ABSTRACT
Clinical relevance
Understanding changes in ocular anatomical parameters after intraocular lens implantation will allow a more accurate determination of dioptric power prior to surgery.
Background
The crystalline lens position might change due to the implantation and removal of an implantable collamer lens (ICL) or toric implantable collamer lens (TICL). This study aimed to assess the effect of ICL implantation on position of the crystalline lens.
Methods
This retrospective study was conducted on patients who underwent V4c ICL or V4c TICL implantation between March and September, 2018. Preoperative and post-operative (2 weeks, 3 months and 6 months) axial length, central corneal thickness, crystalline lens position, crystalline lens thickness and vault height were analysed. Multivariable linear regression was used to determine the variables associated with 6-month changes in lens position.
Results
This study included 117 eyes of 117 patients. There were decreases in all vertical distance measures from the central corneal endothelium to the anterior and posterior crystalline lens capsule (all p > 0.05). The amount of reduction was related to the crystalline lens position before the operation and crystalline lens thickness after the operation (all p < 0.01). An error in anterior chamber depth and lens thickness may appear when the ICL/TICL is close to the crystalline lens.
Conclusion
Phakic intraocular lens implantation resulted in lens thickening and forward movement on day 1 post-operatively, which becomes stable within 6 months. Preoperative lens position and post-operative lens thickness were related to the amount of movement.
Introduction
With the development of novel tools and materials, the safety and effectiveness of refractive surgery continues to improve.Citation1,Citation2 Refractive surgery can improve not only uncorrected distance visual acuity, but also visual quality. Currently, refractive surgery primarily includes corneal and intraocular refractive surgeries. These two types of surgery have their unique advantages and the relevant option is selected according to the circumstances of patients, in a comprehensive and individualised manner.
Intraocular refractive surgery includes posterior chamber intraocular lens (IOL) implantation and implantable collamer lens (ICL) implantation.Citation3 ICL has unique clinical advantages such as a large correction range,Citation4 good visual quality,Citation5,Citation6 predictability,Citation7,Citation8 preservation of corneal tissue integrity, and reversibility. However, a few post-operative complications have been reported.Citation9–11 Therefore, clinicians need to evaluate the patient correctly and plan for possible post-operative complications.
Previous studies on the spatial parameters of intraocular structures after ICL implantation mainly focused on ICL safety indicators such as anterior chamber depth, arch height and chamber angle.Citation12–15 Data on the impact of ICL on ocular anatomy, especially the location of the crystalline lens inside the eye, in Chinese patients are limited.
Studies suggest that some of the crystalline lenses correctly implanted with an ICL suffer from decreased transparency, affecting visual quality, because of ageing or metabolic changes in the crystalline lens.Citation16,Citation17 In addition, due to the increasing number of patients who undergo ICL implantation, the number of patients with ICL requiring cataract surgery is also increasing.Citation18 Although some studies have reported the safety, effectiveness and predictability of ICL removal with cataract extraction and pseudophakic IOL implantation,Citation19–21 effect of the ICL on the calculation of IOL dioptre remains unknown.
The present study hypothesised that the position of the crystalline lens changes due to the implantation and removal of the ICL. If such a phenomenon exists and the calculation of IOL dioptric power is completed before removing the ICL, an error will be induced due to a more anterior effective lens position (ELP), which would reduce the accuracy of IOL dioptric power selection. Therefore, the purpose of this study was to assess the effect of the ICL on the position of the crystalline lens.
Methods
Study design and patients
This retrospective study included patients who underwent V4c ICL or V4c toric ICL (TICL) implantation between March and September 2018 at the Eye Hospital. Approval was obtained from the Hospital Institutional Review Board [MSKLL20180405]. All procedures in this study adhered to the tenets of the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature of the study.
Inclusion criteria were: 1) 20–55 years of age; 2) presence of myopia with a manifest refraction spherical equivalent between–1.00 and–21.00 D; 3) astigmatism between 0.00 and–5.00 D; 4) eyes that underwent V4c ICL or V4c TICL implantation performed by the same experienced surgeon (JZ); 5) follow-up period of > 6 months; and 6) no ICL adjustment during the first 6 months of follow-up.
Exclusion criteria were: (1) existing ocular conditions such as keratoconus, crystalline lens deformity, crystalline lens heterotopia, glaucoma, cataract, uveitis, retinal detachment or macular degeneration; (2) previous ocular or intraocular surgery; (3) acute or chronic corneal infection; (4) endothelial cell density < 2000 cells/mm; (5) anterior chamber distance from the endothelium < 2.8 mm; (6) nasal or temporal iridocorneal angle < 30°; or (7) anterior synechia in any region of the iris.
Stratified sampling was performed for the inclusion of the eyes, excluding the symmetry of both eyes.
Preoperative and post-operative examination
All patients underwent complete a ophthalmic examination, including uncorrected and corrected distance visual acuity (UCDVA and CDVA) (Snellen lines), spherical equivalent (SE), slit lamp microscopy, intraocular pressure (IOP), anterior segment tomography (Sirius; CSO, Florence, Italy), biometry (IOLMaster 700; Carl Zeiss, Jena, Germany), optical coherence tomography (OCT) (Cirrus HD-OCT 5000; Carl Zeiss, Jena, Germany) and ultrasound biomicroscopy (UBM; VuPad B; Sonomed Escalon, NY, USA).
An independent physician performed all UBM examinations using a 50-MHz transducer. Before the examination, the patients were instructed to avoid visual display terminal equipment or books for at least 3 hours.Citation21 Each measurement was performed by one physician.
Central corneal thickness (CCT) and horizontal white-to-white (WTW) diameter were obtained using anterior segment tomography. Horizontal and vertical sulcus-to-sulcus (STS) diameters were obtained using the UBM. The axial length (AL) of the eye was obtained using biometry. The crystalline lensposition (LP) (the vertical distance from the central corneal endothelium to the anterior crystalline lens capsule) and vault (the distance between the posterior surface of the ICL/TICL and the anterior surface of the crystalline lens capsule) were measured manually using the built-in caliper tool of the OCT equipment.
Crystalline lens thickness (LT) was obtained using biometry; however, it had to be confirmed manually. If a device identification error was found (), LT was calibrated by subtracting the distance from the front surface of the ICL/TICL to the lens using the OCT images. All measurements were taken from the most central point. Three readings were taken and an average value was obtained as the result.
Phakic intraocular lens
During the study period, V4c ICL or V4c TICL (STAAR Surgical, Nidau, Switzerland) was used. The ICL/TICL size and intraocular orientation were decided based on horizontal or vertical STS. Four ICL sizes (12.1, 12.6, 13.2 and 13.7 mm) were selected. Conventionally, the size of the implanted ICL should be larger than the STS. The ICL/TICL power was selected from the website of the manufacturer.
Surgical procedure
The same process was consistently used for each ICL selected. The surgery was performed using a 3 mm clear temporal corneal incision after dilating the pupil with 0.5% phenylephrine and 0.5% tropicamide (Mydrin-P, Santen Pharmaceutical Co. Ltd., Osaka, Japan) under topical anaesthesia. The ICL/TICL was inserted using an injector cartridge and rotated to the target position and orientation, with sodium hyaluronate (Qisheng; Qisheng, Shanghai, China) filling the anterior chamber. The sodium hyaluronate was removed at the end of the surgery.
Following surgery, fluorometholone 0.1% (Flumetholon; Santen Pharmaceutical) and bromfenac sodium 0.1% were immediately administered topically. Levofloxacin 0.3% (Cravit; Santen, Osaka, Japan) was administered topically four times a day for 1 week. Fluorometholone 0.1% was administered topically four times a day for 3 weeks, after which its frequency was tapered to three times a day for 1 week, and then twice a day for 1 week, and finally discontinued.
Data collection
AL, CCT, LP, LT () and vault height data were collected preoperatively and at two weeks, 3 months, and 6 months postoperatively and analysed.
Statistical analysis
Categorical variables are presented using n (%). Continuous variables are presented using means ± standard deviations. The Kolmogorov–Smirnov test was used to confirm the Gaussian distribution of the data. Mauchly’s sphericity test was used to confirm that the covariance matrix composed of time points had spherical characteristics.
Repeated measures analysis of variance (ANOVA) with unequal distance was used to assess the anatomical parameters at different examination points. The pre- and postoperative anatomical parameters were confirmed to have a Gaussian distribution but did not meet the Mauchly’s test of sphericity (Greenhouse–Geisser < 0.7). Therefore, the Bonferroni test was used for multivariable statistical analysis and comparisons between each group, after a degree of freedom Greenhouse–Geisser correction. Multivariable linear regression was used to evaluate the correlation between 6-month changes in LP, and multiple variables, including SE, age, CCT, IOP, AL, LP, LT, post-operative AL, post-operative LP, post-operative LT and vault height.
When two independent variables were correlated, only one of the two was included in the multivariable model to avoid covariates. Two-tailed P-values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS 19.0 (IBM, Armonk, NY, USA).
Results
Characteristics of the patients
A total of 117 eyes of 117 patients were included in this study. Of these patients, 76.1% (89/117) were female, and 52% (61/117) of the eyes were right eyes. The average age of patients was 25.4 ± 6.0 (range, 20–47) years. The SE was—10.69 ± 3.12 D. The baseline characteristics of patients are summarised in .
Table 1. Baseline characteristics of patients.
Anatomical parameters
The anatomical parameters of the eyes of patients included in the study are summarised in . The changes in AL, LP, LT and LP + LT are shown in . Post-operative vault height did not change significantly over time (P = 0.367). The AL was longer after surgery than that before surgery (P < 0.001). The LP was shorter after surgery than that before surgery (P < 0.001). After surgery, the lens was thicker than that before surgery (P < 0.001). Still, the LP + LT was shorter after surgery than that before surgery (P < 0.001). The 6-month changes in LP and LP + LT were 0.16 ± 0.04 mm and 0.11 ± 0.11 mm, respectively.
Table 2. Anatomical parameters.
Correlations
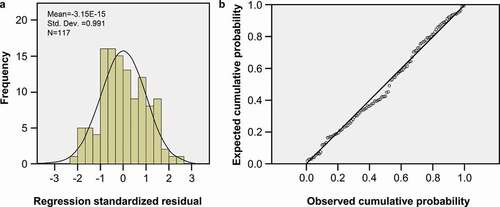
The 6-month changes in LP met the Gaussian distribution and the equivariance criterion (). The matrix shows that the 6-month changes in LP had a linear relationship with LP, LT and post-operative LT. A correlation was also observed among LP, LT and post-operative LT; especially, LT and post-operative LT were completely and positively correlated (P < 0.05). Therefore, the other variables that did not conform to the linear relationship were excluded.
Figure 4. The 6-month changes in LP meet the Gaussian distribution. a. Histogram of regression standardised residual of post-operative 6-month decrease in LP. b. Normal P-P plot of regression standardised residual of post-operative 6-month decrease in LP.
In order to introduce the variables with a strong joint effect in the model, the regression method was selected to exclude the LT variables. The results showed that the variables were suitable for linear regression (Durbin–Watson test = 2.043). The regression model was statistically significant (F = 10.02, P < 0.001); however, the model explains only a small proportion of the decrease in the 6-month LP (adjusted R2 = 0.135). The coefficients of the multivariable linear regression analyses are summarised in .
Table 3. Multivariable linear regression analyses for decrease in LP in 6 months.
Discussion
The present study aimed to compare the ocular anatomical parameters after V4c ICL/TICL implantation. The main result of this study is that the LP decreased and stabilised within 6 months after the ICL/TICL implantation. The changes were positively correlated with preoperative LP and negatively correlated with postoperative LT, suggesting that the anterior surface of the crystalline lens moved forward and that this change remained stable during the 6-month follow-up period. Therefore, in eyes with larger LP, the changes in the longitudinal position of the crystalline lens might be more important.
However, the accuracy of regression analysis using the above parameters is poor, and there is a lack of an accurate quantitative derivation method to predict the forward movement of the crystalline lens. In addition, after V4c ICL/TICL implantation, the crystalline lens expanded significantly, the posterior surface of the crystalline lens moved forward, and both fluctuated during the observation period. Nevertheless, neither returned to the pre-operative state at the end of the examination.
Possible causes of this phenomenon cannot be determined based on the present study. Nevertheless, there was no significant reduction in the postoperative ocular AL compared with that before the surgery. Therefore, there are possibly no oblate ellipsoid changes in the ocular shape caused by the supporting force of the ICL/TICL foot loop. Hence, due to a significant increase in post-operative crystalline LT compared with that before surgery, the authors speculate that the expansion of the crystalline lens and movement of its posterior surface might be related to stimulation of the ciliary body by the ICL/TICL foot loop, pulling the crystalline lens forward.
Further studies are required to understand the duration of this phenomenon and return of the crystalline lens to its original position after ICL removal. Studies suggest that this expansion and movement process may continue until removal of the ICL because of the stable refractive state after ICL/TICL implantationCitation22 and the average dioptric power in low hyperopia.Citation19 Once the ICL is removed, the crystalline lens could return to its original position. This allows optimisation of the expected dioptric correction after ICL/TICL implantation.
At present, the method to obtain the expected dioptric correction after ICL/TICL implantation is based on the online tools provided by the manufacturer. This method has shown good predictability.Citation7 Nevertheless, the forward movement of the crystalline lens after ICL/TICL implantation has not been reported before, and it has not been included in the calculation process. The present study might play a further role in optimising the accuracy of the prediction of post-operative refraction.
At present, many IOL power calculation formulas used to calculate ELP are based on the original anterior chamber depth.Citation23–25 The increase in the anterior chamber depth after ICL removal will make the estimated value of ELP lower than the true value, resulting in hyperopia drift after IOL implantation. Fortunately, the increase in anterior chamber depth after ICL removal should be limited, and patients who undergo ICL implantation mostly have myopia with longer AL.
The removal of the ICL and phacoemulsification with the IOL implantation has good predictability as the effect is usually less than 0.50 D.Citation19–21 However, for patients with short AL, the effect might exceed 0.50 D, which is clinically significant. Finally, the forward movement of the crystalline lens and increase in LT might cause abnormal accommodation function, which needs further evaluation.
Another finding of the present study is the increase in ocular AL 6 months post-operatively. This result might be related to the average age and average myopia dioptric power of the selected population; however, an increase of 0.02 mm in the AL, although statistically significant, has no clinical significance.
During data collection, it was observed that hen the ICL/TICL was close enough to the crystalline lens, an error might appear in recognising the front surface of the ICL/TICL and the anterior capsule of the crystalline lens due to incorrect judgment by the IOLMaster (). This error was encountered in 12.8% (15/117) of the eyes in the present study. Of these, the ratio of patients with vault height above 500 μm was 0.0% (0/48); between 300 and 500 μm was 10.9% (5/46); and below 300 μm was 43.5% (10/23). The highest vault height was 450 μm, and the mean error in the anterior chamber depth and LT was 0.47 ± 0.08 μm. This error can cause significant clinical effects.
One study has shown that eyes with a shallow anterior chamber and a forward LP have lower vaults.Citation26 On the other hand, another study found that different positions of the ICL in the posterior chamber still resulted in postoperative vault height being in the ideal position.Citation27 However, in the present study, the vault height did not change after surgery. Hence, the exact impact of ICL implantation on the eye’s anatomical parameters remains to be examined.
The present study has some limitations. This was mostly a preliminary study of the influence of the primary stage of ICL/TICL on ocular anatomical parameters. Hence, the exact effect will need to be confirmed with a larger sample size. Moreover, future studies need to further evaluate whether the LP of the crystalline lens will change after ICL removal. All of patients included in the present study had normal AL, and those with significantly shorter or longer AL were not included. Therefore, changes in the longitudinal position of the crystalline lens after implantation in these patients were not analysed.
In conclusion, ICL implantation resulted in lens thickening and a small movement forward at day 1 postoperatively, and these changes were stable over 6 months. Preoperative LP and postoperative LT were related to the amount of movement. The changes in the longitudinal position of the crystalline lens might be more important in cases of eyes with larger LP than those in eyes with smaller LP. Therefore, attention needs to be directed towards errors in judgment from biometry data following IOL implantation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Zhang J, Zheng L, Zhao X, et al. Corneal aberrations after small-incision lenticule extraction versus Q value-guided laser-assisted in situ keratomileusis. Medicine (Baltimore). 2019;98:e14210.
- Zhang J, Zheng L, Zhao X, et al. Corneal biomechanics after small-incision lenticule extraction versus Q-value-guided femtosecond laser-assisted in situ keratomileusis. J Curr Ophthalmol. 2016;28:181–187.
- Hernandez-Rodriguez CJ, Pinero DP. A systematic review about the impact of phakic intraocular lenses on accommodation. J Optom. 2020;13:139–145.
- Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102:177–181.
- Alfonso JF, Lisa C, Alfonso-Bartolozzi B, et al. Collagen copolymer toric phakic intraocular lens for myopic astigmatism: one-year follow-up. J Cataract Refract Surg. 2014;40:1155–1162.
- Lim DH, Lee MG, Chung ES, et al. Clinical results of posterior chamber phakic intraocular lens implantation in eyes with low anterior chamber depth. Am J Ophthalmol. 2014;158:447–454 e441.
- Bhandari V, Karandikar S, Reddy JK, et al. Implantable collamer lens V4b and V4c for correction of high myopia. J Curr Ophthalmol. 2015;27:76–81.
- Chang JS, Meau AY. Visian collamer phakic intraocular lens in high myopic Asian eyes. J Refract Surg. 2007;23:17–25.
- Schmidinger G, Lackner B, Pieh S, et al. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology. 2010;117:1506–1511.
- Gonvers M, Bornet C, Othenin-Girard P. Implantable contact lens for moderate to high myopia: relationship of vaulting to cataract formation. J Cataract Refract Surg. 2003;29:918–924.
- Alfonso JF, Lisa C, Abdelhamid A, et al. Three-year follow-up of subjective vault following myopic implantable collamer lens implantation. Graefes Arch Clin Exp Ophthalmol. 2010;248:1827–1835.
- Garcia-De la Rosa G, Olivo-Payne A, Serna-Ojeda JC, et al. Anterior segment optical coherence tomography angle and vault analysis after toric and non-toric implantable collamer lens V4c implantation in patients with high myopia. Br J Ophthalmol. 2018;102:544–548.
- Steinwender G, Varna-Tigka K, Shajari M, et al. Anterior subcapsular cataract caused by forceful irrigation during implantation of a posterior chamber phakic intraocular lens with a central hole. J Cataract Refract Surg. 2017;43:969–974.
- Khalifa YM, Goldsmith J, Moshirfar M. Bilateral explantation of Visian Implantable Collamer Lenses secondary to bilateral acute angle closure resulting from a non-pupillary block mechanism. J Refract Surg. 2010;26:991–994.
- Guber I, Chokri L, Majo F. [Preoperative sizing of the TICL (Toric Implantable Collamer Lens): the largest was too small!]. Klin Monbl Augenheilkd. 2012;229:457–458.
- Sanders DR, Doney K, Poco M, et al. United States food and drug administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111:1683–1692.
- Alfonso JF, Lisa C, Fernandez-Vega L, et al. Prevalence of cataract after collagen copolymer phakic intraocular lens implantation for myopia, hyperopia, and astigmatism. J Cataract Refract Surg. 2015;41:800–805.
- Yan P, Yao L, Li H, et al. The methodological quality of robotic surgical meta-analyses needed to be improved: a cross-sectional study. J Clin Epidemiol. 2019;109:20–29.
- Morales AJ, Zadok D, Tardio E, et al. Outcome of simultaneous phakic implantable contact lens removal with cataract extraction and pseudophakic intraocular lens implantation. J Cataract Refract Surg. 2006;32:595–598.
- Li S, Chen X, Kang Y, et al. Femtosecond laser-assisted cataract surgery in a cataractous eye with implantable collamer lens in situ. J Refract Surg. 2016;32:270–272.
- Lee H, Kang DS, Ha BJ, et al. Effect of accommodation on vaulting and movement of posterior chamber phakic lenses in eyes with implantable collamer lenses. Am J Ophthalmol. 2015;160:710–716 e711.
- Choi JH, Lim DH, Nam SW, et al. Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J Cataract Refract Surg. 2019;45:1555–1561.
- Olsen T, Olesen H, Thim K, et al. Prediction of postoperative intraocular lens chamber depth. J Cataract Refract Surg. 1990;16:587–590.
- Goto S, Maeda N, Koh S, et al. Prediction of postoperative intraocular lens position with angle-to-angle depth using anterior segment optical coherence tomography. Ophthalmology. 2016;123:2474–2480.
- Tamaoki A, Kojima T, Tanaka Y, et al. Prediction of effective lens position using multiobjective evolutionary algorithm. Transl Vis Sci Technol. 2019;8:64.
- Qi MY, Chen Q, Zeng QY. The effect of the crystalline lens on central vault after implantable collamer lens implantation. J Refract Surg. 2017;33:519–523.
- Zhang X, Chen X, Wang X, et al. Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol. 2018;18:114.