Abstract
Purpose
To access the attitudes of service users about the sharing of health records for research and to foster collaboration between municipal health services and the specialist health services in Norway.
Methods
Members (n ≈ 2000) of the Norwegian mental health service users’ organizations (SUO’s), ADHD Norway, the Autism Association and the Tourette Association, representing Central Norway, participated in the study, (N = 108, 5.4% response rate). Descriptive statistics were used to evaluate distributions of responses to the questionnaire.
Results
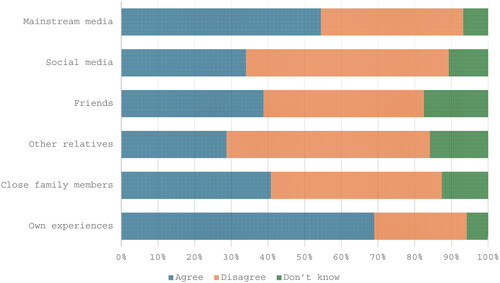
Service users reported being aware that municipal health services collaborate with the specialist health service (62%), with mental health care in the specialist health service (57%), and child and adolescent psychiatric services (61%). A large proportion of individuals were aware of the benefits of sharing their health records (93%), have trust in the use of data by health authorities (81%), and were willing to share records to benefit fellow patients (84%). Personal experience (69%) and impressions from mainstream media (55%) had the most influential impact on users’ views of the Health Platform, an electronic health communication system. A majority of users had a negative perception of the Health Platform, even though some expect it to become a valuable tool in the future (50%).
Conclusions
Service users are aware of and positive about benefiting others by sharing health records. They trust the health authorities, however, have negative attitudes about the Health Platform, apparently based on personal experiences and media influence. However, service users can see the potential usefulness of the Health Platform in the future.
Introduction
Mental disorders are one of the main causes of disability among children and adolescents in Norway [Citation1]. The social costs of mental disorder related disability are considerable, not only to the national health budget, but also because mental health disorders may continue into young adulthood with significant numbers of young people with mental disorders ultimately being unable to join the workforce and contribute to the Norwegian economy [Citation2]. In addition, there is a burden resulting from the suffering of patients and on their social environment, impairment, decreased enjoyment of life and fulfilment, and reduced quality of life [Citation2]. Approximately 7% of Norwegian children and young people 4–14 years of age have a mental disorder at any point in time [Citation3], with almost 11% of these children fulfilling criteria for more than one diagnosis [Citation4]; nearly 6% of all Norwegian children and adolescents are receiving treatment from Norwegian child and adolescent mental health services (CAMHS) [Citation3]. Prevention and early detection of mental disorders require easy access to research-based knowledge, experience-based skills from professionals, and users’ knowledge. Additionally, the exchange of knowledge between service levels and different agencies is also important [Citation5].
In Norway, public primary level health services are operated by municipalities, while public specialist/hospital level services are gathered in four regional health authorities. Acute and emergency services are available on both levels. Child and adolescent mental health care is a specialist service organized as separate clinics (Barne- og ungdomspsykiatri, BUP) only servicing this age group [Citation5]. These Health Authorities are all publicly funded yet maintain separate budgets and health record systems. For child and adolescent mental health care, other municipal and county actors are involved, including schools, educational and psychological counseling services, and child protection agencies, each of which keep separate records, as required by (separate) laws. Until very recently, sharing records across service levels was not legal, leaving collaboration to rely upon explicit communication (within the record systems, or by other, safe means). Different levels of service, overlapping responsibilities, and separate health record systems necessarily lead to some redundancy and significant problems in coordinating care.
In Central Norway, an electronic health communication system, the Health Platform, is being introduced with the goal of solving these challenges in effective mental health care coordination. The Health Platform is intended to provide a single electronic health records (EHRs) system that serves all care levels, and potentially improve communication by enabling sharing of information. For children and adolescents, this may not solve communication problems and improve collaboration because schools, educational, child protection and social services cannot be served by a health record. The introduction of the Health Platform involves not only the health service employees, but also the health service users, i.e. patients and their families. In Norway, for the past 20 years, the health service users has played an increasing important role. Today, service users’ participation is an integral part of all phases of research and development work, as well as in the training of new healthcare personnel [Citation6,Citation7]. Service users have been recognized as important stakeholders in the development of healthcare services, organizations, and policies. Their feedback, based on their own experience, is essential for mapping the needs and challenges in attempt to ensure good health services for all [Citation8].
Service user organizations (SUOs) have been increasingly effective in providing valuable feedback on mental health services and healthcare interventions. EHRs have been used for the purpose of care, quality control, and research [Citation9–12]. In 2021, Bakken, et al. conducted a study of mental health service users investigating their awareness of, and attitudes towards health authorities storing and sharing of EHRs, as well as their opinions surrounding the purposes of the EHR data storage and dissemination [Citation13]. It was found that respondents were aware of and in support of sharing EHR data for research, clinical care practices, and decision support with the latter used in clinical decision support systems (CDSSs) in CAMHS [Citation5,Citation14,Citation15].
The present study aimed to 1) access mental health service users’ opinions about collaboration between municipal services and the specialist health service; 2) investigate service users’ awareness of health authorities sharing EHRs information; and 3) identify service users’ expectations towards the Health Platform.
Material and methods
Participants, procedure and data collection
This study is part of the Individual Digital Decision Assist System (IDDEAS) innovation project and was conducted in Norway. All registered members of three SUOs: ADHD Norway, the Autism Association and the Tourette Association in Central Norway concerned with children and adolescents and their parents and relatives were invited to participate in the study (n ≈ 2000). Participants were recruited via email by ADHD Norway.
Participants were invited to complete an online, anonymous questionnaire (available in supplemental materials) by email which contained a link to the online survey. This method corresponds to Bakken et al. (2022), and we presumed that potential survey-media dependent response and participation also would be similar. One of the reasons for choosing this way of collecting the data was that Norway is relatively sparsely populated, with long distances between communities making it difficult to reach participants. Also, after the COVID-19 pandemic, it is becoming more common and easier to collect data using online questionnaires. The average time for survey completion was approximately 20 min. ADHD Norway, in collaboration with Vårres regional user-led center Mid Norway, assisted in converting the original questionnaire into an internet based EasyQuest survey form.
Data collection took place in January – March 2023, with a reminder to complete the questionnaire being sent in the middle of the data collection period. Identifiable data were collected and sent to Vårres regional user-led center Mid Norway for safekeeping and then encrypted sharing anonymized data with the investigators. A passcode was used for safe data sharing with co-authors.
Questionnaire
The first part of the questionnaire included three questions assessing whether participants are aware of cooperation between community health care (GP’s) service providers and specialist health care service providers with answer alternatives ‘Yes’ and ‘No.’ Next, they were asked about opinions on the level of collaboration between municipal health services and the specialist health service with four questions using a 6-point Likert scale with item response categories on a continuum from ‘To a very large extent agree’ to ‘To a very large extent disagree’ and ‘Don’t know’.
The second part of the questionnaire included five questions on a 5-point Likert scale created to assess participants’ attitudes on the sharing of medical record information within the health services. Item response categories were on a continuum from ‘Very positive’ to ‘Very negative’.
The third part of the questionnaire asked the participants whether they: 1) know what the Health Platform is; 2) are aware that the Health Platform has been adopted in some of the health services in Central Norway; and 3) have been involved in the development or introduction of the Health Platform. If a participant had a positive answer to at least one of these questions, he/she was asked to continue to answer 13 additional items focusing on their opinions, perceived understanding and expectations for the Health Platform, using a 5-point Likert scale with item response categories on a continuum from ‘Very positive’ to ‘Very negative’ (two items), and a 5-point Likert scale with item response categories on a continuum from ‘To a very large extent agree’ to ‘To a very large extent disagree’ and ‘Don’t know’ (11 items).
The final part of the questionnaire consisted of nine background questions, including questions regarding participant gender, age, ethnicity, family situation, education, work situation, whether they live permanently in their area of residence, and how long they had been a member of a SUO.
Ethical considerations
The Regional Ethical Committee concluded that this study was outside their remit and advised investigators to seek approval from the Norwegian Centre for Research Data (NSD). NSD approved the study on 21.12.2022 (reference number 989077).
Analysis
We analyzed quantitative data with SPSS, version 25.0. Descriptive statistical analyses were implemented to demonstrate the distributions of demographic characteristics and individual responses to the questions included in the questionnaire.
Results
Demographic characteristics
Of a total of a 2000 SUOs members were invited to participate in the study, 108 answers were received, yielding a 5.4% response rate ().
Table 1. Baseline characteristics of the study group (N = 108).
Awareness of the collaboration between municipal health services and the specialist health services
Most service users were aware that municipal health services collaborate with the specialist health service (62%), with mental health care in the specialist health service (57%), and with child and adolescent psychiatric services (61%).
38% of the service users were agreeable with the cooperation between the GPs and BUP in the specialist health service while 25% were unsure. Half of the participants (51%) agreed that BUP cooperates well with other involved municipal services, such as schools, educational psychology service, child protection, and kindergartens; 24% disagreed. Most service users (79%) reported that there is a need for more exchange of information between GPs and BUP and that there is a need for joint knowledge across services and service levels to support development of decision support systems (93%).
Participants’ attitudes towards data-sharing
Most service users (83%) reported that it is ethical to share health records for healthcare and research and 81% trusted health authorities with record sharing. Even more (84%) were willing to share their records to help others with similar diagnoses and indicated benefits from sharing (93%).
Participants’ perceptions and expectations towards the Health Platform
Of total 108 participants, 92 subjects (85.2%) reported that they knew what the Health Platform was, 102 (94.4%) were aware about the adoption of the Health Platform in Central Norway and 13 subjects (12%) reported being involved in the development and introduction of the Health Platform in the region. Altogether, 102 subjects (94.4%) participated in the last section of the survey proving information about the Health Platform.
In general, majority of service users (62%) reported a negative perception of the Health Platform with only 13% being positive and 25% neutral. At the same time, when being asked about their expectations toward the Health Platform, their answers were equally distributed with 36% positive, 32% negative and 32% neutral. 48% of the participants reported that the Health Platform will eventually become a good working tool in their care. More results are presented in .
Table 2. Participants’ expectations towards the Health Platform.
Participants were further asked about which factors have influenced their view of the Health Platform. Results are presented in .
Discussion
This study examined the opinions of mental health service users about collaboration between municipal general health services and specialist health services, their awareness that health authorities share EHR information, and expectations about the newly-deployed EHR, the Health Platform.
Findings indicate concern about poor cooperation between GPs and child and adolescent psychiatric service providers, and a need for improving information exchange between these services. This is consistent with those of Tveit and Dahli [Citation16] who found limited cooperation between GPs and the specialist health service for mental health care. Similar findings were reported in a study by Mykletun et al. [Citation17], in which one hundred GPs in Norway were interviewed with the majority reporting a need for improved cooperation between these services.
Our data on service user’s awareness that health authorities share EHRs information are similar to those of Bakken et al. (2022) who reported that most of the service users considered it ethical to share health records for healthcare and research, and also trusted the health authorities with record sharing. They also found that over two-thirds of service users were willing to share their own records to help others with similar diagnoses and recognized the benefits from sharing EHRs information [Citation13]. Our results similarly demonstrate that service users are aware and approve of information sharing, as they recognize the benefits of doing so.
Even though the Health Platform has much potential and many advantages, there are also associated problems. A 2023 survey study of nurses at the St. Olav’s hospital (Trondheim, Norway), conducted by the Norwegian Nurses Organization, showed that many participants were unsure if patient records were correct and up-to-date; almost two-thirds of the nurses believed that the introduction of the Health Platform led to greater work pressure, with one-third reporting that they considered quitting their jobs due to an increased workload related to the Health Platform [Citation18]. The Norwegian Health Authorities has also criticized the new system, pointing to several deviations and problems related to implementation of the Health Platform. These circumstances led to at least a one-year postponement in the full implementation of the Health Platform in Central Norway, with an enormous increase of associated costs [Citation19]. The results of the present study show that almost half of service users reported a currently negative perception of the Health Platform. This negative perception may be a result of all the problems with implementation of the Health Platform, and reports in the media. On the other hand, one-third of the participants demonstrated positive expectations towards the Health Platform in the future and half of all participants opined that the Health Platform could eventually become a beneficial tool in the future. Our results point out that, even though the current perceptions of the Health Platform are mostly negative, respondents expressed optimism that the Health Platform will eventually solve the communication problems and have expectations that the Health Platform has the potential to be a valuable and useful tool for both the specialists and the patients.
Participant views of the Health Platform largely appear to be based on their own experience and impressions from mainstream media. Recent public debates about the Health Platform in the media [Citation20,Citation21] have had an impact on the views surrounding the Health Platform. Most health workers are afraid to share health information because of the duty of confidentiality. However, users are more concerned about the lack of sharing of necessary information so that the services can provide optimal care. And many public reports point precisely to a lack of interaction between the services as the biggest challenge to being able to give patients the best possible follow-up [Citation22]. Simple way around this problem is to ask for the patient’s consent for sharing information about their problems.
Strengths and limitations
To our knowledge, this is the only study that has explored the perceptions of mental health service users on the Health Platform. The main strength of the study is that it elicits opinions of mental health service users, who are often underrepresented in research. The study has several limitations. First, it is a relatively small sample with a low response rate. There is also a lack of balance in the gender distribution with disproportionately more women respondents in our sample. Similarly, the respondents are mostly Norwegian with few other ancestries represented. A relatively small portion of the sample was unemployed. At the time of the survey, very few of the service users had any individual experience with the Health Platform. As only three service-users organizations were invited for participation in the study, the results cannot be generalized to all service users/members of the health care community in Central Norway. The survey was anonymous, meaning that we did not have access to information about non-responders such as age, gender, and socio-economic status to compare with the data from responders.
Future actions
The study revealed the contradiction between, on the one hand, the high level of approval for the collection and exchange of data in the context of cooperation between different services and, on the other hand, the rather negative attitude towards the Health Platform which is intended to facilitate this desired cooperation. This contradictory expectation may have the potential to adversely impact the effectiveness of the Health Platform. This information will be shared with health platform management with the hope they will address these concerns with their end users. It should also be the subject to further investigation and taken up in the professional and health policy debate.
Conclusions
Service users demonstrate awareness of a need for and the fact of cooperation between the municipal health services, the specialist health service and BUP. They are aware of the need for more information exchange between these services. Most users approve of close cooperation between different services for clinical benefit. The study demonstrated that service users approve of information sharing, and they see the benefits of sharing. Finally, despite most of the service users having a negative perception of the Health Platform, they are optimistic that shared record systems will ultimately be a useful component of the care system in the future to come.
Supplemental Material
Download MS Word (34.8 KB)Supplemental Material
Download MS Word (34.3 KB)Disclosure statement
The authors report no financial relationships with commercial interests.
Data availability statement
Requests to access the datasets should be directed to Professor Norbert Skokauskas.
Additional information
Funding
Notes on contributors
Roman Koposov
Dr. Roman Koposov, MD, PhD, is a Professor at the Center of Child and Adolescent Mental Health and Welfare, UiT - the Arctic University of Norway, Tromsø, Norway. He has participated in a series of international studies on different aspects of child and adolescent mental health in young offenders and adolescents from general population.
Line Stien
Line Stien, MSc, received at the Umeå University, Umeå, Sweden.
Carolyn Clausen
Carolyn Clausen, MSc, is a PhD student at the Centre for Child and Adolescent Mental Health and Child Protection, Department of Mental Health, Faculty of Medicine and Health Sciences, the Norwegian University of Science and Technology (NTNU), Trondheim, Norway.
Bennett Leventhal
Dr. Bennett Leventhal is the Irving B. Harris Professor of Child and Adolescent Psychiatry, emeritus, at the University of Chicago, Chicago, USA. He continues to be an active clinician, investigator, and teacher serving trainees and families around the world.
Odd Sverre Westbye
Odd Sverre Westbye, MSc, is a University Lecturer at the Centre for Child and Adolescent Mental Health and Child Protection, Department of Mental Health, Faculty of Medicine and Health Sciences, NTNU, Trondheim, Norway and adviser at the Department of Child and Adolescent Psychiatry, St. Olavs Hospital, Trondheim, Norway.
Øystein Nytrø
Øystein Nytrø, PhD, is a Professor at the Department of Computer Science at the UiT - the Arctic University of Norway, Tromsø, Norway and at the Department of Computer Science, Norwegian University of Science and Technology, Trondheim, Norway.
Kaban Koochakpour
Kaban Koochakpour, MSc, is a PhD student at the Faculty of Information Technology and Electrical Engineering, NTNU, Trondheim, Norway.
Dipendra Pant
Dipendra Pant, MSc, is a PhD student at the Department of Computer Science, NTNU, Norway, holds an ME in Computer Engineering from Kathmandu University, Nepal. He has experience as a web developer and academic coordinator, with research interests in machine learning, data mining, clinical decision support, and health informatics.
Thomas Brox Røst
Thomas Brox Røst, PhD, is a general manager at the Vivit AS, a health informatics company, Trondheim, Norway.
Arthur Mandahl
Arthur Mandahl, is a chief executive officer at the Vårres user-led center Middle Norway, Trondheim, Norway.
Hege Hafstad
Hege Hafstad is a project coordinator at the Vårres user-led center Middle Norway, Trondheim, Norway..
Norbert Skokauskas
Dr. Norbert Skokauskas, MD, PhD, is a Professor of Child and Adolescent Psychiatry at the Centre for Child and Adolescent Mental Health and Child Protection, Department of Mental Health, Faculty of Medicine and Health Sciences, NTNU, Trondheim, Norway.
References
- Brage S, Thune O. Young disability and mental illness (In Norwegian). Arbeid og velferd. 2015. http://www.ung-uforhet-og-psykisk-sykdom.pdf
- Folkehelsemeldingen—Mestring og muligheter. Meld. St. 19 (2014-2015) - regjeringen.no. 2015. https://www.regjeringen.no/no/dokumenter/meld.-st.-19-2014-2015/id2402807/sec3?q=livsgledesykehjem
- Institute of Public Health (FHI). Psykiske plager og lidelser hos barn og unge (in Norwegian). 2023. https://www.fhi.no/he/folkehelserapporten/psykisk-helse/psykisk-helse-hos-barn-og-unge/?term=.
- Bøe T, Heiervang ER, Stormark KM, et al. Prevalence of psychiatric disorders in Norwegian 10-14-year-olds: results from a cross-sectional study. PLoS One. 2021;16(3):e0248864. doi:10.1371/journal.pone.0248864.
- Røst TB, Clausen CE, Nytrø Ø, et al. Local, early, and precise: designing a clinical decision supports system for child and adolescent mental health services. Front Psychiatry. 2020;11:564205. doi:10.3389/fpsyt.2020.564205.
- Andreassen TA. Service user involvement and repositioning of healthcare professionals: a framework for examining implications of different forms of involvement. Nordic Welfare Research. 2018;3(1):58–69. doi:10.18261/issn.2464-4161-2018-01-06.
- Tierney E, McEvoy R, O’Reilly-de Brún M, et al. A critical analysis of the implementation of service user involvement in primary care research and health service development using normalization process theory. Health Expect. 2016;19(3):501–515. doi:10.1111/hex.12237.
- Omeni E, Barnes M, MacDonald D, et al. Service user involvement: impact and participation: a survey of service user and staff perspectives. BMC Health Serv Res. 2014;14(1):491. doi:10.1186/s12913-014-0491-7.
- Weitzman ER, Kaci L, Mandl KD. Sharing medical data for health research: the early personal health record experience. J Med Internet Res. 2010;12(2):e14. doi:10.2196/jmir.1356.
- O’Brien EC, Rodriguez AM, Kum H-C, et al. Patient perspectives on the linkage of health data for research: insights from an online patient community questionnaire. Int J Med Inform. 2019;127:9–17. doi:10.1016/j.ijmedinf.2019.04.003.
- Kim J, Kim H, Bell E, et al. Patient perspectives about decisions to share medical data and biospecimens for research. JAMA Netw Open. 2019;2(8):e199550. doi:10.1001/jamanetworkopen.2019.9550.
- Shen N, Sequeira L, Silver MP, et al. Patient privacy perspectives on health information exchange in a mental health context: qualitative study. JMIR Ment Health. 2019;6(11):e13306. doi:10.2196/13306.
- Bakken V, Koposov R, Røst TB, et al. Attitudes of mental health service users toward storage and use of electronic health records. Psychiatr Serv. 2022;73(9):1013–1018. doi:10.1176/appi.ps.202100477.
- Clausen CE, Leventhal BL, Nytrø Ø, et al. Clinical decision support systems: an innovative approach to enhancing child and adolescent mental health services. J Am Acad Child Adolesc Psychiatry. 2021;60(5):562–565. doi:10.1016/j.jaac.2020.09.018.
- Koposov R, Fossum S, Frodl T, et al. Clinical decision support systems in child and adolescent psychiatry: a systematic review. Eur Child Adolesc Psychiatry. 2017;26(11):1309–1317. doi:10.1007/s00787-017-0992-0.
- Tveit GO, Dahli MP. Samarbeid med fastlegene kan bringe psykologene nærmere dem som trenger det, men systemet legger ikke til rette for det (in Norwegian). Forskersonen.no 2019.
- Mykletun A, Knudsen AK, Tangen T, et al. General practitioners’ opinions on how to improve treatment of mental disorders in primary health care. Interviews with one hundred Norwegian general practitioners. BMC Health Serv Res. 2010;10(1):35. doi:10.1186/1472-6963-10-35.
- Sykepleien. 2023. https://sykepleien.no/2023/01/helseplattformen-pa-st-olavs-hospital-27-prosent-av-sykepleierne-har-vurdert-slutte
- Simonsen MC. Helse Midt-Norge skal vurdere utsettelse av Helseplattformen i ekstraordinært styremøte. Dagens medisin. 2023.
- NRK. 2023. https://www.nrk.no/emne/helseplattformen-1.15838445
- https://www.vg.no/tag/helseplattformen
- https://www.regjeringen.no/no/dokumenter/nou-2017-12/id2558211/