnerability was reflected in patients’ immediate reactions when faced with the shut-down of services. Patients’ negative reactions demonstrate that this abrupt, top-down inflicted situation, was difficult. However, few reported anger, a reaction which also could have been expected [Citation53,Citation54]. Lack of trust or skepticism was likewise, not dominating. On the contrary, a major and striking finding was the large proportion signaling understanding and compliance to the situation. In this early phase of the pandemic, there were little signs of protest and accordingly, few immediate indications of a detrimental break in the collaborative treatment alliance.
Regularity of contact, but not a multicomponent therapy program
Regularity of contact was maintained using the simplest and most readily available channel; telephone, and such consultations were possible from an early stage. Hence, the majority were effectively offered an alternative treatment contact after March 12. In line with other corresponding descriptions of treatments adjustments [Citation29], it is a noteworthy finding that the simple format of telephone consultations was successful as a rapidly implemented intervention platform. It is also an important and perhaps, essential observation of this sample, that frequency of therapist contact was largely, unchanged by the crises [Citation30].
The study demonstrates less effective implementation of digital systems. Such remote channels for the continuation of therapy processes were only marginally able to substitute telephones. The implementation of digital systems within health services involves several organizational levels. If not already prepared, such may not be a rapid process. It is likely that many of the treatment teams had not used such systems before. Other studies have indicated that former experience with such formats facilitated more efficient use of remote therapies during times of restriction [Citation55]. It might also be especially challenging to shift to a digital format for psychodynamic groups as compared to more structured and individual treatments.
The main alternative treatment offered patients lacked the central interpersonal ingredient of specialized PD treatments – group psychotherapy [Citation17, Citation56]. The multicomponent, group-based treatment programs were generally not maintained. In this study, patients quite consistently reported missing groups and group members and worried about their treatment progress. The significance of the group process is emphasized in treatments addressing core aspects of personality functioning [Citation57]. In a longer-term perspective, a lack of group interventions could severely impact treatment effects.
Reestablishment of the full-scale face-to-face program when society gradually opened more up, was slow. Reasons for this can be that outpatient units within hospitals needed time to establish routines and locations fit for new requirements for infection control effecting waiting areas and the size of therapy and other meeting rooms.
Ethical and security issues
Therapy was received in a diversity of arenas (at home, outside, etc.), but in contrast to other reports [Citation28], privacy issues were seldom reported. Increased access to psychotherapy is an obvious advantage, but use of digital systems nonetheless, raises several ethical issues including confidentiality and security, therapist competence, emergency issues, and not least lack of research on effectiveness for patients with PD [Citation58]. Although hybrid solutions are described, digital treatments and guidelines for use of such technology are as yet, not well documented for patients with PDs [Citation25].
Conditional satisfaction, but concern about progress
Patients’ overall satisfaction with a dramatically simplified treatment, was more homogenous and positive than expected. Generally, studies depicting organizational changes and disruptions of treatment teams, report significant barriers to the delivery of effective treatment [Citation59,Citation60]. Along this line, it is an important and perhaps, essential observation that frequency of therapist contact was largely, unchanged by the crises [Citation30]. However, in the qualitative study, patients indicated conditional treatment satisfaction – as temporary solutions in a short period [Citation31]. Retrospectively, societal shutdowns due to Covid-19 restrictions have fluctuated and lasted for a considerable time. Alongside reports indicating acceptability in the current situation, it is therefore important to highlight shortcomings the respondents also emphasized.
The lack of seeing therapists’ faces complicated the therapy process for many. Personality pathology is often associated with disturbed social cognition [Citation61–63]. Several studies of emotional recognition among patients with borderline PD indicate a biased interpretation of others’ mental states including both hypervigilance to social cues as well as disturbed facial emotion perception [Citation64,Citation65]. Not seeing the therapist may thus give rise to uncertainty, misperceptions, misunderstandings, and even paranoid ideation [Citation31]. Knowing that one cannot be seen by the therapist, may also make it more difficult to fully engage in the process. Such problems can be specifically addressed and worked on in therapies using remote formats [Citation26]. However, the clearly reported dissatisfaction with the quality and purpose of therapy in the alternative format is an important feedback from approximately one third of the present study sample.
Maintaining alliance
The reciprocal process between patients and therapists is frequently emphasized in psychotherapy. Balancing processes through difficult emotional situations requires skilled therapists [Citation66]. Therapists’ negative countertransference feelings are commonly encountered in treatment of patients with PD [Citation67–70] and in the extraordinary, pandemic situation, such complicated reactions involving both patient and therapist would be understandable. A recent publication addresses the dialogue between therapists and patients in mentalization-based treatment during the pandemic [Citation26]. The case vignettes illustrate the importance of therapist attunement to the current situation where patients’ personality problems were activated by the pandemic. Accommodating attitudes and conditional satisfaction in our study may be linked to an early experience that the therapist made a convincing effort to keep up contact.
Young adults were more vulnerable
Several authors have generally, recommended special consideration of the development of alliance in therapies with adolescents and younger adults [Citation71,Citation72]. In the extraordinary situation of the present study, the trusting relationship seemed more insecure or easily disrupted in the younger age group. This may have been a reason for enhanced frequencies of digital and face-to-face consultations in this subgroup.
Willingness to adapt during a pandemic crisis
In a Canadian population survey, respondents reported high trust in authorities and information given by medias, high compliance to restrictions and social distancing, but considerable concern about health services and own mental health. Forty-nine percent specified worries about worsening social health, 39% mental/emotional health, and 45% reported mental stress related to the pandemic [Citation73]. However, lower acceptance of mitigation measures has been associated with personality traits of extraversion and emotional instability [Citation74].
In contrast to expectations [Citation3], the present survey of patients with PD does not suggest non-compliance, but a largely accommodating attitude. Considering the nature of PD, such capacity for understanding in the difficult situation may be surprising. Several societal factors could contribute to the willingness to adapt. In line with international recommendations, strict and mandatory measures were promoted by Norwegian authorities for management of the pandemic [Citation75]. In a recent study of public compliance, a reasonable fear of infection was emphasized as the most important factor for adherence to restrictions during the Covid-19 pandemic [Citation76]. In our survey-sample, a sizable proportion reported considerable fear of contagion and health-related anxiety [Citation30]. Moreover, despite anxiety, a sense of being less alienated and more a part of the society during the crises situation, was also reported [Citation31]. Although patients’ confidence in authorities and capacity to comply may be different in a prolonged pandemic situation, the combination of affiliation and fear may have facilitated compliance.
Strengths and limitations
Few have been able to investigate experiences of the Covid-19 shutdown among patients with PD in specialized treatment. A study based on an extraordinary, ad hoc, data collection within an established collaborative clinical research network represents a unique opportunity. A clinical sample counting 133 patients, the majority in specialized treatment is a noteworthy effort. The survey was conducted as soon as possible after the decline of the first wave in order to ensure valid experiences. For practical, economical, and time-saving reasons, a simple paper-based survey with response based on postal systems (non-digital) was chosen.
A drawback of the survey timing was that the clinics still had considerable Covid-19 related extra administrative pressure and also, due to summer vacations, less available resources. Use of non-digital paper systems may have heightened the threshold for patient response as well as increased possibilities of missing data due to inaccurate addresses on several levels. Although there was generally high motivation to participate among network units, such may have contributed to low response rate.
Dominating positive attitudes reflected in the sample could be a social desirability bias. However, to counteract this possibility, the survey was voluntary and anonymous and delivery of response was completely independent of the treatment units and therapists. Nonetheless, selection bias cannot be ruled out as more satisfied patients could be more prone to answer such a survey.
As the conducted survey was anonymous, data for direct comparison of survey responders with those originally invited to participate were unavailable. However, baseline (pretreatment) data within the network provided possibility for comparing survey responders to a large clinical cohort of patients with PD. This comparison generally supported the survey as a clinical representation of patients with PD. However, baseline network data are not fully comparable to the survey’s mixture of patients in different treatment phases.
The survey represents a first wave of Covid-19. Compared to many other nations, contagion was mild. In this early phase, a recent study has also demonstrated that population levels of mental distress were also less severe [Citation77]. The recruitment of patients referred to specialized treatment may limit the generalizability of the situation for PD patients across nations, contexts, and availability of PD health services.
Information in this study was based on self-report from the survey and information was post hoc, based on patients recollection. The precision of detail may have limitations although we expect that emotional experiences will still have high validity.
Conclusion
This study focuses on patients’ experiences of the radical modifications of comprehensive group-based PD programs induced by Covid-19 first wave restrictions in Norway. Although frequencies of contact with therapists were largely maintained, comprehensive group-based treatment programs suffered due to poor implementation of digital consultation systems. The study indicated a noteworthy capacity for accommodation among patients in a challenging situation although satisfaction was conditional, and younger patients were more vulnerable. In the short-term perspective, rapidly implemented telephone consultations ensured continuity. In a longer-term perspective, the results point to the need for secure, prepared and evidence-based digital treatment systems in order to ensure availability of specialized therapies for PD.
Notes on contributors
All authors collaborate in the research group of Personality Psychiatry, University of Oslo, which is headed by EHK (MD, PhD, associate professor/Head senior consultant, Section for Personality Psychiatry).
EHK has clinical and research experience within differential diagnostic assessment and treatment of patients with personality disorder.
GP (MA, PhD, head of the Norwegian Network for Personality Disorders) has experience within clinical research implementation, and psychometric assessments. EHK and GP are joint principle investigators in this project.
KEZ (MA) is a senior psychologist and represents five of the participating units. KEZ has engaged in clinical research within treatment of patients with personality disorder.
LIS (MA, PhD) is a researcher/senior psychologist. Her main research interests are within qualitative methodology, case studies, and research focusing on self-harming behaviors among adolescents.
MSP (MA) has a Masters degree of Nursing - Clinical Research and Professional Development and works currently within the addiction field. She has experience with qualitative research methods and also represents a user perspective.
ÅLB (BA) works currently as communications advisor at the National Advisory Unit for Personality Psychiatry. She is also engaged in health service implementation, qualitative research and user representation.
MSJ (MD, PhD, head senior consultant) heads one of the participating clinical units. She has clinical and research experience within assessment and treatment of patients with personality disorder.
IU-ME (MD, PhD) is head of the National Advisory Unit for Personality Psychiatry and has clinical and research experience within assessment and treatment of patients with personality disorder.
EAA (MA, PhD) is a clinical psychologist/researcher and head of an addiction research unit. He has clinical and research experience within assessment of patients with personality disorder and a broad range of treatments.
BH (MD, PhD) is a senior consultant/researcher with broad experience of clinical research, project implementation, statistical methodology, diagnostic assessment and treatment of personality disorder.
TW (MD, PhD) is a senior consultant/researcher with broad experience of clinical research, project implementation, psychotherapy research, assessment and treatment of personality disorder.
Acknowledgements
We wish to thank the patients and staff from the Network of Personality Disorders in Norway for their contribution to this study. The 12 participating treatment units include Unit for Group Therapy, Øvre Romerike District Psychiatric Center, Akershus University Hospital, Jessheim; Group Therapy Unit, Nedre Romerike District Psychiatric Center, Akershus University Hospital, Lillestrøm; Group Therapy Unit, Follo District Psychiatric Center, Akershus University Hospital; Group Therapy Unit, Kongsvinger District Psychiatric Center, Akershus University Hospital; Clinic for Personality disorders, Outpatient Clinic for Specialized Treatment of Personality Disorders, Section for Personality psychiatry and specialized treatments, Oslo University Hospital, Oslo; Group Therapy Unit, Lovisenberg District Psychiatric Center, Lovisenberg Hospital, Oslo; Group Therapy Team, Vinderen Psychiatric Center, Diakonhjemmet Hospital, Oslo; Unit of Personality psychiatry, Vestfold District Psychiatric Center; Unit for Intensive Group Therapy, Aust-Agder District Psychiatric Center, Sørlandet Hospital, Arendal; Unit for Group Therapy, District Psychiatric Center, Strømme, Sørlandet Hospital, Kristiansand; Group Therapy Unit, Stavanger District Psychiatric Center, Stavanger University Hospital, Stavanger; Section for group treatment, Kronstad District Psychiatric Center, Haukeland University Hospital, Bergen. We also acknowledge the efficient research assistance of Elise Bynander, Outpatient Clinic for Specialized Treatment of Personality Disorders, Section for Personality psychiatry and specialized treatments, Oslo University Hospital, Oslo.
Disclosure statement
None of the above authors have any financial disclosure or other conflicts of interest related to this study. Data collection was funded by Oslo University Hospital.
Data availability statement
A data set is not directly available, but data can be made available upon specified request to the main, corresponding author/principal investigator/last author Geir Pedersen. However, this will require additional application for ethical approval by the board for medical research ethics, South Eastern Norway.
References
- Lakhan R, Agrawal A, Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J Neurosci Rural Pract. 2020;11(4):519–525.
- Li W, Yang Y, Liu ZH, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732–1738.
- Preti E, Di Pierro R, Fanti E, et al. Personality disorders in time of pandemic. Curr Psychiatry Rep. 2020;22(12):80.
- Bender DS, Morey LC, Skodol AE. Toward a model for assessing level of personality functioning in DSM-5, part I: a review of theory and methods. J Pers Assess. 2011;93(4):332–346.
- Hutsebaut J, Feenstra DJ, Kamphuis JH. Development and preliminary psychometric evaluation of a Brief Self-Report Questionnaire for the assessment of the DSM-5 level of Personality Functioning Scale: the LPFS Brief Form (LPFS-BF). Personal Disord. 2016;7(2):192–197.
- Barnicot K, Katsakou C, Marougka S, et al. Treatment completion in psychotherapy for borderline personality disorder: a systematic review and meta-analysis. Acta Psychiatr Scand. 2011;123(5):327–338.
- Busmann M, Wrege J, Meyer AH, et al. Alternative model of personality disorders (DSM-5) predicts dropout in inpatient psychotherapy for patients with personality disorder. Front Psychol. 2019;10:952.
- Horz S, Zanarini MC, Frankenburg FR, et al. Ten-year use of mental health services by patients with borderline personality disorder and with other axis II disorders. Psychiatr Serv. 2010;61(6):612–616.
- Holth F, Walby F, Røstbakken T, et al. Extreme challenges – psychiatric inpatients with severe self-harming behavior in Norway – a national screening investigation. Nord J Psychiatry. 2018;72(8):605–612.
- Euler S, Wrege J, Busmann M, et al. Exclusion-proneness in borderline personality disorder inpatients impairs alliance in mentalization-based group therapy. Front Psychol. 2018;9:824.
- Sharf J, Primavera LH, Diener MJ. Dropout and therapeutic alliance: a meta-analysis of adult individual psychotherapy. Psychotherapy (Chic). 2010;47(4):637–645.
- Schenk N, Furer L, Zimmermann R, et al. Alliance ruptures and resolutions in personality disorders. Curr Psychiatry Rep. 2020;23(1):1.
- Hauber K, Boon A, Kuipers G, et al. Adolescent attachment insecurity and the influence of MBT. Attach Hum Dev. 2020;22(2):157–173.
- Khoury JE, Zona K, Bertha E, et al. Disorganized attachment interactions among young adults with borderline personality disorder, other diagnoses, and no diagnosis. J Pers Disord. 2020;34(6):764–784.
- Livesley J. Integrated therapy for complex cases of personality disorder. J Clin Psychol. 2008;64(2):207–221.
- Ridolfi ME, Gunderson JG. Psychoeducation for patients with borderline personality disorder. In: Livesley WJ, Larstone R, editors. Handbook of personality disorders: theory, research, and treatment. New York (NY): The Guilford Press; 2018. p. 600–610.
- McLaughlin SPB, Barkowski S, Burlingame GM, et al. Group psychotherapy for borderline personality disorder: a meta-analysis of randomized-controlled trials. Psychotherapy. 2019;56(2):260–273.
- Swenson CR, Choi-Kain LW. Mentalization and dialectical behavior therapy. Am J Psychother. 2015;69(2):199–217.
- Storebo OJ, Stoffers-Winterling JM, Vollm BA, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5:CD012955.
- Dimaggio G, Maillard P, MacBeth A, et al. Effects of therapeutic alliance and metacognition on outcome in a brief psychological treatment for borderline personality disorder. Psychiatry. 2019;82(2):143–157.
- Folmo E, Karterud S, Kongerslev M, et al. Battles of the comfort zone: modelling therapeutic strategy, alliance and epistemic trust – a qualitative study of mentalization-based therapy for borderline personality disorder. J Contemp Psychother. 2019;49(3):141–151.
- Rudge S, Feigenbaum JD, Fonagy P. Mechanisms of change in dialectical behaviour therapy and cognitive behaviour therapy for borderline personality disorder: a critical review of the literature. J Ment Health. 2020;29(1):92–102.
- Folmo EJ, Stanicke E, Johansen MS, et al. Development of therapeutic alliance in mentalization-based treatment—goals, bonds, and tasks in a specialized treatment for borderline personality disorder. Psychother Res. 2020;31(5):1–15.
- Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824.
- Smith K, Ostinelli E, Macdonald O, et al. COVID-19 and telepsychiatry: development of evidence-based guidance for clinicians. JMIR Ment Health. 2020;7(8):e21108.
- Wurman TV, Lee T, Bateman A, et al. Clinical management of common presentations of patients diagnosed with BPD during the COVID-19 pandemic: the contribution of the MBT framework. Counsel Psychology Quart. 2020.
- Daubney M, Bateman A. Mentalization-based therapy (MBT): an overview. Aust Psychiatry. 2015;23(2):132–135.
- Lakeman R, Crighton J. The impact of social distancing on people with borderline personality disorder: the views of dialectical behavioural therapists. Issues Ment Health Nurs. 2020;42(5):1–7.
- Álvaroa F, Navarroa S, Palmaa C, et al. Clinical course and predictors in patients with borderline personality disorder during the COVID-19 outbreak: a 2.5-month naturalistic exploratory study in Spain. Psychiatr Res. 2020;292:113306.
- Kvarstein E,H, Zahl KE, Stänicke LI, et al. Vulnerability of personality disorder during the Covid-19 crises – a multicenter survey of mental and social distress among patients referred to treatment; Nordic J Psychiatry; 2021.
- Stänicke LI, Arnevik EA, Pettersen MS, et al. The importance of feeling remembered and cared for during the Covid-19 crisis – a qualitative multi-center survey of everyday life and treatment experiences among vulnerable patients with a personality disorder; submitted for publication; 2021.
- Karterud S, Pedersen G, Bjordal E, et al. Day treatment of patients with personality disorders: experiences from a Norwegian treatment research network. J Pers Disord. 2003;17(3):243–262.
- Sheehan DV, Lecrubier Y, Janavs J, et al. Mini International Neuropsychiatric Interview (M.I.N.I.). Tampa (FL) and Paris: University of South Florida Institute for Research in Psychiatry and INSERM-Hôpital de la Salpétrière; 1994.
- First MB, Williams JBW, Benjamin LS, et al. User’s guide for the SCID-5-PD (structured clinical interview for DSM-5 personality disorder). Arlington (VA): American Psychiatric Association; 2016.
- Zahl KP, Eikenaes IUM, Stänicke LI, et al. Patients with borderline and avoidant personality disorders and their reactions to the Covid-19 crisis; submitted for publication; 2021.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097.
- Yudofsky SC, Silver JM, Jackson W, et al. The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am J Psychiatry. 1986;143(1):35–39.
- van Asselt AD, Dirksen CD, Arntz A, et al. The EQ-5D: a useful quality of life measure in borderline personality disorder? Eur Psychiatry. 2009;24(2):79–85. DOI: https://doi.org/10.1016/j.eurpsy.2008.11.001
- Kvarstein E, Karterud S. Large variation of severity and longitudinal change of symptom distress among patients with personality disorders. Personal Ment Health. 2013;7(4):265–276.
- Bach B, Hutsebaut J. Level of Personality Functioning Scale-Brief Form 2.0: utility in capturing personality problems in psychiatric outpatients and incarcerated addicts. J Pers Assess. 2018;100(6):660–670.
- IBM Corp., inventor. IBM SPSS statistics for Windows, version 27. Armonk (NY); 2020.
- Soeteman DI, Verheul R, Busschbach JJ. The burden of disease in personality disorders: diagnosis-specific quality of life. J Pers Disord. 2008;22(3):259–268.
- Sorensen KD, Rabu M, Wilberg T, et al. Struggling to be a person: lived experience of avoidant personality disorder. J Clin Psychol. 2019;75(4):664–680.
- Katsakou C, Pistrang N. Clients' experiences of treatment and recovery in borderline personality disorder: a meta-synthesis of qualitative studies. Psychother Res. 2018;28(6):940–957.
- Kverme B, Natvik E, Veseth M, et al. Moving toward connectedness – a qualitative study of recovery processes for people with borderline personality disorder. Front Psychol. 2019;10:430.
- Ng FYY, Townsend ML, Miller CE, et al. The lived experience of recovery in borderline personality disorder: a qualitative study. Borderline Personal Disord Emot Dysregul. 2019;6:10.
- Reisch T, Ebner-Priemer UW, Tschacher W, et al. Sequences of emotions in patients with borderline personality disorder. Acta Psychiatr Scand. 2008;118(1):42–48.
- Jacob GA, Hellstern K, Ower N, et al. Emotional reactions to standardized stimuli in women with borderline personality disorder: stronger negative affect, but no differences in reactivity. J Nerv Ment Dis. 2009;197(11):808–815.
- Snir A, Bar-Kalifa E, Berenson KR, et al. Affective instability as a clinical feature of avoidant personality disorder. Personal Disord. 2017;8(4):389–395.
- Choi-Kain LW, Zanarini MC, Frankenburg FR, et al. A longitudinal study of the 10-year course of interpersonal features in borderline personality disorder. J Pers Disord. 2010;24(3):365–376.
- Meyer B, Ajchenbrenner M, Bowles DP. Sensory sensitivity, attachment experiences, and rejection responses among adults with borderline and avoidant features. J Pers Disord. 2005;19(6):641–658.
- Hummelen B, Wilberg T, Karterud S. Interviews of female patients with borderline personality disorder who dropped out of group psychotherapy. Int J Group Psychother. 2007;57(1):67–91.
- Critchfield KL, Levy KN, Clarkin JF, et al. The relational context of aggression in borderline personality disorder: using adult attachment style to predict forms of hostility. J Clin Psychol. 2008;64(1):67–82.
- Salamin V, Rossier V, Joye D, et al. Adaptations of an outpatient dialectical behavioral therapy during the COVID-19 pandemic and consequences of the confinement on patients with borderline personality disorder. Ann Med Psychol (Paris). 2021;179(2):131–136.
- Uliaszek AA, Hamdullahpur K, Chugani CD, et al. Mechanisms of change in group therapy for treatment-seeking university students. Behav Res Ther. 2018;109:10–17.
- Doorn KA, Kealy D, Ehrenthal JC, et al. Improving self-esteem through integrative group therapy for personality dysfunction: investigating the role of the therapeutic alliance and quality of object relations. J Clin Psychol. 2019;75(12):2079–2094.
- Stoll J, Muller JA, Trachsel M. Ethical issues in online psychotherapy: a narrative review. Front Psychiatry. 2019;10:993.
- Bales DL, Verheul R, Hutsebaut J. Barriers and facilitators to the implementation of mentalization-based treatment (MBT) for borderline personality disorder. Personal Ment Health. 2017;11(2):118–131.
- Hutsebaut J, Bales DL, Busschbach JJ, et al. The implementation of mentalization-based treatment for adolescents: a case study from an organizational, team and therapist perspective. Int J Ment Health Syst. 2012;6(1):10.
- Normann-Eide E, Antonsen BT, Kvarstein EH, et al. Are impairments in theory of mind specific to borderline personality disorder? J Pers Disord. 2020;34(6):827–841.
- Moroni F, Procacci M, Pellecchia G, et al. Mindreading dysfunction in avoidant personality disorder compared with other personality disorders. J Nerv Ment Dis. 2016;204(10):752–757.
- Fonagy P, Bateman AW. Adversity, attachment, and mentalizing. Compr Psychiatry. 2016;64:59–66.
- Domes G, Czieschnek D, Weidler F, et al. Recognition of facial affect in borderline personality disorder. J Pers Disord. 2008;22(2):135–147.
- Fertuck EA, Jekal A, Song I, et al. Enhanced 'Reading the Mind in the Eyes' in borderline personality disorder compared to healthy controls. Psychol Med. 2009;39(12):1979–1988.
- Nissen-Lie HA, Havik OE, Hoglend PA, et al. Patient and therapist perspectives on alliance development: therapists' practice experiences as predictors. Clin Psychol Psychother. 2015;22(4):317–327.
- Rossberg JI, Karterud S, Pedersen G, et al. Specific personality traits evoke different countertransference reactions: an empirical study. J Nerv Ment Disord. 2008;196(9):702–708.
- Rossberg JI, Karterud S, Pedersen G, et al. An empirical study of countertransference reactions toward patients with personality disorders. Compr Psychiatry. 2007;48(3):225–230.
- Dahl HS, Ulberg R, Friis S, et al. Therapists' inadequate feelings and long-term effect of transference work. Psychother Psychosom. 2016;85(5):309–310.
- Dahl HJ, Hoglend P, Ulberg R, et al. Does therapists' disengaged feelings influence the effect of transference work? A study on countertransference. Clin Psychol Psychother. 2017;24(2):462–474.
- Labouliere CD, Reyes JP, Shirk S, et al. Therapeutic alliance with depressed adolescents: predictor or outcome? Disentangling temporal confounds to understand early improvement. J Clin Child Adolesc Psychol. 2017;46(4):600–610.
- Owen J, Miller SD, Seidel J, et al. The working alliance in treatment of military adolescents. J Consult Clin Psychol. 2016;84(3):200–210.
- Leigh JP, Fiest K, Brundin-Mather R, et al. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: self-reported beliefs, knowledge, and behaviors. PLoS One. 2020;15(10):e0241259.
- Nofal AM, Cacciotti G, Lee N. Who complies with COVID-19 transmission mitigation behavioral guidelines? PLoS One. 2020;15(10):e0240396.
- Ayenigbara IO, Adeleke OR, Ayenigbara GO, et al. COVID-19 (SARS-CoV-2) pandemic: fears, facts and preventive measures. Germs. 2020;10(4):218–228.
- Harper CA, Satchell LP, Fido D, et al. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020;1–14.
- Geirdal AO, Ruffolo M, Leung J, et al. Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. J Ment Health. 2021;1–8.