ABSTRACT
Clinical relevance
Physical activity is an essential part of childhood physical and mental development. Recent research identified visual problems associated with a sedentary lifestyle in children in Ireland.
Background
This study explored the association between visual function in children and their engagement with physical activities outside school.
Methods
Participants were 1,626 schoolchildren (728 aged 6–7-years, 898 aged 12–13-years) in randomly selected schools in Ireland. Before data collection, parents/legal guardians of participants completed a standardised questionnaire reporting physical activity as no activity (mostly on screens), light activity (occasional walking/cycling), moderate activity (<3 hrs/week engaged in sports), or regular activity (>3hrs/week engaged in sports). Measurements included logMAR monocular visual acuities (with spectacles and pinhole), in the distance (3 m) and near (40 cm), stereoacuity (TNO stereo-test), cover test, and cycloplegic autorefraction (1% cyclopentolate).
Results
Controlling for confounders (socioeconomic disadvantage and non-White ethnicity), linear regression analysis revealed presenting distance visual acuity, near visual acuity, and stereoacuity were significantly better amongst participants who reported regular physical activity rather than moderate, light or no activity in both 6–7-year-old and 12–13-year-old participants. Absence of clinically-significant refractive error (>−0.50D < 2.00D) was associated with regular physical activity. Participants presenting with visual impairment (better-eye vision <6/12) (odds ratio = 5.78 (2.72–12.29)), amblyopia (pinhole acuity ≤6/12 plus an amblyogenic factor) (odds ratio = 5.66 (2.33–13.76)), and participants at school without their spectacles (odds ratio = 2.20 (1.33–3.63)), were more likely to report no activity.
Conclusions
Children regularly engaged in physical activities, including sports; had better visual and stereoacuity; and were less likely to need spectacles. Visual impairment, amblyopia, and refractive error were associated with no physical activity. Spectacle wear compliance was associated with regular physical activity. Regular physical activity is an essential factor in childhood vision and addressing visual impairment in children is vital to increasing participation in sports and exercise. Socioeconomically disadvantaged and non-White communities would benefit most from these measures.
Introduction
Vision impairment (VI) is increasing globally due to ageing populations,Citation1 and increasingly myogenic lifestyles,Citation2 including sedentary living.Citation3 Physical inactivity accounts for 9% of worldwide premature mortality.Citation4 The Irish Children’s Sport Participation and Physical Activity (CSPPA) study reported only 19% of children (10-12-year-olds) and 12% of adolescents (12-18-year-olds) achieve the recommended levels of physical activity for good health (60 minutes of moderate- to vigorous-intensity physical activity per day).Citation5 Worryingly, the likelihood of meeting the recommended physical activity levels decreases with age.Citation5 The World Health Organisation estimated the direct healthcare costs and lost economic output associated with physical inactivity at between €150–300 (AUD220–440) per citizen per year.Citation6 Physical activity in childhood is associated with health in adulthood. Hence, physical inactivity in children is considered one of the most urgent health concerns affecting society and policymakers internationally.Citation6
In addition to vascular and neurological benefits, regular physical activity is associated with positive mental health, slower cognitive decline, reduced body fat and cancer prevalence.Citation7 Physical activity benefits the nervous and visual systems due to shared embryological origins.Citation8 Moreover, physical activity appears to offer a protective effect against myopia progression.Citation9 By contrast, lower physical activity levels are associated with earlier onset age-related macular degeneration, glaucoma, diabetic retinopathy,Citation8 depression and anxiety.Citation10 Adults with amblyopia avoid visually demanding sports due to issues anticipating moving targets.Citation11 Of further concern, visually impaired adults experience barriers to engaging in physical activities.Citation12 Likewise, visually impaired children and adolescents are less likely to engage in physical activity,Citation13 and sports.Citation14
While regular engagement in sports and physical activities is critical for health and well-being, health gains from interventions targeting children lifestyles occur 40–50 years in the future.Citation7 Thus, effective policies targeting childhood physical inactivity, including reducing sedentary lifestyle behaviours, require an understanding of susceptible cohorts.
Recent research identified ‘visual problems’,Citation15 including myopia,Citation2 associated with decreased physical activity in children in Ireland. However, the association between specific aspects of visual function, level of visual acuity (VA) and physical activity engagement in schoolchildren in Ireland remain unknown. This study investigated the association between various aspects of visual function, including VA, stereoacuity, VI, amblyopia and uncorrected refractive error, with parent-reported hours of engagement in outside-school physical activity.
Methods
Sampling, recruitment protocols, participation rates, experimental techniques and methods employed are previously described in detail.Citation16 Stratified random sampling was used to obtain representative samples of children in mainstream schools in Ireland. Schools were stratified by primary/post-primary status, urban or rural living, and socioeconomic status. The Technological University Dublin Research Ethics Committee granted ethical approval, and the study adhered to the tenets of the Declaration of Helsinki.
Public involvement
During the design stage of the study, focus groups were engaged to assess the burden associated with and the time to complete the study questionnaire.Citation16 The study used parent/legal guardian reported measures as a proxy for engagement in physical activities outside school. Previous research found parental reports of physical activity aligned with objectively measured physical fitness.Citation17
Data collection
Data were collected between June 2016 and January 2018. Participants were 1,626 schoolchildren in Ireland: 728 participants aged 6-7-years-old (377 boys and 351 girls) and 898 participants aged 12-13-years-old (504 boys and 394 girls). Ethnicity was as follows: White (combined: White 1346 participants) or non-White (combined: Black 80, East Asian 51, and South Asian 49).
Questionnaire
Parents/legal guardians of the participants completed a standardised eye health and lifestyle questionnaire reporting inter-alia, eye and vision problems, medical and previous eye examination, parental education and employment status. Completed questionnaires were returned to the first author in advance of data collection. The parents/legal guardians of participants reported the level of physical activity by answering the following question: ‘Which of the following best describes your child’s level of physical activity outside school? (Tick one box only):
Spends all or most leisure time on phone/computer/TV (no activity).
Spends time occasionally in light physical activities (e.g., walking, cycling), (light activity).
Participates in regular sporting activities for up to 3 hours a week (e.g., football, swimming, gymnastics, basketball, etc.), (moderate activity).
Participates in regular sporting activities for more than 3 hours a week (e.g., football, swimming, gymnastics, basketball, etc.), (regular activity)”.
Hereafter referred to as no activity, light activity, moderate activity, and regular activity.
Assessed parental factors were paternal and maternal education level (first-level, second-level, third-level); and occupation (full-time paid work, part-time paid work, unemployed, looks after family full-time).
Examinations
Children with written informed consent from parents/legal guardians and child assent were examined on their school premises within school hours. The examination involved: Vision: monocular logMAR presenting (with spectacles if worn) VA were measured and scored by-letter with and without a pinhole at three metres and 40 cm. The TNO anaglyph stereo-test (Richmond products, South San Francisco, CA 94,080, USA) was used to quantify the degree of stereoacuity. Ocular alignment was evaluated using a cover-uncover test and an alternating cover test, using an accommodative target with and without spectacle correction (if worn) in the distance (3 m) and at near (40 cm).
Amplitude of accommodation was measured using a Royal Air Force rule, the push-up method. Cycloplegic autorefraction (Dong Yang Rekto ORK-11 Auto Ref-Keratometer) was performed at least 30 minutes post instillation of anaesthetic (Minims Proxymetacaine Hydrochloride 0.5% w/v, Bausch & Lomb, UK) and cycloplegic eye drops (Minims Cyclopentolate Hydrochloride 1% w/v, Bausch & Lomb, UK). The representative value for spherical equivalent refraction (SER) - sphere plus half the cylindrical value – was used in subsequent analysis.
Vision disorders were classified as follows: amblyopia (pinhole VA ≥ 0.3logMAR in the affected eye, plus the presence of an amblyogenic factor),Citation18 strabismus (misaligned eyes), significant refractive error (myopia SER≤−0.50 dioptre (D), hyperopia ≥2.00D, astigmatism ≥ 1.00D, anisometropia interocular difference SER ≥ 1.00D), and VI (presenting VA > 0.30logMAR in the ‘‘better eye’). Follow up: Subsequent to the examination, all parents/legal guardians received a detailed report advising them of the study findings and the necessity of any further treatment if required.
Statistical methodology
Data were analysed using statistical software package version 27 (IBM-SPSS Inc., Chicago, IL, USA). Categorical data are presented as a percentage, and continuous data are presented as the mean (standard deviation (SD)). Kolmogorov-Smirnov tests were performed to check data distribution. Logistic regression models were fitted to investigate the association and estimate the odds ratio (OR) and 95% CIs for sociodemographic and visual factors associated with physical activity. The primary outcomes examined were VA, stereoacuity, VI, amblyopia, and clinically significant refractive error by physical activity level.
Logistic regression analysis, with participants who reported ‘no physical activity’ as the reference category, was employed to examine the relationship of physical activity engagement with categorical variables while controlling for confounders. Presenting VA (logMAR) and stereoacuity (arc-seconds) were analysed as continuous variables in the multiple linear regression models. Amblyopia means amblyopia in either the right eye, left eye, or both. The 5% significance level has been used throughout, without correction for multiple tests.
Results
Statistical analysis of study questionnaires and examination results included 723 of the 728 6-7-year-olds (response-rate = 99.3%) and 887 of the 898 12-13-year-olds (response-rate = 98.8%). Parents/legal guardians reported 10.4% of 6-7-year-old and 14.4% of 12-13-year-old participants as ‘no physical activity’; 30.3% of 6-7-year-olds and 14.3% of 12-13-year-olds as ‘light physical activity’; 32.6% of 6-7-year-olds and 26.2% 12-13-year-olds as ‘moderate physical activity’ and 26.7% 6-7-year-olds and 45.1% of 12-13-year-olds as ‘regular physical activity’.
Sociodemographic factors associated with physical activity
Sex (OR = 0.93, CI: 0.66–1.31, p = 0.68), urban or rural living (OR = 1.08, CI: 0.72–1.64, p = 0.71), and age-group (OR = 1.23, CI: 0.83–1.82, p = 0.32) were not associated with physical activity engagement; however, socioeconomic disadvantage (OR 6.76, CI 4.55–10.05, p < 0.001), and non-White ethnicity (OR = 8.05, CI 4.85–13.36, p < 0.001) were (). Unless otherwise stated, socioeconomic status and ethnicity are controlled for in all further analyses.
Table 1. The relationship between engagement in physical activity stratified by age in 723 6-7-years-old and 887 12-13-years-old participants and sociodemographic factors.
Parental factors
Regular physical activity engagement was positively associated with maternal education (third-level OR = 4.87, CI: 1.67–14.25, p < 0.001, second-level OR = 2.95, CI: 2.04–4.26, p < 0.001), and paternal education (third-level OR = 4.17, CI: 1.40–12.38, p = 0.01, and second-level OR = 2.98, CI: 2.02–4.39, p < 0.001); and maternal employment (full-time OR = 5.37, CI: 1.84–15.87, p = 0.01, and part-time OR = 7.38, CI: 2.48–21.99, p < 0.001), but not paternal employment (p > 0.05 across the employment categories) (Table S1).
Distance vision (3 m)
Distance presenting VA (better eye) was significantly better amongst participants who reported regular physical activity than participants who reported moderate, light or no physical activity 6-7-year-olds (F₃,720 = 5.02, p = 0.002). Similar results were found for the 12-13-year-old (F3,884 = 22.94, p < 0.001) participants ( and , where a higher value indicates poorer vision). Likewise, distance VA (worse eye) was significantly better amongst regular than moderate, light and no physical activity 6-7-year-olds (F₃,720 = 7.17, p < 0.001) and 12-13-year-olds (F3,884 = 18.88, p < 0.001).
Figure 1. Mean logMAR distance vision in the better eye by physical activity category in 6-7-year-olds (top image) and 12-13-year-olds (bottom image). Higher logMAR acuity scores represent poorer vision.
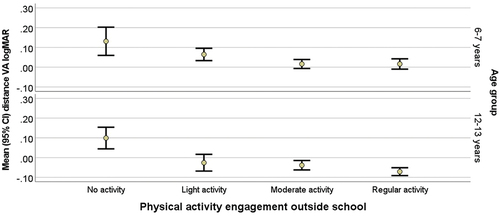
Table 2. The relationship between engagement in physical activity stratified by age in 723 6-7-years-old and 887 12-13-years-old participants and presenting visual acuity (distance 3 m and near 40 cm), presenting stereoacuity, and amplitude of accommodation.
Near vision (40 cm)
Near presenting VA (better eye) was significantly better amongst participants who reported regular rather than moderate, light, or no physical-activity 6-7-year-olds (F₃,720 = 4.71, p = 0.003) and 12-13-year-olds (F3,884 = 3.85, p = 0.009). Similar results were found for VA in the worse eye for 6-7-year-olds (F₃,720 = 4.71, p = 0.003) and 12-13-year-olds (F3,884 = 3.85, p = 0.009) ().
Stereoacuity
Stereoacuity was significantly better amongst 6-7-year-olds who reported regular rather than moderate, light or no physical activity (F₃,720 = 5.01, p = 0.02). Likewise, in 12-13-year-olds (F3,884 = 8.66, p < 0.001) ( and , where a higher value indicates poorer stereoacuity). When stereoacuity was examined as a categorical variable (abnormal stereoacuity >240 arc seconds), regular engagement in physical activities outside school was associated with better stereoacuity <240 arc seconds in 6-7-year-olds (OR = 2.14 CI: 1.12–4.11, p = 0.02) and 12-13-year-olds (OR = 2.44, CI: 1.37–4.33, p = 0.002) ().
Figure 2. Mean stereoacuity by physical activity category in 6-7-year-olds (top image) and 12-13-year-olds (bottom image). A higher stereoacuity reading represents poorer stereoacuity.
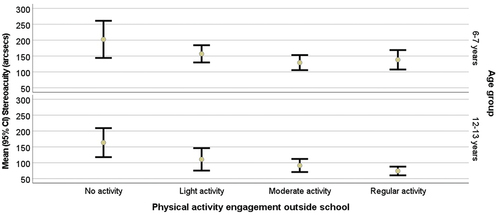
Table 3. The relationship between engagement in physical activity stratified by age in 723 6-7-years-old and 887 12-13-years-old participants and various aspects of visual function, (presenting visual impairment, amblyopia, refractive error and history of spectacle wear).
Hyperopia was associated with abnormal stereoacuity in both cohorts (6-7-years, OR = 3.00, 1.96–4.53, p > 0.001, 12-13-years OR = 10.53, 6.07–18.18, p < 0.001). Myopia was associated with abnormal stereoacuity in 12-13-year-olds (OR = 3.00, 1.96–4.53, p > 0.001), but not 6-7-year-olds (p = 0.21).
Amplitude of accommodation
There was no relationship between the amplitude of accommodation and physical activity engagement in 6-7-year-old (F₃,720 = 0.81, p = 0.49) and 12-13-year-old (F3,884 = 0.41, p = 0.75) participants ().
Visual function, refractive error and physical activity engagement
Overall, 36.5% of participants were reported by their parents or legal guardians as engaging in regular sporting physical activities for more than three hours per week. This was lower amongst participants with amblyopia (18.1% vs 37.9%, p < 0.001) and VI (18.3% vs 37.5% p < 0.001). displays the relationship between visual function, refractive error, and physical activity engagement in 6-7-year-old and 12-13-year-old participants.
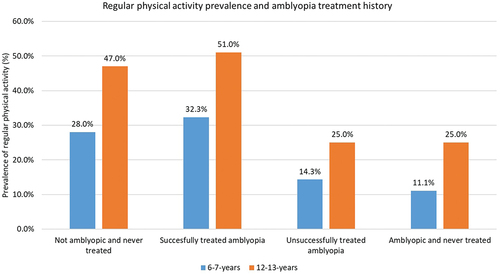
Amblyopia was associated with no physical activity in 6-7-year-olds (OR = 6.44, CI: 1.92–21.62, p = 0.002) and 12-13-year-olds (OR = 5.28, CI: 2.00–13.92, p < 0.001). Amongst participants with a reported history of amblyopia treatment (n = 116), participants successfully treated for amblyopia (n = 78) were significantly (OR = 5.02, CI: 1.65–15.28, p = 0.004) more likely to be active than unsuccessfully treated amblyopic participants (n = 38) and non-treated amblyopic participants (n = 45) ().
Figure 3. Prevalence of regular physical activity (>3 hrs/week) amongst 723 participants aged 6-7-year-old and 887 participants aged 12-13-year-old by amblyopia treatment history category: not amblyopic and no history of amblyopia treatment, previously amblyopic successfully treated for amblyopia, amblyopic and unsuccessfully treated, and amblyopic participants never treated.
No physical activity engagement was associated with VI in 6-7-year-olds (OR = 4.11, CI: 1.13–15.00, p < 0.001) and 12-13-year-olds (OR = 6.90, CI: 2.72–17.49, p < 0.001), ().
Strabismus was not associated with physical activity engagement in either age group (6-7-years: p = 0.33, 12-13-years, p = 0.26). Anisometropia was associated with no physical activity in 12-13-year-olds (p = 0.006) but not 6-7-year-olds (p = 0.58).
The absence of clinically significant refractive error (SER>-0.50D < 2.00D) was associated with regular physical activity in 6-7-year-olds (OR = 1.73, CI: 1.11–2.70, p = 0.015) and 12-13-year-olds (OR = 2.00, CI: 1.32–3.04, p < 0.001). By contrast, refractive errors (myopia: 6-7-year-olds, OR = 6.82, CI: 1.30–35.97, p = 0.02, 12-13-year-olds: OR = 3.13, CI: 1.89–5.15, p < 0.001), and astigmatism, (6-7-year-olds: OR = 2.02, CI: 1.13–3.62, p = 0.01, 12-13-year-olds: OR = 2.22, CI: 1.44–3.42, p < 0.001) were associated with no physical activity ().
Spectacle wear
Wearing spectacles was not associated with physical activity engagement in 6-7-year-olds (p = 0.61). Amongst 12-13-year-olds, there was no difference in physical activity level between participants wearing spectacles and those who did not need spectacles (p = 0.32). However, 12-13-year-old participants at school without their spectacles were significantly more likely to report no physical activity (OR = 2.27, CI: 1.26–4.12, p = 0.007) ().
displays the odds ratio for visual factors associated with no physical activity engagement, controlling for confounders (socioeconomic disadvantage and non-White ethnicity).
Table 4. Odds ratio for visual factors associated with no physical activity controlling for confounders (socioeconomic status and ethnicity) in 1,610 participants (723 aged 6-7-years and 887 aged 12–13 years) in the Ireland Eye Study.
Discussion
This study is the first to explore the relationship between eyesight and parent/legal guardian-reported hours of engagement in physical activities outside school in children attending mainstream schools in Ireland. The present study findings demonstrate children who have better VA, finer stereoacuity and do not need spectacles, are more likely to regularly engage in physical activity, including sports, than children who have reduced VA, reduced stereoacuity, and are in need of spectacles.
Overall, one in three participants reported engaging in physical activity outside school for over three hours per week. However, participants who reported no physical activity were significantly more likely to be visually impaired, aligning with previous research.Citation14 These findings are important as overall, one in ten participants reported no physical activity, yet this rose to one in three amongst visually impaired participants. Moreover, participants with amblyopia and refractive error spent less time engaged in physical activities outside school.
In addition to the main findings, this study demonstrates parental/legal guardian level variables (education and employment) partly explain the inequality in physical activity levels. Aligning with the literature, physical inactivity was associated with socioeconomic disadvantage and ethnic minority status.Citation19 Moreover, parental/legal guardian educational level and occupation group were strong indicators of physical inactivity and VI in participants, demonstrating the importance of education. Lower parental educational levels and social class may indirectly affect physical activity levels by reducing exposure to sports, co-participation and transportation.Citation20
The substantial costs associated with sports kit and coaching is another socioeconomic factor potentially limiting sports participation.Citation19 Fogelholm et al. established that the parent-child inactivity relationship was more potent than parent-child vigorous activity concluding parents wishing to modify the activity levels in their children may need to address their own.Citation21 Interestingly, the relationship between visual function and engagement in outside-school activities was significant despite controlling for sociodemographic factors in the present study.
The assessment of VA measures the ability to see detail, and this study found participants who regularly engaged in physical activities had excellent VA. Notably, the mean average VA (worse-eye) in physically active participants was better than 0.00 logMAR (6/6). This finding aligns with prior research where superior VA levels were found in Olympic-level athletes who participated in sports ranging from track and field to ice hockey, soccer, softball and speedskating.Citation22 Interestingly, Laby et al. found some differences in visual function; archers had superior VA (small stationary bullseye target) but poorer stereoacuity than soccer players, speedskaters, and softball players (dynamic sports involving larger targets and three-dimensional position awareness).Citation22
In the present study, active participants who regularly engage in physical activities, including sports, had excellent stereoacuity (threshold level of depth perception), agreeing with prior research involving dynamic sports such as table tennis,Citation23 and soccer.Citation24 Stereoacuity enables a person to judge the relative position of objects in three-dimensional space. Stereoacuity is vital in dynamic sports involving a moving target, such as ball sports, where players must perform critically timed depth estimations.Citation24 Monocular cues such as lines and shadows facilitate depth awareness to a limited degree; however, binocular cues are superior due to subtle differences in images formed on the retina of the fellow eye.Citation24 However, the assessment of stereopsis using any static test cannot take into account the rapid changes in vergence required when a ball is moving towards a participant, and the measurement of near stereoacuity may not give a reliable measure of distance stereoacuity.Citation25 Despite the limitations associated with the TNO stereotest and other static stereotests, the TNO test is regularly used in optometric practice, and any near stereopsis deficit might be similar at distance viewing.Citation25
In addition to good distance VA and near stereoacuity, physically active participants also had excellent near VA. While this is interesting, there is a paucity of literature addressing detailed visual functions for specific sports; hence, the mean level of VA required for specific sport remains largely unknown. The visual skills necessary for successful involvement in specific sports involve a detailed visual task analysis; hence, further research using specific outcome measures combining vision assessment and sports performance data is needed.Citation26
Although the present study found no association between the amplitude of accommodation and physical activity; nevertheless, it should be noted that the push-up method employed in the present study may overestimate accommodation amplitude.Citation27 As exemplified by Jafarzadehpur, and Yarigholi,Citation28 where no difference in the amplitude of accommodation between table tennis champions and non-players was found, champion table tennis players nonetheless had a significantly enhanced accommodative facility. Hence, further analysis of accommodative function is required to understand the relationship between dynamic sports and dynamic accommodation response.
The absence of clinically significant refractive error was strongly associated with regular physical activity. Whereas no statistically significant relationship between hyperopia and physical activity/inactivity engagement was found. Conversely, myopia and astigmatism were significantly associated with no physical activity aligning with prior research involving Chinese 13-year-olds.Citation29 Similarly, Hansan et al.Citation30 reported low physical activity and excessive screentime related to myopia in Danish teenagers.
In Ireland, prior research involving the same dataset reported that myopic 12-13-year-olds spend more time on screens, less outdoors, and less time engaged in physical activities than emmetropic 12-13-year-olds.Citation2 Furthermore, Zeri et al.Citation31 reported engagement in outdoor sports associated with lower levels of myopia. Hence, it may be time spent outdoors and less time on screens and not the physical activity itself offering a protective effect against myopia.Citation32 For example, Read et al.Citation32 found emmetropes spend significantly more time outdoors during daylight than myopes. Still, in contrast to the present study, they found no significant association with physical activity.Citation32 Hence, not being indoors engaged in near sedentary activities may be as important as being engaged in outdoor physical activities.Citation33 Longitudinal research employing objectively measured physical activity, light exposure and consistent and precise outcome measures is recommended.
There was no significant difference in physical activity level in the present study between participants wearing spectacles and those who did not. However, participants at school without their prescribed spectacles, as they were lost or damaged, were twice as likely to report no physical activity. Reasons for non-compliance with spectacle wear identified in the literature are socioeconomic disadvantage,Citation16 broken or lost spectacles, parental disapproval, and forgetfulness.Citation34 Nevertheless, when socioeconomic status and ethnicity were controlled for in the analysis, the significant relationship between physical inactivity and spectacle non-compliance persisted. Thus, in addition to early identification, diagnosis and treatment of refractive errors, healthcare education and strengthening vision care services are vital.
Recent research identified children with amblyopia had lower athletic competence (aiming and catching skills) than controls.Citation35 Similarly, in the present study, participants with amblyopia were almost six times more likely to report no physical activity than participants without amblyopia. Indeed, participants successfully treated for amblyopia were five times more likely to be regularly physically active than amblyopic participants. Binocular vision is essential for dynamic sports,Citation23 and amblyopic children will have very poor or no stereoacuity; hence, amblyopic participants are less likely to excel in some sporting activities. Moreover, amblyopic adults are more likely to avoid visually demanding sports due to issues catching a ball and balance.Citation11 However, physical activity improves brain plasticity.Citation36
Also, visual (homoeostatic) plasticity can be boosted with physical exercise in amblyopic,Citation36 and non-amblyopic individuals.Citation37 Studies have repeatedly shown increased physical activity associated with reduced neuroinflammation.Citation38 For instance, neuro-inflammation affects brain structures, including the cortex (where visual information is processed), hippocampus (where sense is made of what is seen), brainstem (controls eye movements),Citation38 and thus, it stands to reason that physical inactivity may affect visual function. The present study highlights the positive impact and importance of addressing amblyopia, primarily preventable VI, before school onset when treatment is more likely to succeed,Citation39 to support health in later life.
In line with previous findings,Citation6 the present study found VI impacts physical activity engagement, which is concerning, as physical inactivity is associated with increased susceptibility to metabolic diseases and reduced high-level brain processing and function.Citation38 Reported fitness levels for visually impaired children are poorer than sighted children.Citation13 Understanding the hurdles and barriers to engaging in sports and physical activities visually impaired children encounter is vital. Consequently, children with VI are a critical target group when designing interventions to improve inclusion in sports and other physical activities.
The extensive range of variables and high participation rate in the Ireland Eye Study data set facilitates in-depth analysis of the relationship between physical activity engagement and visual function while examining the part sociodemographics play in this relationship. While visual function formed part of the examination, physical activity was measured via a questionnaire, which may inflate physical activity differences, underestimate the connection between eyesight and activity, or overestimate physical activity engagement.Citation21
Future studies should include objective and exact measurements of time children spend in physical activities to verify the independent effect of time spent on sedentary or physical activity and the presence and magnitude of refractive error myopia and other visual factors. Although study findings are based on cross-sectional data, they are meaningful for childhood development as childhood physical activity habits track into adulthood.Citation40 Understanding the prevalence of physical activity and inactivity and identifying barriers to engaging in physical activity in children in Ireland will help guide public health policy.
Conclusions
Children who have better visual and stereoacuity and do not need spectacles, are more likely to regularly engage in physical activity, including sports, than children who have reduced visual acuity and stereoacuity, and are in need of spectacles. Visual impairment, amblyopia, astigmatism and myopia were associated with sedentary lifestyles. Socioeconomically disadvantaged and non-White children were particularly affected. The relationship between visual function and physical activity engagement may be bidirectional; it is hard to unravel whether physical inactivity results in reduced VA or reduced VA results in reduced physical activity engagement. Nevertheless, engaging in physical activities and reducing near sedentary activities are modifiable lifestyle changes that may prevent VI and refractive errors such as myopia. Eyecare clinicians should incorporate an assessment of physical activity engagement into consultations, include physical activity advice and plans in managing children’s eyecare, and assess the benefits during follow-up.
Public health education programmes on increasing physical activity and reducing sedentary lifestyles are vital for schoolchildren and families. While investment in promoting and prescribing physical activity for all children is critical, policymakers should ensure socioeconomically disadvantaged, non-White and visually impaired children are further supported to participate in physical activity. Not only will the health benefits associated with physical activity manifest themselves in childhood but also in adulthood, where the benefits at that time will be material with significant benefits for not only the individual but also the community in terms of independence and quality of life.
Supplemental Table 1
Download PDF (30.1 KB)Acknowledgements
The authors would like to thank Professor Kathryn Saunders (NICER study, School of Biomedical Sciences, University of Ulster, County Londonderry, Northern Ireland) and Dr Jim Stack (Biostatistician Waterford Institute of Technology) for their valuable input in the Ireland Eye Study. In addition, the authors would like to acknowledge the support and participation of the schools, the children, and their parents and guardians in the Ireland Eye Study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/08164622.2022.2106780.
References
- Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, Leasher J, Limburg H, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 2017; 5: e888–e897.
- Harrington SC, Stack J, O’Dwyer V. Risk factors associated with myopia in schoolchildren in Ireland. Br J Ophthalmol 2019. Epub ahead of print. doi:10.1136/bjophthalmol-2018-313325.
- Smith L, Timmis MA, Pardhan S. Physical inactivity in relation to self-rated eyesight: cross-sectional analysis from the English longitudinal study of ageing. BMJ Open Ophthalmol 2017; 1. Epub ahead of print. doi:10.1136/BMJOPHTH-2016-000046.
- Lee I, Shiroma E, Lobelo F. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012; 380: 219–229.
- Woods C, Powell C, Saunders J. The children’s sport participation and physical activity study 2018. 2018 [cited 2021 Nov 6]. https://pure.ulster.ac.uk/ws/files/77672771/CSPPA_Final_Report.pdf.
- Cavill N, Kahlmeier S, Racioppi F. Physical activity and health in Europe: evidence for action - European University Institute. Copenhagen: European University Institute; 2006 [cited 2022 Jan 23]. http://link.library.eui.eu/portal/Physical-activity-and-health-in-Europe–evidence/2UMuQyc_SoU/2006.
- Cecchini M, Sassi F, Lauer JA. Chronic diseases: Chronic diseases and development 3 tackling of unhealthy diets, physical inactivity, and obesity : health eff ects and cost-eff ectiveness. Lancet 2010; 376: 1775–1784.
- Ong SR, Crowston JG, Loprinzi PD. Physical activity, visual impairment, and eye disease. Eye 2018; 32: 1296–1303.
- Suhr Thykjær A, Lundberg K, Grauslund J. Physical activity in relation to development and progression of myopia – a systematic review. Acta Ophthalmol 2017; 95: 651–659.
- Uddin R, Burton NW, Khan A. Combined effects of physical inactivity and sedentary behaviour on psychological distress among university-based young adults: a one-year prospective study. Psychiatr Q 2020; 91: 191–202.
- Kumaran SE, Khadka J, Baker R. Functional limitations recognised by adults with amblyopia and strabismus in daily life: a qualitative exploration. Ophthalmic Physiol Opt 2019; 39: 131–140.
- Zult T, Smith L, Stringer C. Levels of self-reported and objective physical activity in individuals with age-related macular degeneration. BMC Public Health 2020; 20: 1–10.
- Aslan UB, Calik BB, Kitiş A. The effect of gender and level of vision on the physical activity level of children and adolescents with visual impairment. Res Dev Disabil 2012; 33: 1799–1804.
- Tindall DW, Foley JT, Beets MW. Physical activity levels of children with visual impairments during an adapted sports camp. Br J Vis Impair 2017; 35: 143–153.
- Quigley C, Zgaga L, Vartsakis G. Refractive error and vision problems in children: association with increased sedentary behavior and reduced exercise in 9-year-old children in Ireland. J Am Assoc Pediatr Ophthalmol Strabismus 2019. Epub ahead of print. doi:10.1016/J.JAAPOS.2018.12.011.
- Harrington SC, Stack J, Saunders K. Refractive error and visual impairment in Ireland schoolchildren. Br J Ophthalmol 2019; 103: 1112–1118.
- Palou P, Muntaner-Mas A, Cantallops J, Borràs PA, Labayen I, Jiménez-Pavón D, Dorado García C, Moliner-Urdiales D, Rodríguez Pérez MA, Rojo-Tirado MA, et al. A single question of parent-reported physical activity levels estimates objectively measured physical fitness and body composition in preschool children: the PREFIT project. Front Psychol 2019; 10: 1585.
- Xiao O, Morgan IG, and Ellwein LB. Prevalence of amblyopia in school-aged children and variations by age, gender, and ethnicity in a multi-country refractive error study. Ophthalmology 2015; 122(06): 1924–1931.
- Armstrong S, Wong CA, Perrin E. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: findings from the national health and nutrition examination survey, 2007-2016. JAMA Pediatr 2018; 172: 732–740.
- Doggui R, Gallant F, Bélanger M. Parental control and support for physical activity predict adolescents’ moderate to vigorous physical activity over five years. Int J Behav Nutr Phys Act 2021; 18: 1–10.
- Fogelholm M, Nuutinen O, Pasanen M. Parent-child relationship of physical activity patterns and obesity. Int J Obes Relat Metab Disord 1999; 23: 1262–1268.
- Laby DM, Kirschen DG, Pantall P. The visual function of olympic-level athletes - an initial report. Eye Contact Lens 2011; 37: 116–122.
- Zhu XJ, Li YH, Liu LQ. Functional significance of stereopsis in professional table-tennis players. J Sports Med Phys Fitness 2019; 59: 1798–1804.
- Paulus J, Tong J, Hornegger J. Extended stereopsis evaluation of professional and amateur soccer players and subjects without soccer background. Front Psychol 2014; 5. Epub ahead of print. doi:10.3389/FPSYG.2014.01186.
- Chopin A, Bavelier D, Levi DM. The prevalence and diagnosis of ‘stereoblindness’ in adults less than 60 years of age: a best evidence synthesis. Ophthalmic Physiol Opt 2019; 39: 66–85.
- Laby DM, Appelbaum LG. Review: vision and on-field performance: a critical review of visual assessment and training studies with athletes. Optom Vis Sci 2021; 98: 723–731.
- Burns DH, Allen PM, Edgar DF. Sources of error in clinical measurement of the amplitude of accommodation. J Optom 2020; 13: 3–14.
- Jafarzadehpur E, Yarigholi MR. Comparison of visual acuity in reduced lumination and facility of ocular accommodation in table tennis champions and non-players. J Sports Sci Med 2004; 3: 44.
- Zhu W, Zhang L, Zhang L. Association of physical activity and sedentary behaviors with the risk of refractive error in Chinese Urban/Rural boys and girls. Sustainability 2022; 14. Epub ahead of print. doi:10.3390/su14095539.
- Hansen MH, Laigaard PP, Olsen EM. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study. Acta Ophthalmol 2020; 98: 315–321.
- Zeri F, Pitzalis S, Di Vizio A. Refractive error and vision correction in a general sports-playing population. Clin Exp Optom 2018; 101: 225–236.
- Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 2014; 91: 330–341.
- Ngo C, Saw SM, Dharani R. Does sunlight (bright lights) explain the protective effects of outdoor activity against myopia? Ophthalmic Physiol Opt 2013; 33: 368–372.
- Dhirar N, Dudeja S, Duggal M. Compliance to spectacle use in children with refractive errors - a systematic review and meta-analysis. BMC Ophthalmol 2020; 20: 1–11.
- Birch EE, Castañeda YS, Cheng-Patel CS. Self-perception of school-aged children with amblyopia and its association with reading speed and motor skills. JAMA Ophthalmol 2019; 137: 167–174.
- Lunghi C, Sframeli AT, Lepri A. A new counterintuitive training for adult amblyopia. Ann Clin Transl Neurol 2019; 6: 274.
- Lunghi C, Sale A. A cycling lane for brain rewiring. Curr Biol 2015; 25: R1122.
- Tyndall AV, Clark CM, Anderson TJ. Protective effects of exercise on cognition and brain health in older adults. Exerc Sport Sci Rev 2018; 46: 215–223.
- Holmes JM. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol 2011; 129: 1451.
- Smith L, Gardner B, Hamer M. Childhood correlates of adult TV viewing time: a 32-year follow-up of the 1970 British cohort study. J Epidemiol Community Health 2015; 69: 309–313.
