Abstract
Introduction
Malingering can be divided into simulation and exaggeration of symptoms. Malingering has traditionally been considered rare in general psychiatry. In contrast to earlier estimates, more recent studies report that doctors suspect malingering frequently in psychiatric emergency departments. The aim of this study is to survey how often doctors in psychiatric emergency units in a public, free-of-charge, mental health service suspect that patients are malingering, and which diagnoses, symptom complaints and suspected reasons for malingering doctors ascribe to their patients.
Methods
Questionnaires were distributed in three psychiatric emergency departments in Denmark. Suspected simulation and exaggeration were rated with a 5-point scale. Doctors were encouraged to write down the symptoms and perceived causes for suspected malingering.
Results
362 questionnaires were filled in. 25% of all patients were suspected of simulating to some degree. 8% of patients were highly suspected or definitely believed to be simulating. Patients complaining of suicidal ideation were most frequently suspected of malingering. ‘Attention seeking’ was the most common suspected reason for malingering. Patients with diagnoses of substance use and personality disorder were the most suspected of malingering.
Conclusion
This is the first study to investigate doctors’ suspicions of psychiatric malingering in a European setting. Patients with established personality and substance use disorder are at higher risk of being suspected of malingering, which potentially affects the course of treatment significantly. The rise in suspected malingering is conspicuous and requires further investigation. Doctors are encouraged to act conservatively upon suspicion of malingering in emergency psychiatry.
Introduction
Suspicion of malingering appears to have increased during the last decades. As shown in a recent study, up to 20% of patients in an emergency psychiatric department in the United States were strongly suspected of malingering [Citation1], and as many as 42% of patients were suspected of malingering in another American hospital [Citation2].
These high levels of suspicion are in striking contrast to estimates on the prevalence of malingering. The ICD-10 states that: ‘Malingering is comparatively common in legal and military circles, and comparatively uncommon in ordinary civilian life.’ [Citation3]. Kaplan & Sadock's Synopsis of Psychiatry approximates the prevalence of malingering to 10-20% in forensic settings, but only around 1% in general psychiatry [Citation4]. It seems that the prevalence of suspected malingering is much higher than the estimate of malingering proper.
Literature review
The ICD-10 defines malingering as the intentional simulation or significant exaggeration of symptoms specifically motivated by external incentives or rewards: ‘…evading criminal prosecution, obtaining illicit drugs, avoiding military conscription or dangerous military duty, and attempts to obtain sickness benefits or improvements in living conditions such as housing’ [Citation3]. The DSM-5 and ICD-11 have similar definitions of malingering [Citation5,Citation6].
Malingering can be divided into pure malingering (simulation of non-existent symptoms) and partial malingering (exaggeration of already existent symptoms) [Citation7].
The exact prevalence of psychiatric malingering is unknown, as it is in most circumstances not possible to know for sure if patients are making up symptoms. Certainty is not guaranteed, even when patients admit malingering, as dissimulation also occurs [Citation8].
Some authors have based an estimate upon registered malingering in the medical records [Citation9]. However, this approach is problematic as malingering is often not registered, even when suspicions are high [Citation2]. Others have taken doctors’ suspicion of malingering as an actual prevalence [Citation1]. The problem here is that this assessment could be erroneous and an expression of the doctors’ or other staff’s preconceptions.
An older study investigated 173 psychiatrists' attitudes to a vignette case story. The case varied with information about a previous diagnosis of personality disorder. When informed about this, the psychiatrists were significantly more likely to assume the following statements about the patient: ‘Unlikely to arouse sympathy’, ‘Manipulating admission’, ‘Taking an overdose will be attention seeking’, ‘Not mentally ill’, etc. [Citation10]. Likewise, a systematic review by Van Boekel et al. found that health professionals tend to have negative attitudes towards patients with substance use disorders [Citation11].
Two studies by Rissmiller et al. found that 10% [Citation12] and 12% [Citation13] of patients complaining of suicidal ideation reported having feigned or exaggerated their symptoms. Assuming patients responded frankly, malingering could be detected with 100% sensitivity by a psychiatrist and a psychologist. Unfortunately, as the study concluded, the specificity was not better than chance [Citation12].
Another approach to verify suspected malingering is to examine patients’ diagnostic outcomes. Ritson and colleagues examined 12 patients believed to be simulating psychosis. They found that 3 of these patients qualified for a legitimate diagnosis of schizophrenia, while the rest had either personality disorders or personality problems [Citation14]. 20 years later, Humprey et al. were able to trace the long-term outcomes of 10 of the 12 patients described in Ritson’s study. All these patients qualified for psychotic disorders [Citation15]. Likewise, Hay and colleagues followed up on 6 patients discharged with malingering recorded in the medical records. In all but one case, the diagnosis had been changed to a genuine diagnosis of schizophrenia [Citation16]. By contrast, Pope and colleagues’ results point in another direction: They reviewed the charts of 219 patients hospitalised with psychotic symptoms and found that 6.4% of them (n = 14) were probably or definitely feigning. Upon further investigation, 4.1% of patients (n = 9) were assessed to be definitely feigning. They qualified for diagnoses of borderline and histrionic personality disorder. The writers emphasise the poor clinical outcome of these patients [Citation17].
Relevance
Malingering is very difficult to assess, and suspicion of malingering can have far-reaching implications for patients. As e.g. Rumschick and Appel demonstrated, high suspicion of malingering was likely to result in immediate discharge or not being admitted to the psychiatric hospital [Citation1]. This combination of diagnostic difficulties and the prospect of potentially denying an ill patient treatment should call for caution. Moreover, the above-mentioned American studies concerned suspicion of malingering already in the emergency room [Citation1,Citation2].
There is no obvious explanation for this high prevalence of suspected malingering in psychiatry. Thus, we decided to examine if a similar high frequency (i.e. 20–40%) was detectable in European psychiatric emergency units. Although American settings are somewhat dissimilar, we hypothesised a frequency of suspected malingering in the same range.
Aim
The aim of this study is to survey to what degree medical doctors believe that their patients are malingering and to examine which diagnoses, symptom complaints and suspected reasons for malingering doctors ascribe to their patients.
Materials and methods
Participants
Upon arrival at the psychiatric emergency department, patients are evaluated by either a medical student (who is at most one year from graduating) or a medical doctor with variable degrees of psychiatric experience (from junior doctors to consultants). Attending doctors work variable shifts, and there is a high rotation rate of doctors and medical students. A total of 300 doctors and students had shifts during the data collecting period and were able to answer questionnaires.
Setting
The investigated psychiatric emergency wards are always open for both referred and un-referred patients over the age of 18. Treatment is financed through the Danish welfare system. Two of the hospitals have urban localisation (Capital Region) and one is located in a rural area (Region Zealand). An approval from an ethics committee was not required by Danish law or custom. We included data for two 14-days periods in August and November 2020.
We asked all doctors and medical students working in the psychiatric emergency units to evaluate whether they believed that the patient they had just seen had been malingering. Questionnaires and posters with information about the project were visible in each emergency department. We also regularly sent a standard text message to the doctor on duty reminding her or him of the project. As an additional incentive, doctors were encouraged to take a piece of chocolate from a box, each time they filled in a questionnaire.
Definitions
The definitions of simulation and exaggeration attached to our questionnaires were: ‘By simulation, we understand the conscious simulation of symptoms for the purpose of obtaining an external gain. By exaggeration we understand an exaggerated portrayal of the magnitude or intensity of existing symptoms.’
Measures
We asked for the attending doctor’s level of experience and demographic and diagnostic information on the patient. This information was available to the rater through the medical records that also contain information from earlier assessments. We also asked for an assessment of suspected simulation and exaggeration. Answers were recorded in multiple-choice questionnaires. Answers in free text were also allowed.
Suspicion of malingering was assessed with a 5-point scale (not suspected, slightly, moderately, strongly or definitely) developed by Yates and colleagues [Citation2] and recently used in a study by Rumshick [Citation1].
In case of suspected simulation or exaggeration, the respondent was asked to write the relevant symptoms in free text as well as the suspected reasons for malingering. The rater could also encircle one or more of the following reasons for simulation and exaggeration: ‘Food/shelter’, ‘Drug seeking behaviour’, ‘Attention seeking’, and ‘Loneliness’. These options were based upon our experiences from talking with colleagues about the subject.
Analytic strategy
Patients were grouped by their diagnosis according to major ICD-10 diagnostic groups from F10 to F69. Remaining patients were grouped under ‘Other diagnosis’, ‘No previous diagnosis’ and ‘No registered diagnosis’. We collapsed the 5-point scale for suspected malingering into 3 categories: ‘None’, ‘Low to moderate’ and ‘High to certain’. We calculated differences between diagnostic groups with regards to suspected simulation and exaggeration with Pearson’s Chi Square tests.
16 patients were registered with 2 diagnoses. These patients are included in table one and in the above-mentioned analyses with their highest-ranking diagnosis according to the ICD-10 hierarchy. In the following analyses and tables (as well as in the figure) they are included with both of their diagnoses.
We used Pearson’s Chi Square tests to compare suspected simulation and exaggeration between raters with different levels of experience. We used a two tailed Fisher’s exact test to compare patients with diagnoses of substance use and personality disorder with all other patients with regards to suspected simulation and exaggeration. We used one tailed Fisher’s exact tests to see if specific symptoms and reasons for malingering were attributed to patients with substance use and personality disorder more frequently than to other perceived malingerers.
For analysing the data, we used IBM SPSS Statistics 28.
Results
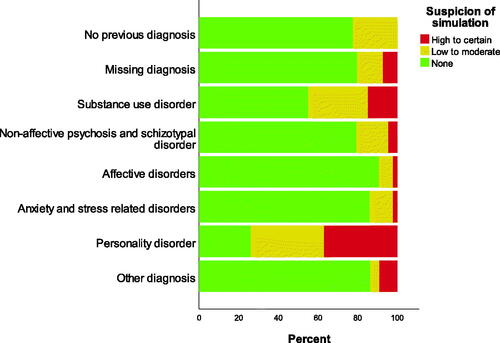
A total of 362 questionnaires were filled in. This amount to a response rate of 44% as there were 822 emergency unit contacts during the data collection period. Demographic information about patients and doctors are shown in and . shows the suspected symptoms and reasons for malingering. shows the proportion of suspected simulation for different diagnostic groups.
Table 1. Demographics of the patients.
Table 2. Responder’s position.
Table 3. Symptoms and reasons for suspected malingering and exaggeration.
25% (n = 90) of all patients in the psychiatric emergency wards were suspected of simulating to some degree (22%, n = 89 suspected of exaggerating), while 8% (n = 29) of patients were highly or definitely believed to be simulating (6%, n = 22 believed to be exaggerating).
Diagnostic groups differed on the frequency of suspected simulation (Chi2= 69, df = 14, p < 0.001) and exaggeration (Chi2= 57, df = 14, p < 0.001). Patients with diagnoses of substance use and personality disorder were suspected of simulation (p < 0.001) and exaggeration (p < 0.001) significantly more often than other patients.
We found no significant differences regarding suspicion of simulation or exaggeration for neither gender nor age of the patients, nor the degree of experience on part of the doctor.
displays the symptoms and suspected reasons for malingering. 9% (n = 33) of all patients were suspected of simulating suicidal ideation to some degree (8%, n = 29 for exaggeration), whereas 6% (n = 23) of patients were suspected of simulating psychotic symptoms (4%, n = 15 for exaggeration). Patients with diagnoses of personality disorder were especially prone to be suspected of simulating (p = 0.004) and exaggerating (p = 0.004) suicidal ideation. Thus, a total of 46% of patients with a diagnosis of personality disorder were suspected of simulating suicidal ideation to some degree.
Differences between diagnostic groups were also found regarding the suspected reasons for malingering. Patients with diagnoses of substance use disorder were significantly more likely to be suspected of simulation (p = 0.017) and exaggeration (p = 0.027) because of ‘Drug seeking behaviour’ than other perceived malingerers. Patients with diagnoses of personality disorder were significantly more likely to be suspected of simulation (p < 0.001) and exaggeration (p < 0.001) for the purpose of ‘attention seeking’ than other patients. Thus, 50% (n = 14) of all patients with a diagnosis of personality disorder were suspected of simulating because of ‘attention seeking’. We found no significant differences regarding suspected symptoms and reasons for malingering between patients from other diagnostic groups.
Discussion
This is the first European study to systematically examine doctors’ experience of malingering in the psychiatric emergency unit. A quarter of patients were suspected of simulating (8% highly suspected or definitely believed to be simulating). Importantly, our study only examined doctors’ suspicions of malingering, not whether the patients were in fact malingering.
The rate of suspected malingering was lower than in similar studies conducted in the US. Yates found that 42% of patients were suspected of malingering psychiatric symptoms [Citation2] while Rumshick found that 20% of patients were strongly or definitely suspected of malingering [Citation1]. It is worth noticing that these studies did not assess suspicion of simulation and exaggeration separately, possibly leading to higher rates of suspected malingering.
Patients with diagnoses of substance use and personality disorder were most frequently suspected of malingering. The most frequently perceived reasons for malingering for these patients were ‘Drug seeking behaviour’ and ‘Attention seeking’, respectively. Moreover, almost half of patients suffering from personality disorder were suspected to simulate suicidal ideation. Rumschik and colleagues theorised that patients suspected of malingering suicidal ideation were more likely to be admitted compared to suspected malingerers with other kinds of symptoms. Rumschik suggested that the potential lethal outcome in this difficult-to-assess symptom leads to admission as a precaution [Citation1]. It is conceivable that patients with multiple admissions throughout the years recognise that specific complaints e.g. suicidal ideation increases their chances of being hospitalised.
An alternative explanation may be related to prejudice on part of the medical staff against patients from certain diagnostic groups [Citation11,Citation18]. This may also explain the high rate of ‘attention seeking’ as a suspected reason for malingering in patients with a diagnosis of personality disorder. Several studies point to negative feelings/attitudes among mental health professionals towards patients with borderline personality disorder [Citation19], possibly affecting the perceived likelihood of malingering. Giles Newton-Howe et al. investigated the attitudes of mental health professionals towards patients with personality disorder and found a significantly greater amount of negativity towards these patients compared to patients from other diagnostic groups. Interestingly, they also found differences in attitude towards patients with covert vs overt diagnoses of personality disorder, allowing diagnostic labelling to become the independent variable. The authors recorded a significant increase in negative attitudes towards patients with overt diagnoses of personality disorders, pointing to prejudices independent of actual behaviour [Citation20].
Additionally, it is worth considering dynamic factors rooted in the relation between patient and doctor. Just as it is conceivable for doctors to react with weariness when triggered in certain ways by patients, patients can also modulate their responses according to the doctor’s attitude towards them and whether they feel understood by their clinician. As pointed out by Sandford et al., a patient may present symptoms differently according to the attitude of the clinician: A traumatized evaluee often presents as an uncooperative manipulator to a hypervigilant clinician, while the same patient presents as overwhelmed and depressed to a clinician who is open to hearing his or her pain [Citation21]
Obviously, the clinician does not have access to the patients’ first-person perspective and can only obtain an indication of the patients’ experiences by talking with the patients and observing their behaviour. However, the relation between experience and behaviour is often not univocal. For example seen in cases with incongruent affect, in which the patient’s emotional expression is not congruent with the thought content e.g. laughing when talking about very difficult subjects [Citation8]. Similarly, it is well known that patients with schizophrenia often abstain from acting upon psychotic experiences. The phenomenon of double bookkeeping makes it possible for the patient to live in two disjointed worlds, viz. our shared social world and the private, delusional world [Citation22].
McCarthy-Jones et al. provided a catalogue of typical properties of auditory hallucinations, for the purpose of guiding the assessment of malingering [Citation23]. The authors point out, that neither the acoustics of the voices, the patient’s attribution of to whom the voice belongs, the localisation, the clarity, the frequency, and length, nor the content or the patient’s ability to ignore the voices can consistently be relied on for assessing the genuineness of auditory hallucinations, as atypical presentations are numerous and common.
We speculate that structural factors influence the doctors’ suspicion of malingering. One example being the limited hospital capacity that makes it necessary for doctors in the emergency unit to sharply prioritise admissions. Additionally, there is a lack of psychopathological knowledge and training in the prototypes of mental disorders [Citation24–26]. Without such training, the clinician meets the patient without the necessary skills to organise and understand the information provided by the patient, and to assess his or her complaints. The doctor finds herself confronted with a myriad of unconnected data, often unable to distinguish essential from trivial information and exclude irrelevant diagnostic categories. When prototypes are not taught systematically, clinicians inevitably acquire their own private prototypes [Citation27], including the malingering patient.
Given the fact that malingering was described as a very rare condition and considered as such until recently, it is perhaps advisable that psychiatrists are very careful and conservative in making this assessment. Outside forensic psychiatry, it is, in most cases, difficult to disclose a clear motivation on part of the patient, and an assessment should not be based on simple symptomatology, and certainly not in the emergency unit. In most cases, malingering is not officially recorded, but nonetheless patients are treated differently as soon as the suspicion of malingering is articulated [Citation1].
Limitations
The major limitation of this study is the low response rate of 44%, possibly resulting in an overestimation of suspected malingering due to response bias. However, it is worth noting that the rate of suspected malingering in our study is comparable and even inferior to those reported in American studies with higher response rates [Citation1,Citation2].
Another limitation is the high rate of patients with no recorded diagnosis (19%, n = 69).
Ethical approval
All participation was anonymous, neither patients nor doctors could be identified. The study was conducted in concordance with the principles laid down by the Helsinki declaration.
Acknowledgements
The authors thank doctors Tobias Sørensen and Annette Rasmussen for their contribution to the study.
Disclosure statement
The authors have no relevant financial or non-financial interests to disclose.
Data availability statement
Not available for this study.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Rumschik SM, Appel JM. Malingering in the psychiatric emergency department: prevalence, predictors, and outcomes. Psychiatr Serv. 2019;70(2):115–122.
- Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv. 1996;47(9):998–1000.
- World Health Organization: WHO. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Weekly Epidemiol Record Relevé épidémiologique hebdomadaire. Geneva: WHO press. 1992;67:227–227.
- Sadock BJ, Va S. Kaplan and Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry. 11th. North American Edition. Philadelphia (PA): Lippincott Williams & Wilkins; 2015.
- ICD-11 for mortality and morbidity statistics. ICD-11 for mortality and morbidity statistics. cited 19 Feb 2022. Available: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1136473465.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington (DC): American Psychiatric Pub; 2013.
- Resnick PJ. Malingering of posttraumatic psychiatric disorders. J Psychiatric Pract. 1998;4:329–339.
- Jansson L, Nordgaard J. The psychiatric interview for differential diagnosis. Cham: Springer; 2016.
- Park L, Costello S, Li J, et al. Race, health, and socioeconomic disparities associated with malingering in psychiatric patients at an urban emergency department. Gen Hosp Psychiatry 2021;71:121–127.
- Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry 1988;153:44–49.
- van Boekel LC, Brouwers EPM, van Weeghel J, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013;131(1-2):23–35.
- Rissmiller DJ, Wayslow A, Madison H, et al. Prevalence of malingering in inpatient suicide ideators and attempters. Crisis 1998;19(2):62–66.
- Rissmiller DA, Steer RA, Friedman M, et al. Prevalence of malingering in suicidal psychiatric inpatients: a replication. Psychol Rep. 1999;84(3 Pt 1):726–730.
- Ritson B, Forrest A. The simulation of psychosis: a contemporary presentation. Br J Med Psychol. 1970;43(1):31–37.
- Humphreys M, Ogilvie A. Feigned psychosis revisited –a 20 year follow up of 10 patients. Psychiatr Bull. 1996;20(11):666–669.
- Hay GG. Feigned psychosis—a review of the simulation of mental illness. Br J Psychiatry 1983;143(1):8–10.
- Pope HG, Jr, Jonas JM, Jones B. Factitious psychosis: phenomenology, family history, and long-term outcome of nine patients. Am J Psychiatry 1982;139(11):1480–1483.
- Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):11.
- Sansone RA, Sansone LA. Responses of mental health clinicians to patients with borderline personality disorder. Innov Clin Neurosci. 2013;10(5-6):39–43.
- Newton-Howes G, Weaver T, Tyrer P. Attitudes of staff towards patients with personality disorder in community mental health teams. Aust N Z J Psychiatry 2008;42(7):572–577.
- Drob SL, Meehan KB, Waxman SE. Clinical and conceptual problems in the attribution of malingering in forensic evaluations. J Am Acad Psychiatry Law 2009;37(1):98–106.
- Parnas J, Urfer-Parnas A, Stephensen H. Double bookkeeping and schizophrenia spectrum: divided unified phenomenal consciousness. Eur Arch Psychiatry Clin Neurosci. 2021;271(8):1513–1523.
- McCarthy-Jones S, Resnick PJ. Listening to voices: the use of phenomenology to differentiate malingered from genuine auditory verbal hallucinations. Int J Law Psychiatry 2014;37(2):183–189.
- Nordgaard J, Sass LA, Parnas J. The psychiatric interview: validity, structure, and subjectivity. Eur Arch Psychiatry Clin Neurosci. 2013;263(4):353–364.
- Schwartz MA, Wiggins OP. Typifications. The first step for clinical diagnosis in psychiatry. J Nerv Ment Dis. 1987;175(2):65–77.
- Schultze-Lutter F, Schmidt SJ, Theodoridou A. Psychopathology—a precision tool in need of re-sharpening. Front Psychiatry 2018;9(446):446.
- Kendler KS, Parnas J. Philosophical issues in psychiatry II: Nosology. Oxford: OUP; 2012.