ABSTRACT
Clinical relevance
Optimisation of vision screening programmes can result the detection of refractive anomalies in a high proportion of school children.
Background
The Refractive Errors Among Children (REACH) programme aims to optimise outcomes of school-based vision screening in India by collaborating with hospitals and monitoring eye care throughout school attendance.
Methods
REACH delivers school vision screening using pocket vision screeners (cards presenting rows of seven 0.2 logMAR Sloan letters at a 3 m viewing distance) in five states across India. Children who fail screening are referred for detailed evaluation including refraction, those requiring cycloplegic refraction are referred to partner hospitals. Spectacles are dispensed as needed and compliance is assessed. All data are recorded electronically.
Results
Out of 2,240,805 children aged 5 to 18 (mean 11.5; SD ±3.3) years, 2,024,053 have undergone REACH screening in 10,309 schools predominantly in rural locations (78.7%) and government-funded (76%). Of those screened, 174,706 (8.6%) underwent detailed evaluation. A higher proportion of children in private or urban schools (11.8% and 10.4% respectively) were referred for detailed evaluation than those in government-funded or rural schools (5.9% and 7.2%, respectively; p < 0.001). The proportion referred for detailed evaluation differed by state (p < 0.001), from 4.0% in West Bengal to 14.4% in Kerala.
Conclusion
The REACH programme screened a high proportion of school children, providing further care and follow-up to optimise visual outcomes.
Introduction
Evidence from the Refractive Error Study in Children confirms that refractive error is the commonest cause of visual impairment among children aged between 5 and 15 years globally, responsible for 63%–77% of blindness and severe visual impairment.Citation1 An estimated 680,000 children in India are blind, including about one third with uncorrected refractive error, the highest number in the world.Citation2,Citation3 Uncorrected refractive errors have a significant negative impact on pre-school literacyCitation4 and adherence to spectacle wear in school children improves literacy, with positive implications for their education.Citation5
The World Health Organization recommends school eye health screening as a cost-effective strategy to address uncorrected refractive error and other eye health problems among school-going children.Citation6 Such screening occurs in various forms globally,Citation7 and for over three decades has been an important activity of the Indian National Programme for Control of Blindness and Visual Impairment. The aim of vision screening is to identify treatable vision problems, educate children and families about them, and to refer if necessary. However, school-based eye care has the potential to provide a complete system of screening, correction of refractive error and follow-up assessment of spectacle compliance.Citation6 The latter is important, since spectacle prescribing helps no-one unless the prescribed correction is worn as required. To date, very limited data are available on compliance with spectacle wear among children receiving spectacles in India and other lower-middle income countries, or on the proportion requiring changes in refractive correction at follow-up.Citation8–10
Vision screening with the provision of free spectacles aids compliance with spectacle wear and may thus improve educational outcomes,Citation7,Citation11 indicating the importance of effective vision screening, which requires competent personnel. School-based vision screening and eye care services in India have involved volunteer school-teachers in primary vision screening. This reduces the workload of ophthalmic personnel. A 2012 review on school-based correction of refractive error found that teachers may provide effective detection of refractive error.Citation12 However, more recent research suggests that this strategy may result in high levels of false positivityCitation13 and variable levels of sensitivity,Citation14 with the latter dependent on training of teachers for this role.
The Refractive Error Among CHildren (REACH) programme was designed to address known challenges in traditional school eye care services (the inclusion of all school children using a standardised protocol and correction of significant refractive errors), to generate evidence for future interventions, and to build an innovative, sustainable and scalable programme for school-based eye care services. The programme has a strong focus on eye health promotion, engaging all stakeholders with the aim of promoting positive eye health-seeking behaviour. The main objectives of this paper are to describe in detail the process and protocol for implementation of the REACH programme across five states in India and its progress to date, and to raise awareness of this novel approach to child vision screening with scope for wider implementation.
Methods
The REACH programme
In India, recommendations for school vision screening include personnel training, screening, refraction, referral and spectacle dispensing, the latter by an optician near the school.Citation15 Traditionally, childhood vision screening involves monocular visual acuity testing to identify uncorrected refractive error and other ocular abnormalities. The School Vision Screening programme in India includes provision of spectacles as an essential component with the cost borne by the National Program for Control of Blindness and Visual ImpairmentCitation16 or shared between funders and parents.Citation17 The School Vision Screening protocol indicates that one teacher selected from each school undergoes one day of training, including appropriate viewing distance and use of an acuity target.Citation15 For those children who fail screening, refraction is conducted by an ophthalmic assistant at a health centre.Citation17
REACH is an innovative and unique model for school eye care services with standardised guidelines and procedures, and comprehensive processes including diagnosis, management, referral and compliance assessment. The programme is a collaboration between OrbisCitation18 and partner hospitals (research, education and clinical specialist centres) in India. Orbis provides REACH with digital and clinical equipment and the relevant partner hospital provides necessary eye care for any referred children.
REACH also monitors compliance with spectacle wear and encourages positive eye health-seeking behaviour using information, education, and communication (IEC) materials. These include pictorial explanations for children about an eye test and about the advantages of wearing any prescribed spectacles. For example, a book, the ‘Singing Tree’Citation19 was developed for the REACH project telling a locally relevant story about a child with poor vision whose everyday life is improved by wearing spectacles. The IEC materials were developed in a knowledge, attitudes and practice study on barriers to school-based eye care conducted by an independent research agency. Results have been presented but have not been published.
All REACH service delivery activities are undertaken by trained teams, and schoolteachers are oriented to promote good school eye health practices and to liaise with the eye health teams. provides a summary of the key features of the REACH programme compared with previous school-based vision screening or eye care services and highlights the rationale for each innovative feature of REACH.
Table 1. A summary of features of the REACH model compared with existing school-based vision screening or eye care services outlining the rationale for the new features of the REACH programme.
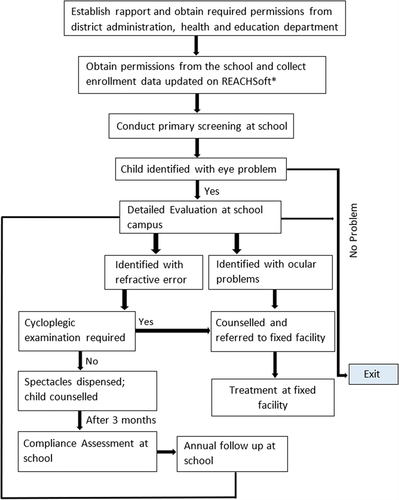
The programme process includes primary screening, detailed evaluation, spectacle management, counselling, referral, compliance assessment, and annual follow-up. Data from each step are recorded using custom software (REACHSoft), described below.
Study area and sample
To date, the REACH programme has been implemented in partnership with six hospitals in the Indian states of Kerala, Madhya Pradesh, Maharashtra, Tamil Nadu and West Bengal ().
Figure 1. The six partner hospitals in the REACH project, located in Kerala (Little Flower), Tamil Nadu (Sankara Nethralaya and Aravind), Maharashtra (HV Desai), Madhya Pradesh (Sadguru Netra Chikitsalaya) and West Bengal (VMA Netra Niramaya Niketan).
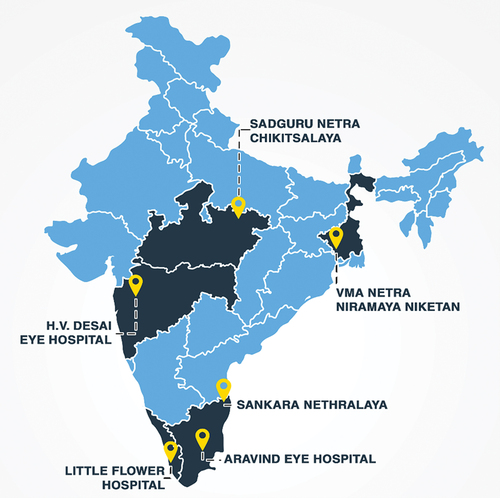
In each region (the area served by each of the hospitals), one district not previously provided with vision screening services was selected for inclusion in the programme. In districts with large populations a part of the district was defined. A list of schools within each district or partial district was compiled by the project manager or co-ordinator in collaboration with the Department of Education. The school locations were mapped using a geographic information system and the relevant latitude/longitude data were recorded. All of those schools were eligible for inclusion, and agreement for the school to participate was sought from the district education officer and from the school itself. Only those schools for which agreement was not given were excluded.
Ethical approval
Each of the six partner hospitals obtained ethical approval from their Institutional Review Board. Information was sent to all parents whose children were identified for detailed evaluation asking them to respond if they did not wish their child to participate in the REACH school eye health programme.
Programme team
The REACH team at each school is led by a project manager with overall responsibility and includes the personnel described in .
Table 2. Details of staff involved in each REACH project team and their training.
A role mapping exercise was completed at the beginning of the programme to designate tasks and roles to individuals. All personnel underwent training in the REACH programme, its aims, processes () and guidelines.
REACHSoft
Dedicated, custom software (REACHSoft) was developed for this programme to provide an electronic database of participating schools and individuals, vision screening, eye examination, refractive correction, dispensing and referral data. Data may be entered offline at the school or hospital location, without dependence on internet access. The software was also used to monitor programme progress and to generate reports to aid management.
REACH common guidelines and screening protocol
Senior paediatric ophthalmologists and optometrists from the six hospitals developed the REACH protocol and guidelines common to all processes and personnel. Clinical evaluation and counselling were not standardised.
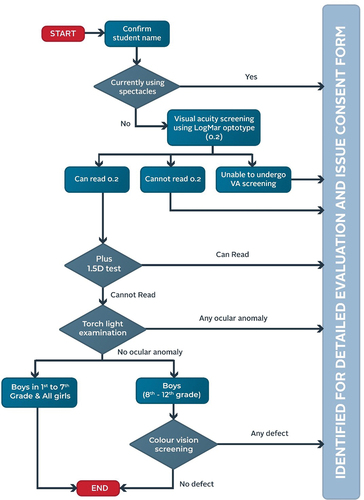
Primary screening protocol
REACH vision screening was conducted using a pocket vision screener in a room with at least 4 m dimensions and moderate ambient illumination.Citation20 Briefly, this method involves presentation of Sloan letters at 0.2 logMAR in three rows of seven viewed monocularly at 3 m first unaided then through a + 1.50D lens (in a pair of spectacles with this power right and left, and with the fellow eye occluded) which relaxes accommodation to identify latent hyperopic errors. The pocket vision screener allows rapid visual acuity screening and has high positive and negative predictive values compared with a standard logMAR chart.Citation20 Each child was instructed to read the letters in the centre row (crowded by the upper and lower rows) and if any three of the central five letters in that line were read correctly the test was passed. These tests were followed by a torch light external eye examination for detection of media opacity, pupillary defects or strabismus.
All children unable to read the letters monocularly, able to read them through a + 1.50D lens, currently wearing spectacles, with an ocular complaint and/or with a sign of external eye abnormality failed the screening and were referred for detailed evaluation. All those who passed returned to their classrooms. An overview of the REACH screening procedure is provided in and the primary screening process is shown in .
Detailed evaluation
Detailed evaluation was conducted at the school by a qualified optometrist, ophthalmic technician or trained vision technician. Primary screening and detailed evaluation were conducted on the same day if possible, but in large schools this was not feasible and they took place on two or more separate days. For children already wearing spectacles, their lenses were measured using a lensometer. Habitual vision was measured monocularly, unaided or with existing spectacles (presenting vision), as appropriate.
Objective refraction (streak retinoscopy) was conducted before monocular subjective refraction using an internally illuminated logMAR chart and including verification of cylindrical axis and power with the aim of attaining acuity of at least 0.0 logMAR. A spot vision screener (Welch Allen, Hillrom, Skaneateles Falls, New York, US) was used in some cases, such as unclear retinoscopy reflex and/or subjective responses, to verify refractive error.Citation21
Accommodative lag was measured using the monocular estimation method of dynamic retinoscopy. Colour vision was tested only in boys at 8th to 12th grade (younger children particularly in rural areas had difficulty completing this test) binocularly using an Ishihara test and cover-uncover and alternating cover tests were used to screen for ocular deviations. The final refractive error was based on streak retinoscopy and subjective responses using the logMAR chart, any reported symptoms, and other factors, such as accommodative lag or ocular deviation.
Torch light examination was repeated to look for anterior segment anomalies. Direct ophthalmoscopy was performed on all children whose corrected acuity in either eye did not improve beyond 0.2 logMAR. Children and their teachers were asked to report any asthenopia symptoms, such as headache, or vision-related symptoms, such as difficulty seeing objects in the classroom.
Cycloplegic retinoscopy was conducted in cases meeting the following criteria: ocular deviation in a child already wearing spectacles or who failed pocked vision screening; hyperopia with asthenopia; >2.00D change from existing correction; fluctuating acuity or retinoscopy results; >0.75D difference between retinoscopy and subjective refraction in myopia; and >1.00D dynamic retinoscopy lag. Clinicians also considered other factors (such as change in astigmatic power or axis) on an individual basis.
Any children requiring cycloplegia, those with apparent ocular disease or other conditions requiring further evaluation (such as low vision, high myopia, strabismus or nystagmus), children with unconfirmed refractive errors, confirmed colour vision deficiencies requiring career counselling, and children with special needs (with no detailed examination in the last 2 years) were referred to the relevant partner hospital.
Spectacles were prescribed if refraction exceeded the levels specified in the common guidelines ().Citation22 Other levels of refractive error were corrected in children with relevant signs or symptoms and the final refraction was dependent on subjective acceptance. To allow for tonus, 1.00D was deducted from the spherical element of hyperopic cycloplegic refractive errors.Citation22
Table 3. Spectacle prescribing criteria by age group.
Spectacle delivery
Spectacles were provided free of cost. On collection, one of the students was asked to read aloud to the group from one of the IEC materialsCitation19 – a book – to convey to children how their everyday life may be improved by wearing spectacles.
Compliance
To encourage compliance,Citation23 children chose their frames from a wide range. Interpupillary distance was measured using a pupillometer and all details were recorded in REACHSoft. Frame fit was checked by the optician before glazing, and again by a trained project team member at spectacle collection. All children who were prescribed spectacles or referred for further evaluation at the hospital were counselled about the need for this action.
A referral card was issued, and children were instructed to hand this to their parents, whose contact details were updated in the REACHSoft system for continuity of follow-up. About 6 months after spectacle delivery, a member of the REACH team visited the school unannounced (only the school principal was aware) to monitor compliance.Citation23 Students were observed in their classrooms and those wearing their spectacles were asked about the number of hours of daily spectacle use, when and for what purpose(s) they were worn. Vision was checked monocularly using the pocket vision screener to check that acuity with the spectacles was at least the level achieved at detailed evaluation, and all data were recorded in REACHSoft.
Those not wearing spectacles were asked why and this was again recorded in REACHSoft. Those in whom corrected monocular acuity was poorer than logMAR 0.2 were referred to the partner hospital for further evaluation. Spectacle condition was checked, and any minor adjustments required were made at the school. All children referred to hospital during detailed evaluation and who had not yet reported were identified and reasons were captured. During this visit, screening was also conducted for children who were absent on the day of the previous screening.
Note that the aim of this paper is to describe the programme and its progress to date and compliance data are not reported here.
Annual follow-up
Annual follow-up includes: refraction and spectacle condition assessment in all children who underwent detailed evaluation the previous year; primary screening of newly enrolled children in the current academic year (using the same protocol as described above); all children in 1st grade (who were not present in the previous year); children with visual concerns (self-reported or identified by teachers); and children absent from vision screening during the previous year. Children in 8th and 11th grades are also screened because many children change school at these grades.
Quality assurance
The project manager makes unannounced visits to one randomly selected screening site and one hospital each quarter to monitor and control quality.
Spectacle frame and prescription details are checked before manufacture and again before the spectacles are provided. Monocular acuities are tested during spectacle delivery and if not at the expected level (as determined at detailed evaluation), the lenses are rechecked and corrected if necessary.
Definitions
The data were classified according to school location (rural or urban, with fewer than or at least 100,000 people per square kilometre, respectively),Citation24 and type (government aided, with funding at least partially from government, or privately funded, with no government funding).
Results
A total of 11,769 schools were invited to participate, and all agreed. Due to scheduling difficulties, primary screening took place in 10,309 (87.6%) of the schools. The number of children enrolled in those schools totalled 2,240,805, of whom 2,024,053 (90.3%) underwent primary screening.
A total of 8.63% (n = 174706) of those screened were referred for detailed evaluation, and the numbers of girls (90877 [52.0%]) and boys (83829 [48.0%]) referred were similar. The reasons for referral included failure to read 0.2 logMAR letters unaided in 49,809 (28.5%); ability to read them with a + 1.50D lens in 1263 (0.7%); self-reported blurred vision in 56,375 (32.3%); and headache in 12,250 (7.0%).
A total of 47,133 (26.9%) children were referred because they were already spectacle wearers, and 17.5% in total for symptoms or signs including eye watering (3.5%), itching (1.6%), red eye (1.3%), abnormal eye movement (0.1%) and others. The categories were not mutually exclusive, so more than one reason could apply to each child. Of the 174,706 referred, 137148 (78.5%) attended detailed evaluation.
A high degree of absenteeism from detailed evaluation when conducted on a separate day explains in part the absence of almost one quarter of referred children from detailed evaluation. Of those who underwent detailed evaluation, 57558 (42.0%) were prescribed new spectacles with a new or changed prescription, 21842 (15.9%) were advised to continue with their existing spectacles, 27621 (20.1%) were referred to the partner hospital, and 4276 (15.5%) attended the hospital. These data indicate 78% children who were referred and underwent evaluation did in fact require spectacles and/or hospital referral, and a false-positive referral rate of 22%.
REACH screening has been conducted in 2196 (21.3%) urban and 8113 (78.7%) rural schools. Larger numbers of children were enrolled in each urban school, so the absolute numbers screened in urban and rural schools are similar (). Most of the schools (7825; 75.9%) were government-aided, the remainder (2484, 24.1%) being privately funded. The large majority (about 90%) of enrolled children in each type of school underwent primary screening, and between 5.9% and 11.8% (with variation between school locations and types) were referred for detailed evaluation.
Table 4. Numbers (N) of boys and girls who were enrolled in schools covered in the REACH programme, those who completed screening, were referred for detailed evaluation and who underwent that evaluation. Note that the total N in the right-hand column includes 21,842 children who were existing spectacle users and were issued with an unchanged prescription and advised to continue to wear the same spectacles.
The few school children who did not attend screening were absent from school on the day screening took place. A significantly higher proportion of children in private schools and in urban locations were referred for detailed evaluation than in government-funded schools or in rural locations (Test of proportions p < 0.001, ). False-positive rates of referral differed between private and government-funded schools (20.5% and 24.1% respectively; p < 0.001) and between urban and rural schools (24.5% and 19.2%, respectively; p = 0.025).
REACH included 607 schools in Kerala (5.9% of the total 10,309 Schools), 2389 (23.2%) in Madhya Pradesh, 2755 (26.7%) in Maharashtra, 3529 (34.2%) in Tamil Nadu and 1029 (10.0%) in West Bengal. While similarly high proportions of children at schools in each of the five states underwent screening (from 87.2% in Madhya Pradesh to 93.9% in Maharashtra), the proportion referred for detailed evaluation differed by state (p < 0.001), ranging from 4.0% in West Bengal to 14.4% in Kerala. Since all children who were wearing spectacles or were unable to read logMAR 0.2 letters monocularly or were able to read them through a + 1.50D lens were referred, this result indicates that the need for refractive correction or other ocular treatment in children varies substantially between states across India.
Discussion
REACH is a large-scale school eye health model, which uses a standardised uniform approach across multiple locations in India. This model facilitates access to comprehensive eye examinations where necessary, incorporates annual eye checks for each child and strategies to encourage spectacle compliance. Children who need refractive correction or other intervention are likely to receive them since detailed evaluation, dispensing and hospital referral are embedded into the model.
Good vision during childhood is important. Reduced vision may prevent the participation of children in activities at school and home, limit their academic potential and may cause visual deficits which persist throughout life.Citation25,Citation26 Previous research indicates that between 3% and 5% of school children in India have uncorrected refractive error,Citation27 representing large numbers of children who may be disadvantaged. Effective vision screening during the school years is therefore vital, as is widely acknowledged.Citation28 School vision screening, which incorporates strategies such as frame choice and IEC material results in significantly higher compliance with spectacles and referral compared to programmes without these featuresCitation23 illustrating the importance of such strategies
REACH school vision screening is conducted by trained personnel, minimising the variability that has been identified in vision screening by teachers.Citation29 Detailed evaluations are conducted within schools by trained personnel including optometrists. Spectacle dispensing was also conducted in the school, facilitating access to refractive correction. In any screening programme of this kind, some of the children will be referred externally for further examination and management; however, barriers may reduce referral compliance, with potential implications for ocular or systemic health.
Previous research has found that referral compliance depends on screeners having spoken with parents about eye- and vision-related problems.Citation30 In the present study, external referral was to a partner hospital and uptake was checked by personnel working with the school and hospital, and at follow-up, to maximise referral compliance. The use of REACHSoft enhances data security and accessibility, facilitating analysis and report generation. The lack of reliance on Internet access has clear advantages in the field.
More than one-fifth (22%) of children who attended detailed evaluation were not prescribed spectacles or referred to the partner hospital. This false-positive rate was significantly higher in urban than rural schools and in government-funded than private schools. False positives may reflect the fact that any self-reported complaint by children (such as headache or eye watering) triggered a referral for detailed evaluation. The relatively high false positives in urban or government-funded schools than in private or rural schools suggest that children in the former schools experienced symptoms of this kind without ocular anomalies, such as refractive error or ocular pathology. For example, symptoms may be related to pollution or other environmental factors.
Since implementation of the REACH programme, a realist evaluation has been conducted to determine the extent to which it has achieved its intended outcomes of accessible, high quality, comprehensive eye care services for children with good fidelity and availability.Citation31 Semi-structured interviews were conducted with team members to understand successes and challenges, and to make recommendations for programme enhancement. They found the following:
Feasibility of school-based eye care provision could be improved by including government officials in the stakeholder group;
Knowledge exchange or ‘common educational’ forums with school staff and students, project team and community members could encourage more participation;
The advantages of REACHSoft and related IT support were recognised by team members, and recommendations were made for training and quality control measures;
A limitation of the REACH model is that it is resource-intensive, with the trained teams visiting each school more than once to conduct screening and annual follow ups. These funding challenges were highlighted, and the need for supplementary external funding was recognised.
Strengths and limitations
The current REACH database provides a rich source of information about prevalence and age-related progression of refractive errors in school going children. Ongoing analysis will examine any associations between a range of factors and prevalence of myopia, uptake of detailed evaluation and spectacle compliance. However, the study reported here has some limitations. First, it did not conduct detailed evaluation in children who passed screening so cannot gauge false negatives in this programme. Second, during primary screening the +1.50D lenses were left in place for only a few seconds. It is possible that latent hyperopia was not fully relaxed during this period, and that some children with uncorrected hyperopia passed vision screening.
Conclusion
The REACH model for child eye health delivery aims to address challenges in the existing model of vision screening and eye health in school children, to provide evidence for future interventions, and to build and test an innovative programme model. Ongoing development will ensure that this programme is sustainable and scalable.
Acknowledgements
In addition to the named authors, the REACH Research group includes: Varun Agiwal, Hunter Cherwek, Sahithya Bhaskaran, Rishi Raj Borah, Nathan Congdon, Kuldeep Dole, Elizabeth Joseph, Saara Krishnamurthy, Subeesh Kuyyadiyil, Anuradha Narayanan, Pravin Narwadkar, Hira Pant, Mary Sebastian Parappuram, and Vijayalakshmi Perumalsamy.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol. 2012;60:432–437.
- Dandona R, Dandona L, Srinivas M, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–622.
- Murthy GVS, Gupta SK, Ellwein LB, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43:623–631.
- Kulp MT, Ciner E, Maguire M, et al. Uncorrected hyperopia and preschool early literacy: results of the Vision in Preschoolers-Hyperopia in Preschoolers (VIP-HIP) study. Ophthalmology. 2016;123:681–689.
- Bruce A, Kelly B, Chambers B, et al. The effect of adherence to spectacle wear on early developing literacy: a longitudinal study based in a large multiethnic city, Bradford, UK. BMJ Open. 2018;8:e021277.
- Burnett AM, Yashadhana A, Lee L, et al. Interventions to improve school-based eye-care services in low- and middle-income countries: a systematic review. Bull World Health Organ. 2018;96:682–694.
- Evans JR, Morjaria P, Powell C Vision screening for correctable visual acuity deficits in school-age children and adolescents. Cochrane Database Syst Rev. 2018;2:CD005023–CD.
- Gogate P, Mukhopadhyaya D, Mahadik A, et al. Spectacle compliance amongst rural secondary school children in Pune district, India. Indian J Ophthalmol. 2013;61:8–12.
- Gajiwala UR, Patel RU, Sudhan A, et al. Compliance of spectacle wear among school children. Indian J Ophthalmol. 2021;69:1376–1380.
- von-Bischhoffshausen FB, Munoz B, Riquelme A, et al. Spectacle-wear compliance in school children in Conception Chile. Ophthalmic Epidemiol. 2014;21:362–369.
- Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health commission on global eye health: vision beyond 2020. Lancet. 2021;9:e489–551.
- Sharma A, Congdon N, Patel M, et al. School-based approaches to the correction of refractive error in children. Surv Ophthalmol. 2012;57:272–283.
- Muralidhar R, Vijayalakshmi P. Sensitivity and specificity of teachers for vision screening among primary school children in South India. Oman J Ophthalmol. 2019;12:88–93.
- Dole KS, Deshpande AS, Deshpande MD, et al. Comparative evaluation of qualitative performance of technical human resource in school eye health program. Indian J Ophthalmol. 2021;69:123–126.
- Jose R, Sachdeva S. School eye screening and the national program for control of blindness. Indian Pediatr. 2009;46:205–208.
- Vision 2020 vision screening in school children manual. [cited 2022 July 19]. Available from: vision2020india.org
- National programme for the control of blindness and visual impairment. [cited 2022 Apr 26]. Available from: https://npcbvi.gov.in/Home
- Orbis International. [cited 2022 Apr 26]. Available from: https://gbr.orbis.org/
- Orbis international resources ‘The singing tree’. [cited 2022 Jan 26]. Available from: https://ind.orbis.org/en/what-we-do/resources/
- Raja M, Ramamurthy D, Srinivasan K, et al. Development of pocket vision screener and its effectiveness at screening visual acuity deficits. Indian J Ophthalmol. 2014;62:1152–1155.
- Pandhy D, Bharadwaj SR, Nayak S, et al. Does the accuracy and repeatability of refractive error estimates depend on the measurement principle of autorefractors? Transl Vis Sci Technol. 2021;10:2.
- Leat SJ. To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Clin Exp Optom. 2011;94:514–527.
- Narayanan A, Ramani KK. Effectiveness of interventions in improving compliance to spectacle wear and referral in school vision screening. Clin Exp Optom. 2018;101:752–757.
- Census India. [cited 2022 Mar 30]. Available from: https://censusindia.gov.in/pca/pcadata/pca.html
- Vision Impact Institute. The impact of uncorrected refractive error on children: a systematic review. [cited 2022 Jul 19]. Available from: https://www.visionimpactinstitute.org/research/the-impact-of-uncorrected-refractive-error-on-children%3A-a-systematic-review
- Taylor K, Powell C, Hatt SR, et al. Interventions for unilateral and bilateral refractive amblyopia. Cochrane Database Syst Rev. 2012. DOI:10.1002/14651858.CD005137.pub3
- Padhye AS, Khandekar R, Dharmadhikari S, et al. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol. 2009;16:69–74.
- Unite for Sight. [cited 2022 Jan 26]. Available from: https://www.uniteforsight.org/eye-health-teachers/importance-vision-screening-for-children
- Marmamula S, Khanna RC, Mettla AL, et al. Agreement and diagnostic accuracy of vision screening in children by teachers, community eye‐health workers and vision technicians. Clin Exp Optom. 2018;101:553–559.
- Priya A, Veena K, Thulasiraj R, et al. Vision screening by teachers in Southern Indian schools: testing a new ‘All class teacher’ model. Ophthal Epidemiol. 2015;22:60–65.
- Seelam B, Liu H, Borah RR, et al. The REACH research group. A realist evaluation of the implementation of a large-scale school eye health programme in India: a qualitative study. Ophthalmic Physiol Opt. 2021;41:565–581.