Abstract
Background
Violence in psychosis has been linked to antisocial behavior and psychopathy traits. Psychopathy comprises aspects of interpersonal, affective, lifestyle, and antisocial traits which may be differently involved in violent offending by persons with psychotic disorders. We explored psychopathy subdomains among violent offenders with and without a psychotic disorder.
Methods
46 males, with a history of severe violence, with (n = 26; age 35.85 ± 10.34 years) or without (n = 20; age 39.10 ± 11.63 years) a diagnosis of a psychotic disorder, were assessed with the Psychopathy Checklist-Revised (PCL-R). PCL-R was split into subdomains following the four-facet model. Group differences in total and subdomain scores were analyzed with a general linear model with covariates.
Results
Total PCL-R scores did not differ between the groups (p = 0.61, Cohen’s d = 0.17). The violent offenders without psychotic disorders had higher facet 2 scores than the patient group with psychotic disorders (p = 0.029, Cohen’s d = 0.77). Facet 1, 3, or 4 scores did not differ between the groups. Controlling for age did not alter the results.
Conclusion
Patients with a psychotic disorder and a history of severe violence have lower affective psychopathy scores than violent offenders without psychotic disorders. This observation may point toward distinct underlying mechanisms for violence and may provide a target for focused treatment and prevention.
Introduction
The large majority of individuals with a mental disorder will never be violent [Citation1] and are more likely to become the victim of violence themselves [Citation2,Citation3]. Nevertheless, epidemiological studies show that individuals with psychotic disorders (disorders that can manifest in psychosis) are at a higher risk of violent behavior than the general population [Citation4,Citation5]. This applies especially to schizophrenia [Citation6–11], which is the most common of these disorders [Citation12]. Males with schizophrenia are up to seven times more likely to be convicted for a violent offense than non-psychiatric controls [Citation9]. Substance use disorders further increase the risk of violence in schizophrenia [Citation6,Citation13]. Violence among adults with psychotic disorders may be divided into at least three etiological subtypes related directly to (i) positive psychotic symptoms, (ii) impulsive violence, and (iii) comorbidity with personality disorders, particularly antisocial personality disorder (ASPD), and psychopathy [Citation14]. Some studies have shown that the violence committed by patients with schizophrenia and psychopathy is primarily caused by personality traits and not psychotic symptoms [Citation6,Citation15]. The prevalence of comorbidity of schizophrenia and psychopathy is unfortunately not well characterized in the general forensic population [Citation16], a variation from below 5% [Citation17] up to 20% is reported, numbers are highest among seriously violent patients with a mental illness [Citation15,Citation18]. This comorbidity has implications for the treatment and understanding of violence in forensic psychiatry wards.
Individuals exhibiting psychopathic traits require extensive resources in the criminal justice system. They commit a large proportion of the most severe violence [Citation19], represent 15–25% of prison populations and approximately 1% of the general population [Citation19], and often recidivate to crime despite rehabilitative efforts [Citation20]. Comorbid psychopathy is a risk factor for violent recidivism in schizophrenia, with a four-fold increase in risk compared to schizophrenia patients without psychopathy [Citation15]. Interestingly, these estimates correspond to incarcerated populations without mental disorders, where individuals with several psychopathic traits have a four to six-fold higher risk for reoffending than non-psychopathic individuals [Citation21]. Accordingly, patients with both schizophrenia and psychopathic traits present a challenging group in forensic psychiatry [Citation8]. They are more likely to be non-compliant with treatment programs and have poorer institutional outcomes [Citation22]. Patients with schizophrenia and high psychopathy scores show similar deficits in emotional information processing as psychopathic persons without psychotic disorders [Citation23]. They show higher levels of hostile and grandiose symptomatology [Citation22], a less compliant interpersonal style, and higher trait impulsivity and aggression scores [Citation22] than non-psychopathic schizophrenia patients. Hence, psychopathic patients with psychotic disorders constitute a specific sub-group that is important to identify to ensure optimal treatment and implement violence precaution measures.
Psychopathy is characterized by personality traits such as a fearless and dominant temperament with an impulsive and antisocial orientation [Citation19]. Robert Hare, the author of PCL-R - which is regarded as the ‘state of the art’-tool for measurement of psychopathy [Citation15,Citation24], considers psychopathy to be a construct [Citation19], but it can also be considered a personality deviance [Citation19], a condition [Citation25] or a personality type [Citation26]. While psychopathy is not recognized as a diagnosis within the existing nosological systems, it has been included as a specifier of ASPD in DSM (APA, 2000) and in dissocial personality disorder in ICD-10 (WHO, 2000).
Following Hervey Cleckley’s definition of psychopathy, the construct comprises different traits [Citation24] including affective deficits (e.g. shallow affect, lack of remorse, and shame), callousness, lack of empathy, and dysfunctional personality traits related to social functioning (e.g. egocentricity, manipulativeness, unwillingness to accept responsibility, insincerity, and lying) [Citation1,Citation8]. Robert Hare argues that there is strong empirical support for an overall superordinate factor of psychopathy, two factors, and four facets [Citation19]. The two main factors are affective/interpersonal traits and antisocial deviance. These factors are further split into four facets: affective, interpersonal, lifestyle, and antisocial [Citation19,Citation27]. Breaking the total score into factors and facets may increase our understanding of the inherent nuances of psychopathy, and inspection of the factors and facet scores facilitates interpretation of a given PCL-R assessment [Citation19].
Psychopathy has been associated with childhood conduct disorders [Citation28], especially in combination with callous-unemotional traits (CU- traits) [Citation22,Citation29–32], which are risk factors for violence in schizophrenia [Citation32]. CU traits are early emerging personality features characterized by deficits in empathy, lack of concern for others, and remorse [Citation30,Citation33]. Behavioral manifestations of CU have been suggested to emerge from the combination of low interpersonal emotional sensitivity and fearlessness, temperaments that appear to be inherited and subsequently interact with parenting [Citation30]. Harsh and strict parenting with a lack of warmth exacerbates the risk of developing CU traits and later psychopathy in genetically vulnerable children [Citation29,Citation30]. The CU traits essentially represent facet 2 in PCL-R [Citation34]. Males diagnosed with schizophrenia are more likely to have a history of conduct disorder [Citation6]. The strength of the association between childhood conduct disorder and aggressive behavior in adulthood appears similar among individuals who do and do not develop schizophrenia [Citation32].
Few studies have examined psychopathy in comparable samples of violent individuals with and without psychotic disorders. A Finnish study of psychopathic traits in homicide offenders with and without schizophrenia showed psychopathic features in both groups [Citation8]; however, offenders with schizophrenia had significantly lower total scores and scored lower on facets 3 and 4 [Citation8]. In contrast, we recently showed that patients with psychotic disorders and a history of violence (‘PSY-V’) from security units had similar PCL-R total scores as incarcerated violent individuals without psychotic disorders (non-psychotic violent individuals-‘NPV’) serving an indeterminate prison sentence for serious violence [Citation35].
This current study builds on our earlier results and explores whether the patients with psychotic disorders and the incarcerated violent offenders without psychotic disorders show different psychopathy construct facet profiles. We hypothesized that PSY-V would score lower than NPV on at least one of the following facets: (i) facet 1 (superficial charm, grandiosity, pathological lying, manipulativeness) due to their weaker social cognitive abilities [Citation36], (ii) facet 2 (lack of remorse or guilt, shallow affect, callous/lack of empathy, and failure to accept responsibility for own actions) – the core symptoms of psychopathy – due to expected less ‘true psychopathic’ traits than the incarcerated group, or (iii) facet 4 (poor behavioral controls, early behavioral problems, juvenile delinquency, revocation of conditional release, and criminal versatility) following earlier findings [Citation8] and the presumed lower ability to plan and carry out criminal acts [Citation37]. We hypothesized that they would score the same on facet 3 (need for stimulation/proneness to boredom, parasitic lifestyle, lack of realistic long-term goals, impulsivity, and irresponsibility).
Methods
Subject sample
The subject sample consisted of 46 males with a history of severe violence (murder, attempted murder, severe violence towards other persons, or sexual assaults) according to the MacArthur criteria) [Citation38]: 26 patients with a psychotic disorder and a history of violence (PSY-V; schizophrenia spectrum (n = 24), and bipolar disorder with psychosis (n = 2)), and 20 violent offenders without psychotic disorders (NPV). The sample partially overlaps (PSY-V = 17, NPV = 17) with the subject sample from previous studies [Citation35,Citation39]. The PSY-V group was recruited from high-security psychiatric wards at Oslo University Hospital and Østfold Hospital, Norway.
The NPV group was recruited from a male prison in the Oslo region, Norway. It consisted of incarcerated persons serving a preventive detention sentence. They did not have a psychotic disorder at the time of the violent offense nor study inclusion. Briefly, preventive detention is a sanction imposed in cases where a time-limited prison sentence is deemed insufficient to protect society from the risk posed by the offender, which may involve life-long imprisonment. As of December 2021, 154 persons were serving a preventive detention sentence, which is the strictest sentence, in Norway.
All participants were assessed by trained clinicians (psychiatrists or psychologists) and included as part of the ongoing multi-center ‘Violence in psychosis’ (sTOP) study in Oslo, Norway, between 2015 and 2019. Inclusion criteria for both groups were age between 18 and 65 years, sufficient skills in Norwegian to understand the study protocol and procedures, IQ scores above 65, and the ability to give informed consent to study participation.
The Norwegian Regional Committee for Medical Research Ethics, Norwegian Data Protection Authority, and relevant correctional agencies approved the study. Written informed consent was obtained from all participants after a complete description of the study and after the project physicians or the treating psychiatrist/psychologist had evaluated the subject’s capacity to give informed consent to study participation. The study was conducted according to the Helsinki declaration.
Clinical assessment
Trained physicians, psychiatrists, and psychologists administered assessments of each study participant through clinical examination, (for details, see [Citation35]). Diagnoses were based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and confirmed with the Structured Clinical Interview for DSM-IV Axis 1 disorders (SCID-1) [Citation40], with the addition of supplementary information drawn from medical records and forensic reports. The presence of anti-social personality disorder was assessed with SCID II. Psychosocial functioning was evaluated with the Global Assessment of functioning scale (GAF) scale. Alcohol and illicit substance use were assessed with The Alcohol Use Identification Test (AUDIT) and The Drug Use Disorders Identification test (DUDIT), respectively. These are self-report questionnaires that cover use over the last 12 months.
Current psychotic symptoms were rated using the Positive and Negative Syndrome Scale (PANSS) [Citation41]. Antipsychotic medication use was assessed and Defined Daily Dosages (DDD) of current antipsychotic medication use were calculated according to the guidelines from World Health Organization (WHO; https://www.whocc/atc_ddd_index/).
A history of violent behavior was assessed from court documents, hospital records, and the self-report instrument Life history of aggression [Citation42]. All participants’ current IQ was measured with the Norwegian version of the Wechsler Abbreviated Scale of Intelligence (WASI) by specially trained psychologists. The number of completed years of formal schooling was used to estimate educational attainment.
Psychopathy traits
Psychopathy was evaluated with PCL-R, a 20-item scale for assessing psychopathy in research, clinical, and forensic settings. It uses a semi-structured interview, file, and collateral information to measure personality traits and behaviors related to a widely understood conception of psychopathy [Citation19]. The items are rated on a three-point Likert scale (0 = not present, 1 = present to some degree, 2 = present), with a maximum score of 40 points. A PCL-R total score of 30 has been used as a cutoff in North America, while 25 is typically used in Europe [Citation19]. The current study used the four-facet model described by Robert Hare in the PCL-R 2nd edition manual [Citation19]: Facet 1 – Interpersonal (PCL items 1, 2, 4, and 5); Facet 2 – Affective (items 6, 7, 8, and 16); Facet 3 – Lifestyle (items 3, 9, and 13–15); and Facet 4 Antisocial (items 10, 12, and 18–20) as shown in . Two of the 20 items are left out because they do not apply specifically to any of the four facets. That is items 11 (promiscuous sexual behaviour) and 17 (many short-term marital relationships).
Figure 1. Table from PCL-R. Factor 1 includes the Interpersonal/Affective facets 1 and 2, while Factor 2 includes the Social Deviance (Lifestyle/Antisocial) facets 3 and 4.

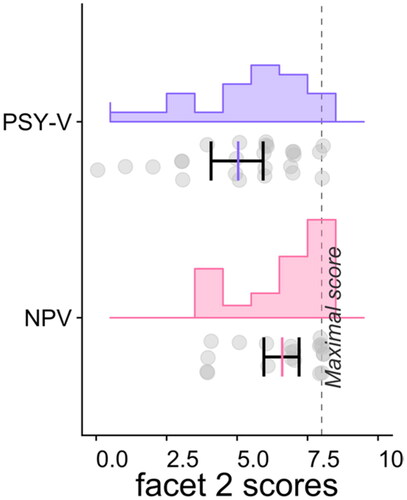
Figure 2. The distribution of facet 2 scores in individuals with a psychotic disorder and a history of violence (PSY-V) and non-psychotic violent individuals (NPV). Histogram, scatter plot, and mean/confidence interval.
The PCL-R assessment was performed by trained and certified medical doctors, psychiatrists, or psychologists calibrated through the official PCL-R training. Two raters (CB, UKH) scored both offenders with psychotic disorders and non-psychotic disorder offenders to ensure the same practice in the prisons and hospital wards.
Statistical analyses
Group differences between PSY-V and NPV in clinical and socio-demographic and clinical characteristics were analyzed with t-tests or chi-square tests in SPSS (version 27). Differences between the groups on four facets and total scores were tested with a general linear model, covarying for age, alcohol, and illicit substance use, and performed with non-parametric permutation-based testing implemented in the PALM tool [Citation43]. The false discovery rate was used to correct for multiple testing (FDR).
Results
Clinical and socio-demographic characteristics
Clinical and socio-demographic characteristics are listed in . The groups differed on all PANSS subscales. PSY-V scored higher than NPV on PANSS total score and general, positive, and negative symptoms. The two groups did not differ significantly on age at inclusion, educational attainment, drug and alcohol use, or IQ.
Table 1. Demographic and clinical characteristics.
Psychopathy traits
The total PCL-R scores did not differ significantly between the groups (p = 0.61, Cohen’s d = 0.17), with PSY-V and NPV having a mean score of 19.3 (SD 9.1) and 20.7 (SD 7.7), respectively. There were 8 of 26 in the PSY-V group and 6 of 20 in the NPV group who scored above the cutoff 25 on the PCL-R assessment (approximately 30%) in both groups (χ2=0.0032, p = 0.955), which was not significant at p < 0.05. 11 of 24 (46%) (2 were missing) in the PSY-V group and 14 of 20 (70%) in the NPV group met the DSM-IV criteria for antisocial personality disorder (ASPD) (Chi-square: χ2=2.597, p = 0.107), which was not significant at p < 0.05.
The NPV offenders scored higher on facet 2 than the PSY-V group (i.e. on the affective traits comprising lack of remorse or guilt, shallow affect, callous/lack of empathy, and failure to accept responsibility for own actions) (p = 0.029, Cohen’s d = 0.76), as shown in . Facet 1, 3, or 4 scores did not differ between the groups (p = 0.98, Cohen’s d= −0.25, p = 1, Cohen’s d = −0.40, p = 0.8, Cohen’s d = 0.03, respectively).
The group difference in facet 2 scores remained significant after adjusting for age (p = 0.04, Cohen’s d = 0.90) but showed only trend level association when we controlled for age, alcohol, and illicit substance use within the same model (p = 0.067, Cohen’s d = 1.12). These results are listed in .
Table 2. Differences in PCL-R total- and facet scores between individuals with a psychotic disorder and a history of violence (PSY-V) and non-psychotic violent offenders (NPV).
Discussion
In this study, we explored psychopathy traits between patients with psychotic disorders and a history of violence (PSY-V), and violent offenders without psychotic disorders (NPV) serving an indeterminate prison sentence. The main results were that PSY-V scored significantly lower for the affective subdomain (facet 2) despite both groups showing similar total psychopathy scores. Scores on the other facets [Citation1,Citation3,Citation4] did not differ between the groups. In both groups, we found that the mean total PCL-R score was approximately 20, in line with the results from earlier research on forensic populations [Citation8,Citation19]. A score of 20 has been considered a cutoff for ‘medium psychopathy’ [Citation44]. In both groups, approximately 30% of the participants scored above 25 on the PCL-R, which is the standard cutoff value for psychopathy applied in Europe [Citation19]. 11 of 24 (46%) in the PSY-V group and 14 of 20 (70%) in the NPV group met the DSM-IV criteria for antisocial personality disorder (ASPD). This is in line with the current diagnostic criteria according to which it is easier to qualify for ASPD than psychopathy [Citation19] and consistent with previous studies showing that up to 90% of individuals with psychopathy would meet the diagnostic criteria for ASPD, while up to 40% of the individuals diagnosed with ASPD would satisfy the criteria for psychopathy [Citation19,Citation45,Citation46].
The NPV group had a higher load of facet 2 traits, including lack of remorse or guilt, shallow affect, callousness/lack of empathy, and failure to accept responsibility for own actions. These traits are those components of the psychopathy construct that comprise affectivity and emotional sensitivity [Citation19]. They are usually stable throughout life and less influenced by culture than the other PCL-R facets [Citation47]. This finding aligns with our hypothesis of higher facet 2 scores in the NPV group since facet 2 comprises the core psychopathy symptoms [Citation48]. However, the PSY-V group also scored relatively high on this facet. This observation is consistent with previous studies showing difficulties in identifying emotions, feeling connected to others, considering others’ perspectives, and reacting emotionally to others among schizophrenia patients [Citation36,Citation49], as well as reduced recognition of facial expressions [Citation50,Citation51] and mentalizing abilities [Citation52].
Contrary to our hypotheses, PSY-V and NPV did not differ in facet 1 and facet 4. Regarding facet 1, we expected that this facet, the interpersonal facet (glibness/superficial charm, grandiose sense of self-worth, pathological lying, and conning/manipulativeness), would be lower in PSY-V due to these patients’ expected reduced non-social [Citation37] and social cognitive [Citation36,Citation49] abilities, including problems with processing complex information, lower cognitive flexibility, and difficulties in planning compared to healthy control subjects [Citation37]. However, they did not differ from the NPV group. A prior study [Citation8] showed lower facet 4 scores, the antisocial facet (poor behavioral controls, early behavioral problems, juvenile delinquency, revocation of conditional release, and criminal versatility), in schizophrenia patients than in offenders without psychotic disorders. We did not replicate this finding, our groups showed similar levels of antisocial traits.
Factor 1 (facet 1 and 2) traits often manifest as treatment-interfering behaviors. Callous and unemotional traits cause difficulties in establishing an effective therapeutic alliance [Citation24]. Previous research has demonstrated that facet 2 is associated with less therapeutic change and higher dropout rates in forensic treatment [Citation34,Citation53] as affective and empathy deficits are hypothesized to undermine the development of insight and the willingness to truly engage in treatment [Citation24,Citation53]. The PSY-V scored lower on facet 2, which suggests an advantage relative to the NPV regarding the possible treatment of psychopathic traits. However, the study of Laajasalo et al. showed that offenders with schizophrenia and high levels of psychopathic traits showed several similarities to psychopathic offenders without psychotic illness [Citation8]. Both groups presented early life problems such as school difficulties, parental psychiatric and criminal history, and contact with mental health services during childhood and adolescence, and they performed similar violent acts [Citation8]. These observations have implications for early intervention and management [Citation8], and importantly, treating only the psychosis may not reduce the risk for violence in patients with a high psychopathic profile [Citation18].
Psychopathy (without other mental illnesses) has widely been considered treatment-resistant, but the literature on treatment outcomes is scarce and the current results on treatment effectiveness are inconsistent [Citation14]. Research generally shows that psychopathic offenders are less likely to benefit from, and more likely to drop out of, treatment programs [Citation54,Citation55] and that the interpersonal and emotional features of psychopathy may be associated with poor treatment response [Citation34]. However, some studies have reported reductions in sexual or violent recidivism among psychopathic offenders who displayed positive treatment behavior [Citation56] or who were evaluated as having made risk-related treatment gains after cognitive-behavioral oriented therapy [Citation57]. Lower rates of violence were also reported in a sample of psychopathic civil psychiatric patients who received larger doses of outpatient mental health services [Citation58] Interestingly, prosocial behavior in individuals with psychopathy was seen after computerized training that targeted cognitive-affective deficits [Citation59], and after biofeedback training where the offenders learned to regulate their brain activity to improve behavioral control [Citation45,Citation60].
Not surprisingly, patients with both psychotic disorders and psychopathy also show reduced compliance with treatment programs [Citation8,Citation61,Citation62], but there have been some optimistic studies linked to risk-reduction-focused treatment [Citation34,Citation53] in patients with schizophrenia, a history of violent behavior, and comorbid psychopathy [Citation53]. This therapy focuses on treating factor 2 (facets 3 and 4), as the antisocial facet (facet 4) is the strongest predictor of future recidivism in the PCL-R [Citation9,Citation34,Citation53,Citation63]. Further, this is in line with epidemiological studies showing that a criminal history is the strongest predictor of all types of aggression, including severe violence [Citation53]. In the present study, the PSY-V group scored similarly to the NPV group on facets 3 and 4, pointing toward the same risk for violent recidivism in both groups [Citation9,Citation34,Citation63]. Studies have shown that the association between recidivism and factor 2 (facet 3 and 4) remain significant after controlling for substance abuse, which is another important predictor of violence in schizophrenia [Citation4,Citation63]. However, our two groups did not differ significantly on substance abuse. The participants had mostly been drug-free for a long period because of incarceration/admission to security wards with restricted access to drugs and alcohol, but previous substance and alcohol misuse were present in both groups.
Accordingly, the shown comorbidity has many implications for treatment. If the patient has comorbid antisocial or psychopathic traits, the risk of recidivism is higher [Citation15] the probability of drug abuse is higher [Citation64], and the probability of establishing an alliance with the patient as well as the probability of treatment compliance is lower [Citation8]. It follows that the treatment program should even more closely monitor psychosis patients with comorbid ASPD or psychopathy. Antipsychotic medication is used for treating psychosis, but also for its anti-aggressive effect [Citation65,Citation66]. Ensuring adherence to antipsychotic medication is important, either by using depot injections or by ensuring oral intake by regular blood tests [Citation67], Clozapine is the preferred antipsychotic for highly aggressive patients [Citation68–70]. The absence of illegal substances must be secured through frequent drug screenings, and general security evaluations should be undertaken regularly [Citation71]. Impulsivity and anxiety should be properly treated when prominent (e.g. antiepileptics, lithium, antipsychotics) [Citation72]. Anger control training has also shown an effect on reducing aggression [Citation15]. Leaves during hospitalization should be restricted when necessary, and extended surveillance in the community post-discharge should be implemented [Citation15]. All this while bearing in mind that these patients have good abilities to lie and manipulate [Citation8]. When paranoia, bizarre thinking, and delusions manifest themselves in a person with psychopathic traits such as novelty-seeking, lack of remorse, and callousness, the violence risk increases considerably [Citation8], but on the contrary, when symptoms of schizophrenia are improved this can sometimes facilitate psychopathic traits and behavior [Citation73]. Reinforcing prosocial behaviors is important in all interactions between patients and staff [Citation71].
Treatment must be individualized as there is heterogeneity among patients with schizophrenia and psychopathy [Citation73]. Psychopathic traits can influence the function of schizophrenia patients in complex ways, as shown by Abu-Akel et al. [Citation74]. They found that increased PCL-R scores in a schizophrenia patient sample were associated with a decline in metacognitive abilities, but only until the cut-off was reached. Those with psychopathy scores above the cut-off had their meta-cognitive abilities mostly intact, which could explain goal-directed aggression among some individuals with schizophrenia [Citation74]. This is of importance when assessing violence risk. Sedgwick et al. found that violent offenders with comorbid psychosis and dissocial personality disorder showed larger impairments in sensorimotor gating (lower PPI) than in individuals with psychosis alone [Citation75]. The impairments were hypothesized to make psychosis patients with comorbid dissocial personality disorder vulnerable to overstimulation at times of high stress and thereby less likely to restrict themselves, which can result in impulsive and antisocial behavior [Citation75].
Finally, since psychopathy is considered one of the greatest risks regarding future criminal recidivism for violence in schizophrenia [Citation15], there are good reasons for implementing PCL-R, (or at least its short version, the PCL-SV [Citation76]) in clinical forensic practice on a general basis [Citation73].
The present study has some limitations. The subject sample was limited and included males only, reflecting the populations in the security hospital wards and prisons as well as the higher prevalence of violence among males [Citation77]. As such, the results cannot be generalized to female violent offenders. We had 24 patients with schizophrenia spectrum disorders and 2 patients with bipolar disorder with psychosis. This may be a confounder since psychopathic traits can behave differently in these conditions. We used a cross-sectional design that captures a specific moment in time. Some of the participants’ psychopathy traits may change over time, although reports indicate that the psychopathy traits are relatively stable across lifetime [Citation19,Citation78].
We chose to use PCL-R to measure psychopathy. However, other instruments such as the Comprehensive Assessment of Psychopathic Personality-Institutional Rating Scale (CAPP-IRS) [Citation63], The Triarchic Psychopathy Measure (TriPM) [Citation79], or Cooke and Michies 3-factor model for the PCL-R [Citation80] could provide additional information. Attributing psychopathy symptoms to schizophrenia might underestimate actual psychopathy traits. Conversely, calculating PCL-R scores independent of the underlying etiology may overestimate psychopathy traits (false positives) [Citation63]. The PCL-R has no exclusion criteria [Citation19] and it has been widely used to study psychopathy in (forensic) schizophrenia patients [Citation8,Citation9,Citation15,Citation73,Citation81] but the validity of the PCL-R assessment of patients with psychotic disorders has been debated [Citation63]. The use of PCL-R in violent patients with schizophrenia may be confounded by the presence of concurrent psychotic symptoms [Citation82]. Negative symptoms of schizophrenia (e.g. flat affect or emotional withdrawal) can be confused with the PCL-R item ‘Shallow affect’ [Citation15,Citation47]. Positive schizophrenia symptoms such as inflated self-esteem in megalomania or psychomotor agitation can lead to higher scores on the PCL-R items ‘Grandiose self-worth’ or ‘Impulsivity’ [Citation63]. The PCL-R manual does not provide guidelines for handling this potential confounding [Citation63], but there is a study examining this which concludes that the negative state of psychosis and ‘the deficient affective experience’ in psychopathy construct are most likely different concepts [Citation47] In the current study, the symptom overlap is expected to be relatively small since the majority of the patients were in a stable phase of their illness during study procedures, i.e. they were on antipsychotic medication and mostly showed low to moderate psychotic symptoms (see , PANSS scores) during the examinations and interviews. Moreover, the PCL-R covers lifetime behavior and traits, i.e. the score also depends on their history from before the onset of psychosis. Personality traits included in the psychopathy construct have been demonstrated to emerge before developing psychotic symptoms [Citation6]. There is an overlap between personality pathology and all types of mental disorders [Citation83], and new methods to define and measure this comorbidity are needed. Maybe a shift toward a dimensional framework of personality pathology will lead to better methods in the future [Citation83].
Strengths of the study include a thorough and standardized clinical characterization of all participants, with validated scoring instruments. All PCL-R-raters underwent the same structured training, and raters discussed scores to achieve consensus. Two raters (CB, UKH) scored both patients with psychotic disorders and violent offenders without psychotic disorders to ensure the same practice in the prisons and hospital wards. A large part of the studies on psychopathy using PCL-R comes from the USA [Citation19]. This study gives a contribution from Scandinavia, where both the legal system and the health care system are different. Despite the relative small subject sample, the study includes approximately 20% of the individuals serving a preventive detention sentence in Norway at the time of data collection.
Conclusion
In this study, we found that patients with psychotic disorders (mainly schizophrenia spectrum disorders) and a history of severe violence and incarcerated violent offenders without psychotic disorders differ in the facets within the psychopathy construct. The patient group scores lower on the affective dimensions of psychopathy, which may be beneficial for establishing a therapeutic alliance. Our findings support the relevance of the clinical construct of psychopathy for both violent offenders with and without a psychotic disorder as well as the importance of undertaking psychopathy assessments among these violence-prone individuals as they are essential for treatment and for predicting violence risk. Future studies should address the potential of individualized treatment of subdomains of psychopathy. However, it is important to emphasize that the most severe violence is perpetrated by a subgroup of patients with schizophrenia and comorbid psychopathy traits, and this may contribute to destigmatizing schizophrenia.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guides on the care and use of laboratory animals.
Acknowledgement
We performed this work on the Services for sensitive data (TSD), University of Oslo, Norway, with resources provided by UNINETT Sigma2 - the National Infrastructure for High-Performance Computing and Data Storage in Norway, and the South-Eastern Norway Regional Health Authority 2022080
Disclosure statement
OAA has received a speaker’s honorarium from Lundbeck and is a consultant to HealthLytix. All the other authors report no conflicts of interest.
Data availability statement
Due to ethical and data security issues related to the sensitive nature of the clinical data we are not allowed to share the data without specific IRB approval and data use agreements with the relevant institution. More information can be obtained through the corresponding author: Christina Bell (email address: [email protected]).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Christina Bell
Christina Bell, psychiatrist, consultant at the psychiatric security unit at Gaustad, Oslo University Hospital, and PhD candidate at the University of Oslo since 2018. Research fields of interest include psychosis, psychopathy, violence, social cognition, and neuroimaging.
Jaroslav Rokicki
Jaroslav Rokicki, PhD, Researcher at the Centre of Research and Education in Forensic Psychiatry, Oslo University Hospital from 2020, with an interest in the application of machine learning methods for brain age prediction and to disentangle the role of violence in mental illnesses.
Gabriela Hjell
Gabriela Hjell, MD and resident in psychiatry. PhD candidate at the University of Oslo from 2018, focusing on biological correlates of agitation. Research fields of interest include severe mental disorders, cardiovascular comorbidity, and interplay between the immune system and mental health.
Thomas Fischer-Vieler
Thomas Fisher-Vieler, MD, PhD candidate at NORMENT/University of Oslo. Consultant psychiatrist in a flexible assertive community treatment (FACT) team at a public out-patient clinic in Bærum, Norway. Main interests are psychotic disorders, insight and self-disorders.
Ingrid Melle
Ingrid Melle, Psychiatrist, professor at the University of Oslo, senior consultant at Oslo University Hospital, main fields of interest: Etiology of Schizophrenia and bipolar disorder, treatment, and suicidality.
Ole A. Andreassen
Ole Andreassen, Psychiatrist, professor, and leader at the centre of excellence, Norment. His main fields of interest are mental health, somatic comorbidity, and genetics. Senior consultant at Nydalen district psychiatric centre, Oslo University Hospital.
Petter Andreas Ringen
Petter Andreas Ringen, Head of Division, Division of Mental Health and Addiction, Oslo University Hospital. Professor of Psychiatry, University of Oslo. Research interests: risk factors and understanding of psychosis and somatic comorbidity in severe mental illness.
Kirsten Rasmussen
Kirsten Rasmussen is professor emerita in forensic psychology at the Norwegian University of Science and Technology and working at St Olav’s hospital Centre for Research and Education in Forensic Psychiatry. Her research has focused mainly on mental health and violence, psychopathy, adult ADHD and violence risk assessment.
Hilde Dahl
Hilde Dahl, PhD, a senior research scientist at St. Olavs Hospital, Centre for research and education in forensic psychiatry, Trondheim, Norway, and Norwegian University of Science and Technology (NTNU), Department of Psychology and Department of Mental Health.
Christine Friestad
Christine Friestad, Psychologist, PhD, researcher at Centre of Research and Education in Forensic Psychiatry, Oslo University Hospital, Norway, and at University College of Norwegian Correctional Service, Oslo, Norway.
Unn K. Haukvik
Unn K. Haukvik, MD, PhD, associate professor of psychiatry, Institute for Clinical Medicine, University of Oslo. Head of the forensic psychiatry research group at the Centre of excellence Norwegian center for mental health research NORMENT. Senior researcher at the Centre for research and education in forensic psychiatry, Oslo University Hospital.
References
- Walsh E, Fahy T. Violence in society. BMJ. 2002;325(7363):507–508.
- Walsh E, Moran P, Scott C, et al. Prevalence of violent victimisation in severe mental illness. Br J Psychiatry. 2003;183:233–238.
- Latalova K, Kamaradova D, Prasko J. Violent victimization of adult patients with severe mental illness: a systematic review. Neuropsychiatr Dis Treat. 2014;10:1925–1939.
- Fazel S, Gulati G, Linsell L, et al. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8):e1000120.
- Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiatry. 2006;163(8):1397–1403.
- Volavka J. Comorbid personality disorders and violent behavior in psychotic patients. Psychiatr Q. 2014;85(1):65–78.
- Fazel S, Wolf A, Palm C, et al. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry. 2014;1(1):44–54.
- Laajasalo T, Salenius S, Lindberg N, et al. Psychopathic traits in Finnish homicide offenders with schizophrenia. Int J Law Psychiatry. 2011;34(5):324–330.
- McGregor K, Castle D, Dolan M. Schizophrenia spectrum disorders, substance misuse, and the four-facet model of psychopathy: the relationship to violence. Schizophr Res. 2012;136(1–3):116–121.
- Whiting D, Gulati G, Geddes JR, et al. Association of schizophrenia spectrum disorders and violence perpetration in adults and adolescents from 15 countries: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79(2):120–132.
- Maier W, Hauth I, Berger M, et al. [Interpersonal violence in the context of affective and psychotic disorders]. Nervenarzt. 2016;87(1):53–68.
- Holder SD, Wayhs A. Schizophrenia. Am Fam Physician. 2014;90(11):775–782.
- Rund BR. A review of factors associated with severe violence in schizophrenia. Nord J Psychiatry. 2018;72(8):561–571.
- Volavka J, Citrome L. Heterogeneity of violence in schizophrenia and implications for long-term treatment. Int J Clin Pract. 2008;62(8):1237–1245.
- Tengstrom A, Grann M, Langstrom N, et al. Psychopathy (PCL-R) as a predictor of violent recidivism among criminal offenders with schizophrenia. Law Hum Behav. 2000;24(1):45–58.
- Newton-Howes G, Tyrer P, North B, et al. The prevalence of personality disorder in schizophrenia and psychotic disorders: systematic review of rates and explanatory modelling. Psychol Med. 2008;38(8):1075–1082.
- Rice ME, Harris GT. Psychopathy, schizophrenia, alcohol abuse, and violent recidivism. Int J Law Psychiatry. 1995;18(3):333–342.
- Abushua’leh K, Abu-Akel A. Association of psychopathic traits and symptomatology with violence in patients with schizophrenia. Psychiatry Res. 2006;143(2–3):205–211.
- Hare RD. Hare PCL-R. 2nd ed. Toronto (ON): Canada Multi-Health Systems Inc.; 2003.
- Moraga G, Garcia FR, Billstedt D, et al. Facets of psychopathy, intelligence, and aggressive antisocial behaviors in young violent offenders. Front Psychol. 2019;10:984.
- Hemphill JF, Hare RD, Wong S. Psychopathy and recidivism: a reviewl. Legal Crim Psychol. 1998;3(1):139–170.
- Fullam R, Dolan M. The criminal and personality profile of patients with schizophrenia and comorbid psychopathic traits. Personal Individual Differ. 2006;40(8):1591–1602.
- Fullam R, Dolan M. Emotional information processing in violent patients with schizophrenia: association with psychopathy and symptomatology. Psychiatry Res. 2006;141(1):29–37.
- Yang M, Wong SC, Coid J. The efficacy of violence prediction: a meta-analytic comparison of nine risk assessment tools. Psychol Bull. 2010;136(5):740–767.
- Viding E, McCrory E, Seara-Cardoso A. Psychopathy. Curr Biol. 2014;24(18):R871–R874.
- Pujol J, Harrison BJ, Contreras-Rodriguez O, et al. The contribution of brain imaging to the understanding of psychopathy. Psychol Med. 2019;49(1):20–31.
- Werner KB, Few LR, Bucholz KK. Epidemiology, comorbidity, and behavioral genetics of antisocial personality disorder and psychopathy. Psychiatr Ann. 2015;45(4):195–199.
- Saltaris C. Psychopathy in juvenile offenders. Can temperament and attachment be considered as robust developmental precursors? Clin Psychol Rev. 2002;22(5):729–752.
- Viding E, McCrory EJ. Understanding the development of psychopathy: progress and challenges. Psychol Med. 2018;48(4):566–577.
- Waller R, Hyde LW. Callous-unemotional behaviors in early childhood: the development of empathy and prosociality gone awry. Curr Opin Psychol. 2018;20:11–16.
- Cutler BL. Encyclopedia of psychology and law. Thousand Oaks (CA): SAGE Publications, Inc.; 2008.
- Hodgins S, Piatosa MJ, Schiffer B. Violence among people with schizophrenia: phenotypes and neurobiology. Curr Top Behav Neurosci. 2014;17:329–368.
- Rhoads SA, Cardinale EM, O’Connell K, et al. Mapping neural activity patterns to contextualized fearful facial expressions onto callous-unemotional (CU) traits: intersubject representational similarity analysis reveals less variation among high-CU adolescents. Personal Neurosci. 2020;3:e12.
- Olver ME, Lewis K, Wong SCP. Risk reduction treatment of high-risk psychopathic offenders: the relationship of psychopathy and treatment change to violent recidivism. Personal Disord. 2013;4(2):160–167.
- Bell C, Tesli N, Gurholt TP, et al. Associations between amygdala nuclei volumes, psychosis, psychopathy, and violent offending. Psychiatry Res Neuroimaging. 2022;319:111416.
- García RR, Aliste F, Soto G. Social cognition in schizophrenia: cognitive and neurobiological aspects. Rev Colomb Psiquiatr (Engl Ed). 2018;47(3):170–176.
- Morice R, Delahunty A. Frontal/executive impairments in schizophrenia. Schizophr Bull. 1996;22(1):125–137.
- Monahan J, Steadman HJ, Appelbaum PS, et al. Developing a clinically useful actuarial tool for assessing violence risk. Br J Psychiatry. 2000;176:312–319.
- Tesli N, Rokicki J, Maximov II, et al. White matter matters: unraveling violence in psychosis and psychopathy. Schizophr Bull Open. 2021;2(1).
- Spitzer RL, Williams JB, Gibbon M, et al. The structured clinical interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–629.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276.
- Coccaro EF, Berman ME, Kavoussi RJ. Assessment of life history of aggression: development and psychometric characteristics. Psychiatry Res. 1997;73(3):147–157.
- Winkler AM, Ridgway GR, Webster MA, et al. Permutation inference for the general linear model. Neuroimage. 2014;92(100):381–397.
- Woodworth M, Porter S. In cold blood: characteristics of criminal homicides as a function of psychopathy. J Abnorm Psychol. 2002;111(3):436–445.
- De Brito SA, Forth AE, Baskin-Sommers AR, et al. Psychopathy. Nat Rev Dis Primers. 2021;7(1):49.
- Hildebrand M, de Ruiter C. PCL-R psychopathy and its relation to DSM-IV axis I and II disorders in a sample of male forensic psychiatric patients in The Netherlands. Int J Law Psychiatry. 2004;27(3):233–248.
- Goethals K, Van Giels M, Ekiz E, et al. Possible correlations between the deficient affective experience and negative symptoms of psychosis: an exploratory study in (forensic) psychiatric patients. Crim Behav Ment Health. 2013;23(5):336–346.
- Ogloff JR. Psychopathy/antisocial personality disorder conundrum. Aust N Z J Psychiatry. 2006;40(6–7):519–528.
- Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16(10):620–631.
- McCleery A, Lee J, Joshi A, et al. Meta-analysis of face processing event-related potentials in schizophrenia. Biol Psychiatry. 2015;77(2):116–126.
- Megreya AM. Face perception in schizophrenia: a specific deficit. Cogn Neuropsychiatry. 2016;21(1):60–72.
- Ayesa-Arriola R, Setién-Suero E, Neergaard KD, et al. Evidence for trait related theory of mind impairment in first episode psychosis patients and its relationship with processing speed: a 3 year follow-up study. Front Psychol. 2016;7(592):592.
- Wong SC, Olver ME. Risk reduction treatment of psychopathy and applications to mentally disordered offenders. CNS Spectr. 2015;20(3):303–310.
- Brunner F, Neumann I, Yoon D, et al. Determinants of dropout from correctional offender treatment. Front Psychiatry. 2019;10:142.
- Klein Haneveld E, Neumann CS, Smid W, et al. Treatment responsiveness of replicated psychopathy profiles. Law Hum Behav. 2018;42(5):484–495.
- Langton CM, Barbaree HE, Harkins L, et al. Sex offenders’ response to treatment and its association with recidivism as a function of psychopathy. Sex Abuse. 2006;18(1):99–120.
- Olver ME, Wong SC. Therapeutic responses of psychopathic sexual offenders: treatment attrition, therapeutic change, and long-term recidivism. J Consult Clin Psychol. 2009;77(2):328–336.
- Skeem JL, Monahan J, Mulvey EP. Psychopathy, treatment involvement, and subsequent violence among civil psychiatric patients. Law Hum Behav. 2002;26(6):577–603.
- Baskin-Sommers AR, Curtin JJ, Newman JP. Altering the cognitive-affective dysfunctions of psychopathic and externalizing offender subtypes with cognitive remediation. Clin Psychol Sci. 2015;3(1):45–57.
- Konicar L, Veit R, Eisenbarth H, et al. Brain self-regulation in criminal psychopaths. Sci Rep. 2015;5:9426.
- Cullen A, Soria C, Clarke AY, et al. Factors predicting dropout from the reasoning and rehabilitation program with mentally disordered offenders. Crim Just Behav. 2011;38:217–230.
- Cullen AE, Clarke AY, Kuipers E, et al. A multisite randomized trial of a cognitive skills program for male mentally disordered offenders: violence and antisocial behavior outcomes. J Consult Clin Psychol. 2012;80(6):1114–1120.
- De Page L, Mercenier S, Titeca P. Assessing psychopathy in forensic schizophrenia spectrum disorders: validating the comprehensive assessment of the psychopathic Personality-Institutional rating scale (CAPP-IRS). Psychiatry Res. 2018;265:303–308.
- Mueser KT, Drake RE, Ackerson TH, et al. Antisocial personality disorder, conduct disorder, and substance abuse in schizophrenia. J Abnorm Psychol. 1997;106(3):473–477.
- Correll CU, Yu X, Xiang Y, et al. Biological treatment of acute agitation or aggression with schizophrenia or bipolar disorder in the inpatient setting. Ann Clin Psychiatry. 2017;29(2):92–107.
- Buckley P, Citrome L, Nichita C, et al. Psychopharmacology of aggression in schizophrenia. Schizophr Bull. 2011;37(5):930–936.
- Morrissette DA, Stahl SM. Treating the violent patient with psychosis or impulsivity utilizing antipsychotic polypharmacy and high-dose monotherapy. CNS Spectr. 2014;19(5):439–448.
- Patchan K, Vyas G, Hackman AL, et al. Clozapine in reducing aggression and violence in forensic populations. Psychiatr Q. 2018;89(1):157–168.
- Belli H, Ural C. The association between schizophrenia and violent or homicidal behaviour: the prevention and treatment of violent behaviour in these patients. West Indian Med J. 2012;61(5):538–543.
- Krakowski M, Tural U, Czobor P. The importance of conduct disorder in the treatment of violence in schizophrenia: efficacy of clozapine compared With olanzapine and haloperidol. Am J Psychiatry. 2021;178(3):266–274.
- Stahl SM, Morrissette DA, Cummings M, et al. California state hospital violence assessment and treatment (Cal-VAT) guideline. CNS Spectr. 2014;19(5):449–465.
- Nolan KA, Czobor P, Roy BB, et al. Characteristics of assaultive behavior among psychiatric inpatients. Psychiatr Serv. 2003;54(7):1012–1016.
- Buzina N, Periša A, Arbanas G. The assessment of psychopathic traits in perpertrators with schizophrenia and psychopathy as comorbidity. Psychiatr Danub. 2021;33(Suppl 4):535–540.
- Abu-Akel A, Heinke D, Gillespie SM, et al. Metacognitive impairments in schizophrenia are arrested at extreme levels of psychopathy: the cut-off effect. J Abnorm Psychol. 2015;124(4):1102–1109.
- Sedgwick O, Young S, Greer B, et al. Sensorimotor gating characteristics of violent men with comorbid psychosis and dissocial personality disorder: relationship with antisocial traits and psychosocial deprivation. Schizophr Res. 2018;198:21–27.
- Guy LS, Douglas KS. Examining the utility of the PCL:SV as a screening measure using competing factor models of psychopathy. Psychol Assess. 2006;18(2):225–230.
- Staniloiu A, Markowitsch H. Gender differences in violence and aggression - a neurobiological perspective. Proc Soc End Behav Sci. 2012;33:1032–1036.
- Lynam DR, Charnigo R, Moffitt TE, et al. The stability of psychopathy across adolescence. Dev Psychopathol. 2009;21(4):1133–1153.
- Sleep CE, Weiss B, Lynam DR, et al. An examination of the triarchic model of psychopathy’s nomological network: a meta-analytic review. Clin Psychol Rev. 2019;71:1–26.
- Cooke DJ, Michie C. Refining the construct of psychopathy: towards a hierarchical model. Psychol Assess. 2001;13(2):171–188.
- Balcioglu YH, Kirlioglu Balcioglu SS, Oncu F, et al. Psychopathy, temperament, and character dimensions of personality as risk determinants of criminal recidivism in schizophrenia patients. J Forensic Sci. 2021;66(6):2340–2353.
- Moran P, Hodgins S. The correlates of comorbid antisocial personality disorder in schizophrenia. Schizophr Bull. 2004;30(4):791–802.
- Newton-Howes G, Austin S, Foulds J. The prevalence of personality disorder in mental state disorder. Curr Opin Psychiatry. 2022;35(1):45–52.
