ABSTRACT
Clinical relevance
The peripheral refraction profile in myopes with different corrective modalities varies significantly for both distance and near viewing and will have implications in managing myopia.
Background
This study investigated how the magnitude of peripheral myopic defocus induced by Ortho-K varies with and without accommodation, and how this compares to single vision spectacles and soft-contact-lenses (SCL).
Methods
Relative peripheral refraction (RPR) of 18 young adults (spherical equivalent −1.00 D to −4.50 D) was determined along the horizontal meridian (±10°, ±20°, ±25°) during distance (3-metres) and near viewing (0.2-metres), and along vertical meridian (±10°, ±15°) for distance viewing alone. Measurements were obtained in an uncorrected state and with single vision spectacles, soft contact lens and Ortho-K. Changes in RPR and astigmatic components were compared between distance and near viewing with all different modalities.
Results
A significant interaction (p = 0.02) between relative peripheral refraction and the target distance (distance and near viewing) was found among different refractive modalities. Single overnight Ortho-K lens wear alone led to relative peripheral myopia for both distance (mean RPR ± SE: −0.92 ± 0.21D and −1.04 ± 0.22D) and near viewing (−0.71 ± 0.17D and −0.76 ± 0.20D). Comparisons of relative peripheral refraction between different corrective modalities at each eccentricity indicated statistical significance of RPR at extreme locations along both temporal and nasal meridian (±20 and ±25°, p < 0.05). RPR with soft contact lenses and spectacles were similar for both distance and near viewing (p > 0.05).
Conclusion
Single overnight Ortho-K lens wear alone shifted the RPR in the myopic direction for both distance and near viewing in comparison with single vision spectacles and soft contact lenses. The Ortho-K lens designs that offer a large amount of mid-peripheral corneal steeping, in-turn leading to high relative peripheral myopia for both distance and near viewing and might offer beneficial effects on myopia control.
Introduction
The debate over the onset and progression of myopia has been encapsulated by the complex interaction of genetic and environmental factors.Citation1,Citation2 Among various hypotheses that were proposed as possible causes of myopia, hypotheses relating to mechanical tension theory,Citation3,Citation4 peripheral defocus theory,Citation5–7 and lag of accommodation theoryCitation3,Citation8–11 are widely investigated.Citation12,Citation13
While DonderCitation14 and HelmholtzCitation15 considered myopia to be an acquired condition associated with stress at the equator of the eye due to excessive near work, various studies have proposed that greater lag of accommodation during near viewing in myopic children, that is, central hyperopic defocus compared to that of emmetropes, could be a stimulant for ocular growth.Citation8,Citation16–18 Experiments conducted on animal models indicated that the elimination of foveal signals did not interfere with emmetropization and lens-induced hyperopic defocus on the peripheral retina promoted ocular growth causing axial myopia.Citation19,Citation20 In humans, multiple research studies have reported relative peripheral hyperopia and prolate retinal contour in myopes compared to emmetropes and hyperopes.Citation21–24 Although the role of peripheral hyperopic defocus is considered as an important factor associated with myopia progression, the influence of accommodation on peripheral refraction is not clear. While Walker and Mutti found relative peripheral refraction to become more hyperopic with accommodation in myopic participants compared to emmetropic participants,Citation25 Calver et al. indicated no impact of accommodation in the peripheral retina and reported similar peripheral refraction patterns in both emmetropes and myopes.Citation24
Whilst the use of conventional single vision spectacle lenses for the correction of central myopic refractive error results in relative peripheral hyperopic defocusCitation26,Citation27 several corrective modalities that induce relative peripheral myopia (in both spectacle and contact lens form) have been used recently for controlling myopia progression.Citation28–34 Although previous studies have shown that orthokeratology (Ortho-K) lens wear typically induces relative peripheral myopia for distance viewing and it can be expected that peripheral myopic pattern could remain the same with accommodation, it is not clear if the magnitude of myopic defocus with Ortho-K remains the same with and without accommodation, and how it varies in comparison with single vision spectacles and soft contact lenses.Citation35–37
Assuming the importance of having relative peripheral myopic defocus in myopia irrespective of distance or near viewing, this study aimed to investigate and improve understanding of peripheral refraction profile in myopes during distance and near viewing with different optical correction modalities (spectacles, soft contact lenses and single overnight Ortho-K lens wear).
Methods
A total of 20 healthy young adult myopes (spherical equivalent range −1.00D to −4.50 D with astigmatism not exceeding −0.50 D) without any ocular or systemic conditions that could influence the refractive error were recruited for the study. All participants had a best-corrected visual acuity of 0.00 logMAR or better in both eyes with high contrast logMAR chart under normal room illumination (130–140 lux, measured using lux-metre), and no participants had any monocular or binocular vision anomalies that could affect the experimental outcomes. The study was approved by the institutional review board of the L V Prasad Eye Institute, India (LEC 05-18-095), and adhered to the tenets of the declaration of Helsinki. Before commencing any measurements, appropriate written and informed consent was obtained from all participants after explaining the nature and consequences of the study.
Examination protocol
The protocol for the experiment required participants to visit the myopia research lab for two consecutive days. At the baseline visit, all participants underwent a comprehensive eye examination with particular attention to the lid and corneal health to check for their suitability for participation in the study. The following techniques were conducted: i) corneal topography was determined using an Oculyzer IICitation38 (WaveLight®, Alcon, Fort Worth, TX, USA), ii) Central and peripheral refraction using open-field Shin-Nippon autorefractorCitation39,Citation40 (Nvision-K 5001, Japan) at two fixation distances (distance and near), and iii) on-axis ocular biometry and pupil size were measured under normal room illumination using LenstarCitation41 (LS 900, Haag-Streit, Switzerland). Refraction was recorded in the uncorrected state, with spectacles, and with soft contact lenses (details of spectacles and contact lens described below). On the same day after the baseline measurements, participants were fitted with the Ortho-k lens and asked to sleep with the lenses for at least 8 hours that night. On the second visit, participants were instructed to revisit the clinic without removing their Ortho-K lenses from the eyes. The corneal topography, ocular biometry, and peripheral refraction measurements (for both distance and near viewing) were performed immediately after the lens removal following a similar protocol of baseline visit. All measurements were completed in less than 30 minutes. With each instrument, five measurements were recorded, and the averaged measurements were used for analysis.
Central and peripheral refraction
Central and peripheral refraction were measured in the uncorrected state first and then the measurements were repeated with habitual correction in place, that is, spherical equivalent refraction inserted in a full aperture trial frame with a lens diameter of 22 mm and maintaining a vertex distance of 12 mm. Spherical equivalent was chosen instead of inserting cylindrical lenses to avoid reflection from multiple lens surfaces (note that none of the participants had central astigmatism > 0.5 D and the effect of using spherical equivalent should be minimal on the outcomes as the major comparisons are for refraction with and without accommodation).
Soft contact lens trial
The soft contact lens trial was performed for all the participants with 1-Day Acuvue Moist (etafilcon A) daily disposable contact lenses (Johnson & Johnson Private Ltd.). All participants were fitted with a soft contact lens of appropriate power in both eyes after compensating for vertex distance. The contact lenses are commercially available in a universal diameter of 14.2 mm and two different base curvatures: 8.5 and 9.0 mm. During the lens trial, the average keratometry value from the topography map was used to identify the closest match for the available base curve of the contact lens. An adaptation period of 30 minutes was allotted for the lens to settle down on the ocular surface before the assessment of contact lens fitting. Standard parameters such as the lens coverage, centration, movement and lag from the primary and up-gaze position were noted to certify the acceptability of the lens fit, following which both central and peripheral refraction measurements were recorded.
Ortho-K trial
The Ortho-K lens trial was conducted using Paragon CRT® (paflufucon B) contact lenses (Paragon Vision Sciences, USA). The lenses are typically available for a uniform diameter of 10.50 mm and are designed to reshape corneal curvatures ranging from 39 D to 50 D. The three unique components of the lens: a central 6.0 mm fixed optic zone that serves as the treatment zone, a surrounding 1.0 mm annular region that defines the return zone depth (varies in 25-micron steps), and third, a landing zone angle (varies in 1-degree steps) that define the relationship of lens periphery with the corneal limbus are fundamental in the functioning of these lenses. The determination of the trial, the decision of a conclusive final contact lens for dispensing, and the assessment of the lens fitting characteristics were according to standard established guidelines from the literature.Citation42 Emphasis was given on the centration of the optic zone over the pupillary area and the correction factor achieved with the contact lenses. An over-refraction ranging from plano to +1.00 D, a central island of the flattened corneal surface (at least 6.0 mm in diameter) surrounded by an annular zone of relatively steeper curvature (at least 1.0 mm in diameter) after lens removal was considered appropriate. The lens dynamics (lens movement and stability over the corneal surface) understanding of the lens–cornea relationship with the help of fluorescein as well as the ideal lens fitting characteristics were considered similar to those reported by Gonzalez and colleagues.Citation43 Once the Ortho-K lens fit was deemed satisfactory, the participants were dispensed with the lenses for both eyes and the second visit was scheduled on the immediate next day, after a minimum overnight 8 hours of lens wear. The necessary care and maintenance regimen of the contact lens was explained in detail to all the participants recruited in the study. No under or over correction was prescribed during the measurement with any of the corrective modalities (spectacles or soft contact lenses). In participants with best-corrected visual acuity of 6/6 in both eyes, only the right eye was considered for analysis. However, in the case of participants with asymmetrical best-corrected visual acuity with overnight wear of Ortho-K, the eye with better VA, that is, at least 6/6 for distance and N6 for near was chosen for analysis. Based on these criteria, we had data from the right eye for 12 participants and the left eye for six participants for analysis. Although 15% of the Ortho-K lens participants had a residual refractive error after overnight lens wear, their uncorrected visual acuity was 6/6 at 6 m and N6 at 33 cm. We excluded two participants who had decentred Ortho-K lens fitting during the evaluation leading to the availability of 18 participants for data analysis.
Peripheral refraction
Peripheral refraction was determined at six eccentricities along the horizontal meridian (±10°, ±20°, ±25°) and four eccentricities along vertical meridian (±10°, ±15°) with the participants making an eye turn to fixate the targets (with the head fixed in the head-chin rest of the auto-refractor). To ensure the accuracy of measurements, the axis of the auto-refractor (graticule) was aligned with the geographic centre of the pupil during all the measurements at all eccentricities by using the inbuilt video monitor screen of the auto-refractor.Citation44 An inbuilt software was used to automatically transfer data from auto-refractometer to computer (in Microsoft Excel format) to avoid errors in data entry. During distance viewing, participants fixated monocularly with the eye for which measurements are recorded (the non-tested fellow eye was patched during the measurement). The Maltese cross targets (luminance: 0.02-0.03 cd/m2; 85% Michelson contrast, size – 6 cm x 6 cm crosses) that are placed on a flat surface (wall) that is 3 m away from the eye. During near viewing, participants viewed the high contrast Bull’s eye pattern target binocularly (20 cm from the eye) and was kept at desired visual field angles by using a rotating protractor fixed on top of the open-field Shin-Nippon auto-refractor. The size of the near target was 3 × 3 cm with a luminance of 0.02–0.03 cd/m2 and 85% Michelson contrast and was equivalent to a letter size that corresponds to the Snellen visual acuity of 6/9 (20/30). Five measurements of refraction were recorded at each eccentricity, and data collection for all participants was conducted between 7:00 am and 10:00 am. Non-cycloplegic peripheral refraction was conducted to preserve accommodation for the near vision measurement. Conventional sphero cylindrical refractive error (S/C x Ө) measured by the auto-refractor was converted into power vectors M, J0, and J45 to allow for statistical analysis, using the equations derived by Thibos.Citation45 Relative peripheral refraction was determined by subtracting central refraction from refractions obtained at different retinal eccentricities (relative peripheral refraction = peripheral M—central M). The lag of accommodation was calculated as the difference between the accommodative demand and the accommodative response. Relative peripheral refraction, J0, and J45 were plotted as a function of visual field positions and were taken as being positive for both nasal and superior visual fields. Absolute peripheral refraction refers to the value given by the instrument at each eccentric location without subtracting the central refraction value.
Statistical analysis
The statistical analyses were performed using IBM SPSS software version 23.0.0 (SPSS, Inc, Chicago, IL), and graphs were plotted using the inbuilt feature of MS-Excel (Microsoft Office Version 2016). Shapiro-Wilk test indicated the normal distribution of the data and thus parametric tests were applied for analyses. Repeated measures ANOVA was conducted for relative peripheral refraction, J0, and J45 separately, with each treatment modality and visual field meridian (horizontal/vertical) as within-subject factors. Post-hoc t-tests with Bonferroni correction were used to compare results between different corrective modalities. To investigate if the peripheral refraction profile was affected by the treatment modality and the changing viewing distance interaction term was calculated using ANOVA.
Results
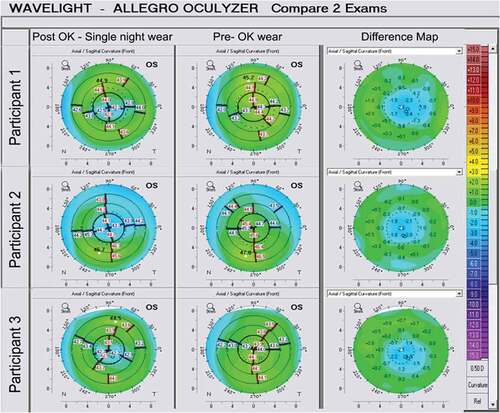
The mean age ± SD of the 18 participants was 22 ± 3 years (range: 20 to 26 years). The mean central spherical equivalent refractive error and on-axis axial length were −2.60 D ± 0.85 D and 24.28 ± 0.82 mm, respectively. The average pupil size of the study participants was 4.94 ± 0.89 mm (range: 3.97 to 6.13 mm). There was no significant difference (p = 0.061) in mean foveal refractive error among all different corrective modalities [spectacles (−0.12 ± 0.41), soft contact lenses (−0.13 ± 0.30), and Ortho-K (−0.38 ± 0.34 D)]. The magnitude of accommodative lag with spectacles (+1.23 D ± 0.14 D), soft contact lenses (+1.09 D ± 0.14 D), and Ortho-K (+1.38 ± 0.20 D) was similar (p = 0.27). A typical topography difference map with pre- and post-single overnight Ortho-K wear of three individual participants is described in . In the present study, participants exhibited a residual refractive error of less than −0.75D after overnight Ortho-K lens wear with 51% of them showing the residual error of only −0.25 D.
Figure 1. Topography difference map for a participant pre and post overnight Ortho-K lens wear. The panel on the extreme left side is for post overnight Ortho-K lens wear and the panel on the extreme right indicates differences in corneal curvature and thickness pre and post Ortho-K wear.
Mean absolute peripheral refraction measured during distance and near viewing with different corrective modalities and in the uncorrected state are shown in ; the statistical significance of corresponding values based on eccentricity and viewing distance is given in . The mean absolute peripheral refraction at 25° temporal and 25° nasal eccentricities with single overnight Ortho-k lens was −1.78 ± 0.22 D and −1.68 ± 0.28 D for distance viewing, and −2.38 ± 0.20 D and −2.33 ± 0.18 D for near viewing. While soft contact lenses led to a small amount of absolute peripheral myopia at 25° nasal and 25° temporal eccentricities (−0.08 ± 0.12 and −0.31 ± 0.11D) for distance viewing, the spectacles did not alter peripheral refraction in nasal and temporal eccentricities during distance and near viewing.
Table 1. The mean relative peripheral refraction (± SE) with corrective modalities across different eccentricities. The F and P values are derived from repeated measures of ANOVA. * mark indicates significant difference in pairwise comparison of distance and near peripheral refraction within each modality.
Figure 2. Mean absolute peripheral refraction across different eccentricities for distance and near viewing with spectacle, soft contact lenses, Ortho-K lens wear, and in the uncorrected state. Error bars indicate standard error of mean.
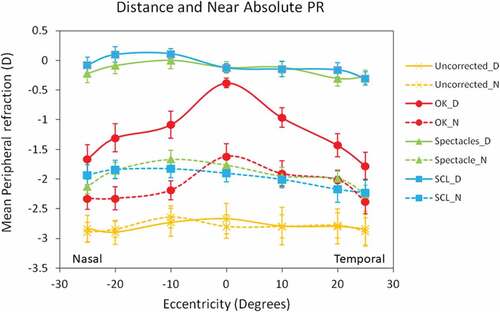
Repeated measures ANOVA indicated the influence of corrective modality on relative peripheral refraction (combined across all eccentricities) for both the distance (p = 0.001) and near (p = 0.03) viewing. Comparisons of relative peripheral refraction between different corrective modalities at each eccentricity indicated statistical significance of relative peripheral refraction at extreme locations along both temporal and nasal meridian (±20 and ±25 degrees, p < 0.05). On comparing the relative peripheral refraction at different eccentricities within each corrective modality, a significant influence of eccentric location on the relative peripheral refraction profile was observed with overnight wear of Ortho-K lenses (for both distance and near viewing) and soft contact lenses (only for distance viewing). Single overnight wear of Ortho-K lenses led to greater relative peripheral myopia compared to uncorrected state and other corrective modalities in both the viewing distances (). The relative peripheral refraction values with Ortho-K at the nasal 25° and temporal 25° were −0.92 ± 0.20 D and −1.04 ± 0.21 D, respectively; corresponding values for the near viewing were −0.71 ± 0.17 D and −0.76 ± 0.20 D, respectively. There was no significant naso-temporal asymmetry in relative peripheral refraction at extreme eccentricities obtained during distance (p = 0.35) and near viewing (p = 0.40) with Ortho-K lens. Relative peripheral refraction with the soft contact lenses and spectacles were similar across all eccentricities for both distance (p = 0.67) and near viewing (p = 0.73). While the relative peripheral refraction values with the soft contact lenses were numerically small, they were statistically significant for distance viewing (nasal 25°: +0.05 ± 0.13 D vs. temporal 25°: −0.18 ± 0.11 D, p = 0.04).
A significant interaction (p = 0.02) was noted between relative peripheral refraction and the target distance (distance and near viewing). On comparing the relative peripheral refraction at each eccentricity between distance and near viewing, the relative peripheral myopia with single overnight wear of Ortho-K lenses during near viewing was found less along temporal and nasal than that of distance viewing (−0.38D along temporal and −0.16 D along nasal) (p < 0.001 for both). Other modalities did not show such significance. The target distance did not alter peripheral refraction in both soft contact lenses and spectacles.
Relative peripheral J0 component measured during distance viewing showed more negative values in the periphery along the horizontal meridian with all the treatment modalities () (F5,Ortho-K = 8.88, p = 0.001; F5,soft-contact lens = 3.22, p = 0.01; and F5,spectacles = 3.05, p = 0.002). Ortho-K lens alone showed a significant increase in negative values with eccentricities for near viewing (F5,Ortho-K = 3.02, p = 0.01; F5,soft-contact lens = 0.52, p = 0.75; F5,spectacles = 0.51, p = 0.76). The J45 component did not change significantly with eccentricity for both distance and near viewing along the horizontal meridian with all corrective modalities (corresponding ANOVAs: P > 0.05) ().
Figure 3. Mean variation in power vector J0 component across different eccentricities for distance (panel A: and near (panelB: viewing with spectacles, soft contact lenses, Ortho-K lens wear, and in the uncorrected state. Error bars indicate standard error.
Figure 4. Mean variation in power vector J45 component across different eccentricities for distance (panel A: and near (panelB: viewing with spectacles, soft contact lenses, Ortho-K lens wear, and in the uncorrected state. Error bars indicate standard error.
Along the vertical meridian (), although Ortho-k lead to greater relative peripheral myopia at extreme eccentricity, there was no statistical significance noted on relative peripheral refraction with any of corrective modality (F3,Ortho-K = 2.55, p = 0.06, F3,soft-contact lens = 2.12, p = 0.10, and F3,spectacles = 2.05, p = 0.11).
Discussion
This study found variation in peripheral refraction profiles (for distance and near viewing) among three different corrective modalities (spectacles, soft contact lenses and single overnight Ortho-K lens wear), and the uncorrected state in a sample of myopic participants. Corneal reshaping with single overnight Ortho-K lens wear led to significant relative peripheral myopia (M values) for both distance and near viewing in comparison with uncorrected, spectacles and soft contact lenses. Change in J0 (astigmatism component) mirrored that of the M component at all eccentricities in all the corrective modalities whilst J45 (oblique component) did not change in either of the corrective modalities.
Although there is extensive literature on peripheral refraction and its association with myopia,Citation22,Citation46,Citation47 there is limited information about how peripheral refraction varies during distance and near viewing with different optical modalities.Citation16,Citation24,Citation25,Citation61 Previous studies have either investigated changes in relative peripheral refraction with a single corrective modality (Ortho-K, single vision spectacles, and multifocal spectacles and contact lenses) for distance viewing alone,Citation26,Citation48–51 or with spectacles or soft contact lenses separately for both distance and near viewing.Citation16,Citation24,Citation25 To the best of our knowledge, this is the first study to report the effect of different corrective modalities (spectacles, soft contact lenses, and single overnight Ortho-K lens wear) on the peripheral refraction profile for distance and near viewing in the same individuals.
compares the results obtained from the current study with mean relative peripheral refraction changes using different optical corrective modalities reported in previous studies. During distance viewing, the relative peripheral refraction values with spectacle followed the pattern that was obtained without any correction and agrees with that of the previous studies.Citation24,Citation26,Citation27 Earlier studies have reported naso-temporal asymmetry in the relative peripheral refraction profile using soft contact lenses with temporal retina receiving greater myopic defocus than nasal retina, which agrees with the findings of the present study (−0.18 D at 25° temporal and +0.05 D at 25° nasal eccentricity with soft contact lenses).Citation52–54 Some amount of decentration of the soft contact lenses remains a possible explanation for the asymmetry seen in the peripheral refractive profile. The relative peripheral myopia with single overnight Ortho-K wear corroborates with the findings of previous studies that have investigated relative peripheral refraction changes with the Ortho-K lens.Citation37,Citation48,Citation55–58 The present study shows a similar amount of relative peripheral myopia at 25° eccentricity for distance viewing with single overnight Ortho-K lens along with the temporal (−1.04 ± 0.21 D) and nasal meridian (−0.92 ± 0.20 D) compared to that of the previous study at 30 degrees nasal and temporal eccentricity.Citation48,Citation56 We found no significant differences in relative peripheral refraction at the extreme eccentricities of the nasal and temporal meridian after a single night of Ortho-K lens wear (p = 0.38), which differs from the results reported by Kang and Swarbrick,Citation57 and Queiros et al.Citation37 who indicated an asymmetric pattern of peripheral refraction, with the temporal retina being more myopic than the nasal retina after correction with Ortho-K lenses. This discrepancy related to the pattern of the relative peripheral refraction profile along the horizontal meridian between our findings and that of previous studies could be attributed to the possible effects of lens decentration found in previous studies. Both Kang and Swarbrick,Citation57 and Queiros et al.Citation37 included participants with decentration, whereas in the current study, we included participants without decentration. In addition, the differences could also be attributed to the fact that the duration of lens wear is different among the studies (the current study assessed peripheral refraction with only a single night of lens wear).
Table 2. Mean relative peripheral refraction investigated across different eccentricities for distance and near viewing with different corrective modalities in 13 previously published studies compared with the results of the current study in myopes. Abbreviations: PALs-progressive addition lenses, SCL-soft contact lenses and RGP-rigid gas permeable lenses.
In the present study, the lag of accommodation at 20 cm was similar among all corrective modalities (p > 0.05), and the magnitude of accommodative lag was similar to the previously reported lag among myopes.Citation24,Citation52,Citation59–61 We found no significant differences in the peripheral refraction pattern with spectacles when changing the fixation point from distance to near which agrees with the findings of Calver et al.Citation24 The finding of myopic defocus with soft contact lenses across all eccentricities except 10° and 20° nasal locations during near viewing corroborate with the results reported by Whatman et al.Citation16 who found a myopic shift in relative peripheral refraction with increasing levels of accommodationCitation16 after correcting myopes with a soft contact lens. Although the amount of peripheral myopic defocus during near viewing with a single overnight of Ortho-K wear was slightly less compared to that of distance viewing, it is still greater than the values obtained with other corrective modalities. Bersten et.al.Citation52 reported hyperopic defocus with a soft contact lens for near viewing at all eccentricities except at the 40° temporal location, whereas in the present study, myopic defocus was found with soft contact lenses across all eccentricities except 10° and 20° nasal locations for near viewing.
Overall, a single overnight of Ortho-K lens wear has shown greater relative peripheral myopia for both distance and near viewing compared to soft contact lenses and spectacles across all eccentricities. The mean relative peripheral refraction across all eccentricities was emmetropic for distance viewing with the soft contact lenses, but there was relative peripheral myopia at the extreme temporal retinal location (20° eccentricity: −0.03 ± 0.12 D and 25° eccentricity: −0.18 ± 0.11 D). Spectacles had the least myopic defocus for distance and near in comparison with soft contact lenses and Ortho-K lenses. In contrast to the findings of the present study, Backhouse et al.Citation27 reported that correction with spectacle lenses resulted in hyperopic defocus (+1.01 ± 0.13 D) in the peripheral retina, whereas the same eyes experienced significant myopic defocus (−1.84 ± 0.61 D) in the peripheral retina when corrected with soft contact lenses. In the current study, we found that during distance viewing, Ortho-K lens leads to significant myopic defocus throughout the periphery of the retina, whereas soft contact lenses lead to hyperopic defocus in all zones except the extreme temporal eccentricity which is in agreement with a study conducted by Tarutta et al.Citation62 which evaluated the influence of soft contact lenses and Ortho-k on peripheral refraction during distance viewing. Both relative peripheral refraction and J0 across both meridians for both distance and near viewing with Ortho-K lens show significant negative values compared to other corrections, which could be a possible reason for why Ortho-K lenses tend to give better implications for myopia control as compared to other treatment strategies.Citation31,Citation34,Citation63,Citation64
The relative peripheral J0 component of astigmatism showed negative relative peripheral refraction during distance viewing across all eccentricities with correction (spectacles, soft contact lenses, and Ortho-K lens) as compared to without correction and is consistent with findings of previous literature.Citation26,Citation37,Citation48,Citation49 For near viewing, the J0 component at different eccentricity was not influenced by spectacles and soft contact lenses, but the Ortho-K lens resulted in significant negative J0 relative peripheral refraction with active accommodation.
Along the vertical meridian, there was no statistical significance difference noted on relative peripheral refraction with any of the corrective modality and the uncorrected state is in concordance with published literature.Citation26,Citation37,Citation48,Citation49 None of the previous studies have investigated peripheral refraction along the vertical meridian with Ortho-K.
From the peripheral retina theory for myopiogenesis, it is understood that relative peripheral hyperopic defocus could trigger myopia development, and thus a lot of anti-myopia strategies have been developed to counteract this triggering hyperopic defocus.Citation65–67 Previous studiesCitation16,Citation24,Citation25 that investigated the relationship between peripheral defocus at distance and near viewing have conflicting results and it is not clear if the relative peripheral myopia needs to be maintained during both distance (relaxed accommodation) and near viewing (active accommodation). While the findings from the current study, that is, Ortho-K lens due to its reverse geometry lead to relative peripheral myopic refraction (1.25 D during distance viewing and 0.75 D during near viewing), it shows greater relative peripheral myopia compared to regular single vision strategies and, in turn, could show better efficacy in myopia control.
If the peripheral defocuses should be myopic all the time, then the anti-myopia strategies through either mid-peripheral steepening or addition of plus power in lens format need to consider lag of accommodation in myopes (range: +0.75 D to +1.25 D) and induce appropriate peripheral myopic defocus during near viewing.Citation8,Citation10 We measured peripheral refraction only till ±25°and it is possible that peripheral refraction beyond the ±25° could have shown more relative myopic peripheral refraction for both distance and near viewing (absolute myopia). Previous studies that investigated peripheral refraction with Orth-K during distance viewing reported peripheral refraction values to range from 0.5 D to 3 D.Citation37,Citation48,Citation55–57 Studies conducted to evaluate the effect of multifocal contact lens on peripheral refraction have indicated that central distance lens design with higher peripheral add power results in more myopic defocus and better efficacy in myopia control compared to lower add.Citation51,Citation52,Citation67,Citation68 Longitudinal studies are awaited in this zone to investigate the potential need for absolute myopic defocus in peripheral retinal locations during both distance and near viewing for myopia control. Given that myopes tend to show greater accommodative lag, the orthokeratology lens designs that lead to a greater amount of myopic defocus due to mid-peripheral steeping may work in favour to counteract the increased lag of accommodation during near viewing.
The primary strength of the present study was that the study protocol allowed obtaining measurements of peripheral refraction for both distance and near viewing in the same individuals following the use of spectacles, soft contact lenses and Ortho-K lens. The result here agrees with previous research about changes in relative peripheral refraction using different optical strategies for distance viewing and provides additional information on changes in relative peripheral refraction in the horizontal visual field for near viewing too. The peripheral refraction for all three corrective modalities was measured at the same time of the day, minimising the possible errors due to diurnal variation in various ocular structures. There are certain limitations to this study. Firstly, only spherical lenses were used. Spherical lenses were used for simplicity to avoid reflection from multiple lens surfaces. None of the participants had central astigmatism > 0.5 D and the effect of using spherical equivalent should be minimal on the outcomes. Secondly, changes in peripheral refraction were recorded after one night of Ortho-K lens wear only, meaning that change to relative peripheral refraction is likely to be less than reported in previous studies measured after longer periods of overnight Ortho-K wear. Thirdly, we did not examine peripheral refraction with centre distance design multifocal soft contact lenses. Comparison of relative peripheral refraction changes between Ortho-K and multifocal lenses (in addition to single vision spectacles and soft contact lenses) would have added additional critical information to the field of peripheral optics and anti-myopia strategies.
In conclusion, compared to both spectacles and soft contact lenses, a single overnight of Ortho-K lens wear shifted the relative peripheral refraction in the myopic direction for both distance and near viewing due to the presence of mid-peripheral corneal steeping. The Ortho-K lens designs that offer a greater amount of mid-peripheral corneal steeping, in turn leading to greater relative peripheral myopia for both distance and near viewing might offer beneficial effects on myopia control.
Acknowledgements
The authors gratefully acknowledge the Hyderabad Eye Research Foundation for support in conducting this study. We are indebted to Mr. Shashank Bhandary for his assistance with data collection and Mr. Swapnil Thakur for providing critical feedback on the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32:3–16.
- O’Donoghue L, Kapetanankis VV, McClelland JF, et al. Risk factors for childhood myopia: findings from the NICER study. Invest Ophthalmol Vis Sci. 2015;56:1524–1530.
- Berntsen DA, Mutti DO, Zadnik K. Study of Theories about Myopia Progression (STAMP) design and baseline data. Optom Vis Sci. 2010;87:823–832.
- Smith EL 3rd, Hung LF, Huang J, et al. Effects of optical defocus on refractive development in monkeys: evidence for local, regionally selective mechanisms. Invest Ophthalmol Vis Sci. 2010;51:3864–3873.
- Mutti DO, Sholtz RI, Friedman NE, et al. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000;41:1022–1030.
- Logan NS, Gilmartin B, Wildsoet CF, et al. Posterior retinal contour in adult human anisomyopia. Invest Ophthalmol Vis Sci. 2004;45:2152–2162.
- Smith EL 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–2392.
- Gwiazda JE, Hyman L, Norton TT, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45:2143–2151.
- Weizhong L, Zhikuan Y, Wen L, et al. A longitudinal study on the relationship between myopia development and near accommodation lag in myopic children. Ophthalmic Physiol Opt. 2008;28:57–61.
- Mutti DO, Mitchell GL, Hayes JR, et al. Accommodative lag before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2006;47:837–846.
- Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82:273–278.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622–660.
- Saw SM. A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom. 2003;86:289–294.
- Donders FC, Moore WD. On the anomalies of accommodation and refraction of the eye: with a preliminary essay on physiological dioptrics. Br Foreign Med Chir Rev. 1864;34(68):443–445.
- von Helmholtz H. Treatise on physiological optics. Hamburg (Germany): Verlag; 1962. von Leopold Voss; 1909. Translated by Southhall JPC. In: New York: Dover Publications.
- Whatham A, Zimmermann F, Martinez A, et al. Influence of accommodation on off-axis refractive errors in myopic eyes. J Vis. 2009;9:11–13.
- Davies LN, Mallen EA. Influence of accommodation and refractive status on the peripheral refractive profile. Br J Ophthalmol. 2009;93:1186–1190.
- Lundstrom L, Mira-Agudelo A, Artal P. Peripheral optical errors and their change with accommodation differ between emmetropic and myopic eyes. J Vis. 2009;9:11.
- Smith EL 3rd, Kee CS, Ramamirtham R, et al. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–3972.
- Huang J, Hung LF, Smith EL 3rd. Recovery of peripheral refractive errors and ocular shape in rhesus monkeys (Macaca mulatta) with experimentally induced myopia. Vision Res. 2012;73:30–39.
- Seidemann A, Schaeffel F, Guirao A, et al. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am A Opt Image Sci Vis. 2002;19:2363–2373.
- Verkicharla PK, Mathur A, Mallen EA, et al. Eye shape and retinal shape, and their relation to peripheral refraction. Ophthalmic Physiol Opt. 2012;32:184–199.
- Verkicharla PK, Suheimat M, Schmid KL, et al. Peripheral refraction, peripheral eye length, and retinal shape in myopia. Optom Vis Sci. 2016;93:1072–1078.
- Calver R, Radhakrishnan H, Osuobeni E, et al. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol Opt. 2007;27:584–593.
- Walker TW, Mutti DO. The effect of accommodation on ocular shape. Optom Vis Sci. 2002;79:424–430.
- Lin Z, Martinez A, Chen X, et al. Peripheral defocus with single-vision spectacle lenses in myopic children. Optom Vis Sci. 2010;87:4–9.
- Backhouse S, Fox S, Ibrahim B, et al. Peripheral refraction in myopia corrected with spectacles versus contact lenses. Ophthalmic Physiol Opt. 2012;32:294–303.
- Bakaraju RC, Ehrmann K, Ho A, et al. Pantoscopic tilt in spectacle-corrected myopia and its effect on peripheral refraction. Ophthalmic Physiol Opt. 2008;28:538–549.
- Tabernero J, Vazquez D, Seidemann A, et al. Effects of myopic spectacle correction and radial refractive gradient spectacles on peripheral refraction. Vision Res. 2009;49:2176–2186.
- Mutti DO, Sinnott LT, Reuter KS, et al. Peripheral refraction and eye lengths in myopic children in the Bifocal Lenses In Nearsighted Kids (BLINK) study. Transl Vis Sci Technol. 2019;8:17.
- Walline JJ. Myopia control: a review. Eye Contact Lens. 2016;42:3–8.
- Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181–1185.
- Downie LE, Lowe R. Corneal reshaping influences myopic prescription stability (CRIMPS): an analysis of the effect of orthokeratology on childhood myopic refractive stability. Eye Contact Lens. 2013;39:303–310.
- Li X, Friedman IB, Medow NB, et al. Update on orthokeratology in managing progressive myopia in children: efficacy, mechanisms, and concerns. J Pediatr Ophthalmol Strabismus. 2017;54:142–148.
- Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913–3919.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5065.
- Queiros A, Gonzalez-Meijome JM, Jorge J, et al. Peripheral refraction in myopic patients after orthokeratology. Optom Vis Sci. 2010;87:323–329.
- Bao F, Savini G, Shu B, et al. Repeatability, reproducibility, and agreement of two scheimpflug-placido anterior corneal analyzers for posterior corneal surface measurement. J Refract Surg. 2017;33:524–530.
- Davies LN, Mallen EA, Wolffsohn JS, et al. Clinical evaluation of the Shin-Nippon NVision-K 5001/Grand Seiko WR-5100K autorefractor. Optom Vis Sci. 2003;80:320–324.
- Cleary G, Spalton DJ, Patel PM, et al. Diagnostic accuracy and variability of autorefraction by the tracey visual function analyzer and the Shin-Nippon NVision-K 5001 in relation to subjective refraction. Ophthalmic Physiol Opt. 2009;29:173–181.
- Shammas HJ, Hoffer KJ. Repeatability and reproducibility of biometry and keratometry measurements using a noncontact optical low-coherence reflectometer and keratometer. Am J Ophthalmol. 2012;153:e52.
- Rah MJ, Jackson JM, Jones LA, et al. Overnight orthokeratology: preliminary results of the Lenses and Overnight Orthokeratology (LOOK) study. Optom Vis Sci. 2002;79:598–605.
- Gonzalez-Meijome JM, Villa-Collar C. Nomogram, corneal topography, and final prescription relations for corneal refractive therapy. Optom Vis Sci. 2007;84:59–64.
- Ehsaei A, Chisholm CM, Mallen EA, et al. The effect of instrument alignment on peripheral refraction measurements by automated optometer. Ophthalmic Physiol Opt. 2011;31:413–420.
- Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–375.
- Charman WN, Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt. 2010;30:321–338.
- Rotolo M, Montani G, Martin R. Myopia onset and role of peripheral refraction. Clin Optom. 2017;9:105–111.
- Charman WN, Mountford J, Atchison DA, et al. Peripheral refraction in orthokeratology patients. Optom Vis Sci. 2006;83:641–648.
- Shen J, Clark CA, Soni PS, et al. Peripheral refraction with and without contact lens correction. Optom Vis Sci. 2010;87:642–655.
- Berntsen DA, Barr CD, Mutti DO, et al. Peripheral defocus and myopia progression in myopic children randomly assigned to wear single vision and progressive addition lenses. Invest Ophthalmol Vis Sci. 2013;54:5761–5770.
- Kang P, Fan Y, Oh K, et al. The effect of multifocal soft contact lenses on peripheral refraction. Optom Vis Sci. 2013;90:658–666.
- Berntsen DA, Kramer CE. Peripheral defocus with spherical and multifocal soft contact lenses. Optom Vis Sci. 2013;90:1215–1224.
- Kang P, Fan Y, Oh K, et al. Effect of single vision soft contact lenses on peripheral refraction. Optom Vis Sci. 2012;89:1014–1021.
- Moore KE, Benoit JS, Berntsen DA. Spherical soft contact lens designs and peripheral defocus in myopic eyes. Optom Vis Sci. 2017;94:370–379.
- Gifford KL, Gifford P, Hendicott PL, et al. Stability of peripheral refraction changes in orthokeratology for myopia. Cont Lens Anterior Eye. 2020;43:44–53.
- Gonzalez-Meijome JM, Faria-Ribeiro MA, Lopes-Ferreira DP, et al. Changes in peripheral refractive profile after orthokeratology for different degrees of myopia. Curr Eye Res. 2016;41:199–207.
- Kang P, Swarbrick H. Peripheral refraction in myopic children wearing orthokeratology and gas-permeable lenses. Optom Vis Sci. 2011;88:476–482.
- Kang P, Gifford P, Swarbrick H. Can manipulation of orthokeratology lens parameters modify peripheral refraction? Optom Vis Sci. 2013;90:1237–1248.
- Felipe-Marquez G, Nombela-Palomo M, Palomo-Alvarez C, et al. Binocular function changes produced in response to overnight orthokeratology. Graefes Arch Clin Exp Ophthalmol. 2017;255:179–188.
- Gifford K, Gifford P, Hendicott PL, et al. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Cont Lens Anterior Eye. 2017;40:184–189.
- Kang P, Watt K, Chau T, et al. The impact of orthokeratology lens wear on binocular vision and accommodation: a short-term prospective study. Cont Lens Anterior Eye. 2018;41:501–506.
- Tarutta EP, Tarasova NA, Milash SV, et al. The influence of different means of myopia correction on peripheral refraction depending on the direction of gaze. Vestn Oftalmol. 2019;135:60–69.
- Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2019;102:364–377.
- Si JK, Tang K, Bi HS, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92:252–257.
- Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104:363–368.
- Sankaridurg P, Donovan L, Varnas S, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87:631–641.
- Sankaridurg P, Bakaraju RC, Naduvilath T, et al. Myopia control with novel central and peripheral plus contact lenses and extended depth of focus contact lenses: 2 year results from a randomised clinical trial. Ophthalmic Physiol Opt. 2019;39:294–307.
- Li SM, Kang MT, Wu SS, et al. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic Physiol Opt. 2017;37:51–59.