ABSTRACT
Optometrists play an integral role in primary eyecare services, including prevention, diagnosis, and management of acute and chronic eye conditions. Therefore, it remains essential that the care they provide be timely and appropriate to ensure the best patient outcomes and optimal utilisation of resources. However, optometrists continuously face many challenges that can affect their ability to provide appropriate care (i.e., the care in line with evidence-based clinical practice guidelines). To address any resulting evidence-to-practice gaps, programs are needed that support and enable optometrists to adopt and utilise the best evidence in clinical practice. Implementation science is a field of research that can be applied to improving the adoption and maintenance of evidence-based practices in routine care, through systematic development and application of strategies or interventions to address barriers to evidence-based practice. This paper demonstrates an approach using implementation science to enhance optometric eyecare delivery. A brief overview of the methods used to identify existing gaps in appropriate eyecare delivery is presented. An outline of the process used to understand the behavioural barriers responsible for such gaps follows, involving theoretical models and frameworks. The resulting development of an online program for optometrists to enhance their capability, motivation, and opportunity to provide evidence-based eyecare is described, using the Behaviour Change Model and co-design methods. The importance of and methods used in evaluating such programs are also discussed. Finally, reflections on the experience and key learnings from the project are shared. While the paper focuses on experiences in improving glaucoma and diabetic eyecare in the Australian optometry context, this approach can be adapted to other conditions and contexts.
Introduction
Chronic eye conditions, including glaucoma, diabetic retinopathy, age-related macular degeneration, and dry eye, pose a significant burden to health systems.Citation1 Timely and appropriate diagnosis and ongoing management of such eye conditions are desirable as they can significantly reduce disease burden and improve quality of life and vision.Citation1 Provision of appropriate care, such as adhering to evidence-based guidelines, helps to improve patient outcomes and lessen health expenditure.Citation2–4
However, optometrists experience a wide range of context-specific barriers located at both the practitioner level (for example, beliefs and skill proficiency deficits) and organisational level (for example, lack of time and resources) that can affect their ability to provide evidence-based care in routine clinical practice.Citation5 This divergence or tension between best evidence and clinical practice, known as the evidence-to-practice gap, is of concern as the care patients receive may not be sufficient or fit for their needs, resulting in sub-optimal outcomes.Citation6
To overcome evidence-to-practice gaps, campaigns, initiatives, and programs should be implemented that support the use of best evidence and appropriate care in clinical practice. However, interventions aimed at improving the appropriateness of healthcare delivery often have modest or variable effects on changing health practitioner behaviour.Citation7–9 The limited success of these interventions has been attributed to a lack of theoretical basis for the strategies and activities employed to modify practitioner behaviour.Citation10,Citation11 Intervention effectiveness is increased when well-defined and appropriately targeted behaviour change techniques are used.Citation12
Implementation science, a field of research that can be applied to improving the adoption and maintenance of evidence-based practices in routine care, arose to overcome the trial-and-error approach commonly used in designing research translation strategies.Citation13 The theories, models, and frameworks of implementation science assist in understanding the underlying issues and behaviours that require modifying, guiding the process of translating knowledge into practice, helping select methods most suited to achieving the desired behaviour, and providing a framework to evaluate the success of the implementation.Citation14
The iCareTrack project, led by a multidisciplinary team at the School of Optometry and Vision Science, UNSW Sydney, focuses on improving the uptake of evidence-based eyecare practice. This paper presents a data-led approach used in the iCareTrack project that combined the principles of implementation science and behaviour change to develop an intervention to support optometrists in delivering appropriate eyecare. The aim is to demonstrate the application of an implementation science approach in developing an intervention program in eyecare service delivery, rather than to present a comprehensive report of the project.
The approach described involves a cycle of 1. gap identification, 2. intervention development and 3. evaluation of the intervention (). The research team has used the approach described in to develop improvement interventions for glaucoma and diabetic eye disease so far, and these are presented as examples in this paper. However, the approach could be adapted to any other eye or health conditions. Comprehensive results of the intervention development and evaluation will be published separately. It is expected that this high-level description of the process (and challenges faced and lesson learnt) will be useful to eyecare researchers and readers novice to the field of implementation science in preparation for a similar journey.
Figure 1. Overview of the iCaretrack approach demonstrating the key steps. The process starts with identifying the existing gaps (step A) and analysing the underlying behavioural determinants (step B), followed by developing an intervention using theory and centring around the end-user needs (step C), evaluating the intervention (step D) and finally scaling up the effective interventions (step E) for broader public health impact.

Identifying the gap
Measuring the size of the existing gap in evidence-based eyecare services is an important first step towards enhancing care delivery (Step A in ). As leading causes of irreversible, yet preventable vision loss in Australia, glaucoma and diabetic eye disease are significant public health concernsCitation15 and thus were chosen as the focus of the iCareTrack study. The iCareTrack study established the appropriateness of glaucoma and diabetic eyecare delivery by auditing randomly sampled clinical records (420 per condition) in a nationally representative sample of 42 Australian optometry practices.Citation16
Care was assessed against evidence-based clinical indicators (38 glaucoma and 15 diabetes), which are the measurable components of guideline recommendations.Citation17 These clinical indicators were derived from evidence-based guidelines and refined by experts using a Delphi process. For each condition, the clinical indicators were stratified into consultation domains of history taking, physical examination, recall, and referral.
Care was delivered appropriately in 63% and 69% of patient encounters for glaucoma and diabetic eyecare, respectively.Citation16 In general, care was delivered at higher appropriateness for recall and referral domains, compared to history taking and physical examinations for glaucoma and diabetic eye disease ().Citation18,Citation19
Table 1. Appropriateness levels for glaucoma and diabetic eyecare for consultation domains and overall care.Citation16,Citation18,Citation19.
Australian optometrists delivered key aspects of glaucoma and diabetic eyecare at high appropriateness levels. For example, optometrists appropriately performed intraocular pressure measurement (90%) and imaging of the optic nerve head and retinal nerve fibre layers (78%) for glaucoma care.Citation18 Similarly, they referred people with suspected diabetic macular oedema or proliferative diabetic retinopathy (100%) for secondary care.Citation19 However, pockets of sub-optimal care for specific aspects of history taking and physical examinations for both conditions existed. For history taking, these gaps in care were related to risk factor identifications such as ethnicity (0%), steroid use (2%), low blood pressure status (2%) for glaucoma,Citation18 and duration of diabetes (43%) and blood glucose control (47%) for diabetes.Citation19 Gaps in care were observed for physical examinations, such as assessment of the peripheral anterior chamber by gonioscopy or van Herick’s and visual field assessment by standard automated perimetry for glaucoma and dilated fundus examination and iris examination for diabetic eyecare.Citation18,Citation19
These results indicate a potential divergence in several aspects of glaucoma and diabetic eyecare delivery compared to guideline recommendations. This divergence should be further explored to understand the underlying reasons, and efforts made to address these gaps to enhance evidence-based eyecare delivered by optometrists in Australia.
Intervention development
To develop the intervention program, the iCareTrack approach used a combination of two main design approaches: evidence and theory-based design and participatory design (co-design process).Citation20 Evidence and theory-based design process utilises either published research evidence or formal theories to design the intervention.Citation20 The Behaviour Change Wheel (BCW) framework provided the theoretical underpinning for the quality improvement program and was used to select components of the conceptual intervention strategy (see subsection 2.1).Citation21
Participatory design, which involves end-users and stakeholders in the design process, ensures that the resultant program is appropriate to their needs.Citation20 Thus, the intervention development process involved understanding the underlying causes for the identified gaps (through a behavioural analysis) (Step B in ), theoretical mapping and intervention conceptualisation, participatory design, and refinement of prototype intervention (Step C in ). The following sections describe the process with examples from the diabetes module.
Behavioural analysis
Having established the gaps in care delivery and made the case for improving the care delivered, the next step consisted of identifying what needed to change in the optometrists and/or their environment to achieve the desired change in behaviour for optimal care delivery. An accurate understanding of the target behaviour and behavioural determinants (barriers and enablers) in context (i.e., the setting in which the implementation will occur) is likely to result in an effective intervention.Citation22 Using the implementation science theories, models and frameworks helps in rigorous behavioural analysis and intervention design.Citation14,Citation23
The iCareTrack approach uses the BCW model for intervention design. This widely used model incorporates elements of 19 behaviour change frameworks into a single comprehensive and coherent tool, linked to an overarching model of behaviour: the COM-B model.Citation21 The COM-B model explains the source of behaviour and identifies the capability (C), opportunity (O), and motivation (M) as the main drivers of behaviour (B). The BCW model links these sources of behaviour to appropriate intervention options.
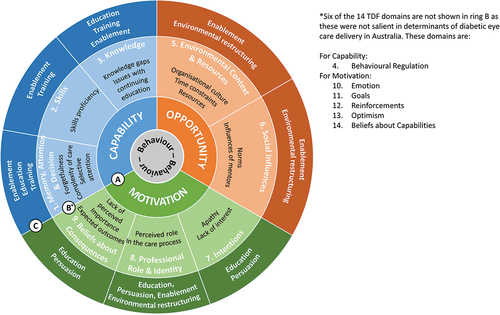
For a more granular understanding of the behaviour, another framework known as the Theoretical Domains Framework (TDF) was used during the behavioural analysis. TDF is an established method to understand the determinants influencing the uptake of evidence-based clinical recommendations of health professionals and has been used in various settings, including eye care delivery.Citation24–28 The TDF consists of 14 domains (see ring B in ), which can be mapped to the COM-B components (ring A in ) in the BCW model.Citation22,Citation29
Figure 2. The Theoretical Domains Framework (TDF) and Behaviour Change Wheel (including COM-B) model used for behavioural analysis and intervention conceptualisation in the iCaretrack approach. The eight salient TDF domains (ring B) are linked to COM-B (ring A). The intervention functions most likely to address these determinants are outlined in ring C (step 1 described in the text). The selected intervention functions need to be further explored to identify the behaviour change techniques (not shown in the figure) which are the core ingredients in an intervention (step 2 described in the text). The BCW model also includes an outermost ring of seven policy categories (not shown in the figure) that support the implementation of the selected intervention functions.
A qualitative study (focus group discussion and interviews) was conducted to explore barriers and enablers experienced by optometrists when providing diabetic eyecare. This study helped to identify what needed to be modified at the individual, group, or organisational level to optimise care delivery.Citation18,Citation30
The study participants were informed about the gaps identified (section 1) and then asked about the perceived barriers and enablers to appropriate history taking and physical examination for diabetic eyecare. The responses of the participants were classified as barriers or enablers and coded to appropriate TDF domain(s).Citation29 Salient domains () were identified as those with high coding frequency and deemed important (as expressed by participants or judged by investigators based on the strength, intensity, passion, or sentiment of the beliefs of participants).Citation31–33
Table 2. Key determinant themes (barriers and enablers) grouped in COM-B components with examples.
The study suggested that at the individual level, optometrists should be supported to enhance their capability by acting on their knowledge, and information processing. At practice level, a supportive work environment, including longer consultation time, support staffs and resources, and a positive organisational culture, would enable optometrists to deliver appropriate care. Higher level system-wide changes, including incentives, were also needed to support and engage optometrists in providing comprehensive and appropriate care. Thus, a need to develop a multifaceted tailored intervention program to address individual as well as external contextual determinants of optometrists for appropriate eyecare delivery was recognised.
Designing the conceptual intervention strategy
With the determinants for appropriate care delivery identified, the next step involved designing an intervention that addressed these behavioural determinants. Linking the determinants to behaviour change techniques engenders a selection of effective techniques to support optometrists in overcoming barriers or harnessing enablers.Citation22 Once the generic behaviour change techniques are chosen, they can be further developed to specify the content (what is to be delivered), format (how it is set out) and mode of delivery (how it will be delivered)Citation21 while ensuring the end product is acceptable, cost-effective, and implementable.Citation34
A three-step process based on the BCW methodology was used to design the conceptual intervention strategy: step 1: identify and select intervention functions, step 2: identify and select behaviour change techniques, and step 3: adapt behaviour change activities to the context and combine to develop a conceptual intervention strategy.
In step one, salient TDF domains identified in the Behavioural Analysis stage were mapped to the COM-B from the BCW model to identify candidate intervention functions that represent the broad categories of intervention likely to bring about behaviour change (i.e., linking ring B to ring C in ).Citation21,Citation35 The intervention functions were then selected based on the frequency to which they were mapped and their suitability for modifying behaviour within the context of the research and optometry in Australia using the APEASE (affordability, practicability, effectiveness or cost-effectiveness, side effects and safety, and equity) criteria.Citation21 The intervention functions identified through this process were ‘enablement’, ‘environmental restructuring’, ‘persuasion’, ‘education’, and ‘training’.
In step two, the selected intervention functions were mapped to the Behaviour Change Taxonomy to identify candidate behaviour change techniques (not shown in ). The Behaviour Change Taxonomy is a comprehensive list of 93 defined behaviour change techniques, such as goal setting or action planning, which are the active ingredients of behaviour change interventions.Citation36,Citation37 The most suitable behaviour change techniques for the context were selected based on the frequency of reported use in the literature and APEASE assessment.
In step three, the selected behaviour change techniques were combined and adapted to the context of optometrists and optometry practice in Australia. For example, the behaviour change techniques of goal setting, self-monitoring of outcomes of behaviour, feedback on outcomes of behaviour and social comparison constituted the conceptual intervention activity of audit and feedback with benchmarking.
The resulting conceptual intervention strategy included various behaviour change activities that were likely to be successful in enhancing care delivery in the context described above.
This scope of the project was limited to addressing individual behavioural determinants to enable optometrists (rather than changing the practice environment, system or policy) to provide appropriate eyecare. Thus, the potential intervention components targeting optometry practices and policies were not explored in this study. For intervention designers with no or limited policy access, the BCW model developers recommend a flexible approach allowing skipping the policy mapping step.Citation22,Citation38,Citation39 If the policy-level changes are of interest or within the study scope, the intervention functions can be further mapped to identify the policy categories (guidelines, regulations, legislation, fiscal measures, service provision, communication/marketing, and environmental/social planning) that can be tapped to support the implementation of the behaviour change activities.Citation21
Participatory design (co-design) of the program
During the participatory design stage, a combination of workshops and interviews with optometrists, patients, and stakeholders (including Optometry Australia, patient advocacy groups, ophthalmologists, and optometry corporate groups) were used to explore and refine the conceptual intervention strategies. Co-design is a participatory design method in which end-users and stakeholders partner with researchers or designers to jointly analyse problems and create solutions.Citation40 It leverages the unique knowledge and experience of end-users in the design process to develop a product or service that is most suitable to the needs of end-users.
The participatory design stage was guided by a commonly used co-design model comprising six elements (engage, plan, explore, develop, decide, and change) that can be used sequentially, simultaneously or discretely (Supplementary 1).Citation41 The co-design process involved program development and program prototype refinement stages. The program development stage comprised two sequential workshops with optometrists and stakeholders and semi-structured interviews with patients. Participants were briefed on the results from earlier phases of the study, including the gaps identified and barriers explored before and during workshops and interviews. Both workshops used the elements of ‘explore’, ‘develop’, and ‘decide’ from the co-design model and co-creation activities adapted from the business world ().Citation42 In addition, patient interviews uncovered perspectives of patients regarding appropriate glaucoma and diabetic eyecare delivery that were included in the intervention. The results from the workshops and interviews were qualitatively analysed to determine feasibility within the research scope and then combined with the conceptual intervention strategies to develop the conceptual quality improvement program.
Table 3. Overview of the co-design workshops with optometrists and stakeholders.
A working prototype of the conceptual quality improvement program was developed and then refined iteratively during the program prototype refinement stage. Detailed user feedback on the usability and functionality of the program was obtained through the ‘think-aloud’ approach and semi-structured interviews with optometrists. In the think-aloud approach, optometrists were instructed to verbalise their thoughts while completing different tasks of the quality improvement program.Citation43 At the completion of tasks, overall impressions of optometrists were gained through semi-structured post-task interviews, where they were asked about their experience and suggestions to improve the program components. The quality improvement program was modified based on the feedback received.
A summary of the steps, methods, and outcomes in the design of intervention with examples from the diabetes module is presented in .
Table 4. Outline of steps involved in the intervention development process with examples from the diabetes module.
Quality improvement program overview
The resultant quality improvement program comprises a clinical self-assessment tool, peer support activities, educational activities, and resources that are delivered via a secure web portal (). The hub of the program is the iCareTrack Assessment of appropriateness Clinical pracTice (i-ACT) tool.
Figure 3. iCaretrack quality improvement program and its components for diabetes module. The glaucoma eyecare module had a similar layout and presentation. The focus of the program was the i-ACT (iCaretrack: assessment of appropriateness in Clinical pracTice) dashboard. Other supporting components included education (lectures and case studies); resources (a curated list of resources developed by the research team as well as links to external resources), and peer support activities (webinars and discussion forums).
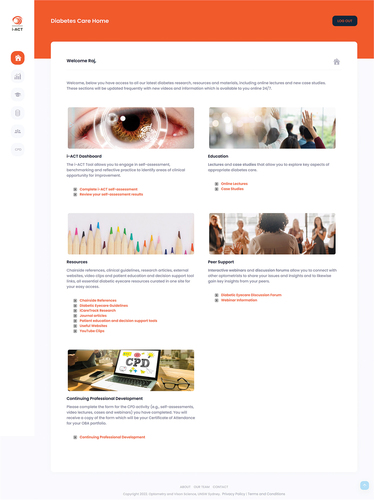
The i-ACT tool is a clinical self-assessment that consists of 45 and 32 clinical indicators for glaucoma and diabetic eyecare, respectively. The clinical indicators are stratified by the consultation domains of history taking, physical examinations, management, recall and referral, and education and communication. The i-ACT tool allows optometrists to assess several patient records for either glaucoma or diabetic patients in self-assessment cycles. At the end of each self-assessment cycle, the i-ACT dashboard allows optometrists to visualise their performance compared to national benchmarks (). The final element of the self-assessment involves self-reflection and improvement goal setting.
Figure 4. Diabetes i-ACT (iCaretrack: assessment of appropriateness in Clinical pracTice) dashboard for optometrists. The glaucoma dashboard had a similar layout and presentation.

Implementing the program is likely to be facilitated by recent changes to the continued professional development (CPD) requirements for registration set by the Optometry Board of Australia. The updated CPD guidance encourages optometrists to engage in planning and reflection for effective learning through various activities, including ‘clinical audit or review of records’.Citation44 While new to the Australian optometry as a professional development activity,Citation44,Citation45 self-assessment is a widely accepted part of educational or CPD programs in medicine and healthcare.Citation46,Citation47 Self-assessment and reflection (and all other activities included in the program) can be logged into the Optometry Board of Australia’s CPD portfolios of optometrists.
Evaluation
Evaluation is an important aspect of any implementation project as it informs if and shows how the interventions worked and helps explore the experiences of recipients and stakeholders. Two key aspects of evaluation are quality (process evaluation) and success (outcome evaluation) of intervention.Citation48,Citation49 Process evaluation focuses on the functioning of an intervention, examines fidelity (i.e., the extent to which the intervention is implemented as intended) and explores the mechanisms of change and associated contextual factors.Citation48,Citation49 Basic examples of process evaluation include assessing the completion rates for self-assessment cycles and examining the cost and time required to deliver the program. Outcome evaluation examines the effectiveness of the intervention in achieving its goal; for example, the impact of an educational program in increasing the rate of dilated fundus examination in patients with diabetes.Citation50
The evaluation phase (Step D in ) in the iCareTrack study involves a cluster randomised controlled trial. In the ongoing cluster randomised controlled trial (ACTRN12622000076774), optometry practices (clusters) are randomly allocated to intervention (use of the i-ACT tool and other intervention components for 3 months) and control (no intervention).
The effectiveness (outcome evaluation) of the intervention is measured through a retrospective record card review using relevant diabetic eyecare clinical indicators before and after the intervention period.Citation16 The process evaluation involves a mixed-method approach (qualitative interviews and quantitative data collection). The data collection for feasibility and fidelity of intervention is guided by the framework of Proctor (Supplementary 2).Citation51
Next steps: implement change and scale up
If shown to be effective, the intervention can then be delivered at scale to achieve better health benefits at the population level. Scaling up is a process of expanding the health interventions or programs shown to be efficacious in controlled settings to broader practice (or policy) in real-world conditions.Citation52 Implementation (integrating evidence-based intervention in routine practice) and scaling up (expansion to wider practice and policy) are part of a “program life cycle” that includes development, implementation, maintenance, and scaling up of the intervention.Citation53 Unlike routine adoption of evidence in practice, which is a passive and slow process, the scaling up is an active process with systematic strategies with the explicit intent of expanding the intervention to new settings or populations.Citation54
Once the effectiveness of the program is established, its coverage will be expanded to reach practising Australian optometrists and transfer the control for program delivery from the research team to local stakeholders or institutions (for example, Optometry Australia) (Step E in ).Citation55 The process will begin with a scalability assessment of the intervention and then the development of a scale-up plan, securing resources and preparing for scaling up, and finally scaling up the intervention based on the developed plan.Citation56,Citation57
Lessons learnt
Several important lessons were learned through developing the quality improvement program underpinned by theory and co-designed with key stakeholders. Examples of such included that there were challenges and benefits in the use of the TDF and BCW model; the barriers and facilitators uncovered were diverse with a combination of expected and novel determinants unearthed; that while co-design was beneficial to user acceptability of the intervention, it was a labour-intensive process with limited guides to its practical application; and that co-design can generate ideas that are outside the scope and feasibility of projects.
Many theories, models, and frameworks developed across a range of disciplines exist, and these have been used to varying extents in implementation science.Citation14 The large number of frameworks and limited guidance make it challenging to select and use the most appropriate framework to address the relevant research question.Citation58,Citation59 Reviews of implementation frameworks,Citation14,Citation23 tools, such as Theory Comparison and Selection Tool (T-CaST),Citation60 websites (such as https://dissemination-implementation.org/index.aspx) and published guidanceCitation58,Citation59 can be valuable resources in identifying and selecting suitable theories and frameworks.
Similarly, selecting behaviour change techniques can be challenging due to the sheer number of techniques available.Citation36,Citation61 To overcome this issue and guide intervention design, a systematic approach comprising a behaviour change theory, linking behavioural determinants to behaviour change techniques using theory, and user engagement should be employed.Citation62
Using the TDF and BCW models was challenging due to the time required to understand and utilise these models appropriately in the research. In addition, coding data to the TDF was complicated by a lack of clear operational definitions and examples for the domains, an issue noted by other researchers.Citation63 This issue was overcome by creating a coding manual with optometry-specific examples for each domain to guide coding and through robust discussion among the research team to ensure the validity of the coding decisions. Ultimately, the use of the TDF instilled confidence in the team that the topic had been thoroughly explored and that no preconceived assumptions of the barriers and enablers were made.
In addition, the use of the TDF helped identify a broad range of barriers and enablers with a combination of expected and novel determinants unearthed. For example, beliefs about consequences, social norms, and issues with memory and attention were novel barriers to glaucoma care not previously uncovered in the literature.Citation18 This strength of the TDF in uncovering a broad perspective of barriers and enablers has been noted previously by researchers involved in a variety of healthcare implementation programs.Citation63
Likewise, while the BCW model helped identify intervention functions most likely to address the determinants effectively, the number of salient determinants identified meant that all intervention functions were possible candidates. This resulted in numerous potential behaviour change activities as candidates that had to be prioritised. Other researchers have previously reported the challenge of prioritising numerous potential intervention functions and behaviour change activities.Citation64 This was overcome in the current context by using a rubric to guide the selection of intervention functions and behaviour change activities based on frequency, pragmatic reasoning, and the APEASE criteria.Citation64 While there were subjective and pragmatic decisions made during this selection process, the research team is confident that a systematic approach and pre-defined rubric to guide decisions resulted in the selection of the most suitable behaviour change activities for the context.
While co-design was a beneficial approach to the design process, it was labour-intensive requiring greater effort than anticipated compared to normal design methods; this was an issue noted by other researchers.Citation65 Thus, a recommendation for further work in this area is to factor in ample time and resources when planning co-design.Citation66 As co-design is a relatively novel approach in healthcare, there was limited guidance on practical applications or the types of activities that should be used in co-design workshops. This required novel approaches, such as utilising well-established co-creation tools sourced from the business world.
The co-design workshop format in this study had to be translated into an online format due to COVID-19-related restrictions. Such translation required several modifications to co-design activities and tools to fit the online environment. This was particularly challenging as few activities have been developed to suit online mode as co-design methods have historically relied on face-to-face engagement.Citation67 Additional challenges included the need for dedicated technical support, disruptions in internet connections, managing online etiquette in a large and diverse group, and the need for enough facilitators to run breakout sessions.
Despite these challenges, the online process has some advantages. Online co-design workshops and interviews have helped overcome geographic barriers to participation and reduce costs associated with travel and organising face-to-face workshops. The growing familiarity and acceptance of the videoconference as a method for general interaction and eyecare delivery may also have positively impacted participant engagement during these workshops and interviews.Citation68–70
Another challenge in the co-design process was creating an environment that allowed participants to generate ideas freely while focusing on feasible ideas within the research context.Citation65 For example, some ideas of participants were outside the scope of the research (e.g., developing living guidelines for glaucoma and diabetic eyecare) or were unfeasible for the research team to achieve (e.g., lobbying for expanded scope of optometry practice). While many of these ideas were not necessarily integrated into the invention, they were nevertheless captured in a document to be shared with Optometry Australia and other stakeholders for further investigation. Thus, the final lesson learnt was that clear research objectives and alignment of stakeholder expectations are required during the set-up phase of co-design.Citation71
Summary
This paper describes a step-by-step approach to identifying existing gaps in appropriate eyecare delivery and developing and evaluating approaches to address such gaps. Through a retrospective patient record audit in optometry practices, this paper demonstrates high levels of appropriate care delivered by optometrists while identifying areas of sub-optimal performance. The underlying determinants (i.e., barriers and enablers) to appropriate glaucoma and diabetic care delivery were then explored using an established behavioural theory. To address these barriers and enablers, an intervention program was designed based on the BCW model and an iterative co-design approach.
The resulting intervention program consists of self-assessment of clinical care (i-ACT tool), education, peer support, and resources. The feasibility, fidelity, and effectiveness of the program are currently being evaluated through a cluster randomised controlled trial among Australian optometry practices. Once the data on effectiveness become available, it is hoped that the intervention program can be appropriately scaled up across Australia.
The approaches and experiences described in this paper can provide direction for researchers, clinicians, policymakers, and other stakeholders interested in understanding and improving care delivery across various healthcare contexts and conditions.
Supplementary 1: Description of the six elements from the co-design model used
Download PDF (102.5 KB)Supplementary 2: Areas of process evaluation (based on Proctor Framework1 and methods of data collection
Download PDF (110.7 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/08164622.2023.2178286
Additional information
Funding
References
- Burton MJ, Ramke J, Marques AP et al. Lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health 2021; 9: e489–551. doi:10.1016/S2214-109X(20)30488-5
- Fritz JM, Cleland JA, Brennan GP. Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Med Care 2007; 45: 973–980. doi:10.1097/MLR.0b013e318070c6cd
- Komajda M, Lapuerta P, Hermans N et al. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. Eur Heart J 2005; 26: 1653–1659. doi:10.1093/eurheartj/ehi251
- Rutten GM, Degen S, Hendriks EJ et al. Adherence to clinical practice guidelines for low back pain in phys ther: do patients benefit? Phys Ther 2010; 90: 1111–1122. doi:10.2522/ptj.20090173
- Toomey M, Gyawali R, Stapleton F et al. Facilitators and barriers to the delivery of eye care by optometrists: a systematic review using the theoretical domains framework. Ophthalmic Physiol Opt 2021; 41: 782–797. doi:10.1111/opo.12801
- McGlynn EA, Asch SM, Adams J et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003; 348: 2635–2645. doi:10.1056/NEJMsa022615
- Ivers N, Jamtvedt G, Flottorp S et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012; doi:10.1002/14651858.CD000259.pub3
- O’brien MA, Rogers S, Jamtvedt G et al. Educational outreach visits: effects on professional practice and heatlh care outcomes. Cochrane Database Syst Rev. 2007 [cited]. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000409.pub2/full.
- Forsetlund L, O’brien MA, Forsén L et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2021; Art No.:CD003030 2021: doi:10.1002/14651858.CD003030.pub3
- Michie S, Johnston M, Abraham C et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005; 14: 26–33. doi:10.1136/qshc.2004.011155
- Sales A, Smith JL, Curran GM et al. Models, strategies, and tools. J Gen Intern Med 2006; 21: S43–49. doi:10.1111/j.1525-1497.2006.00362.x
- Greaves CJ, Sheppard KE, Abraham C et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011; 11: 119. doi:10.1186/1471-2458-11-119
- Eccles MP, Mittman BS. Welcome to Implementation Science. Implementation Sci 2006; 1: 1. doi:10.1186/1748-5908-1-1
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015; 10: 53. doi:10.1186/s13012-015-0242-0
- Keel S, Xie J, Foreman J et al. Prevalence of glaucoma in the Australian national eye health survey. Br J Ophthalmol 2019; 103: 191–195. doi:10.1136/bjophthalmol-2017-311786
- Ho KC, Stapleton F, Wiles L et al. iCaretrack: measuring the appropriateness of eyecare delivery in Australia. Ophthalmic Physiol Opt 2020; 40: 433–441. doi:10.1111/opo.12699
- Runciman WB, Coiera EW, Day RO et al. Towards the delivery of appropriate health care in Australia. Med J Aust 2012; 197: 78–81. doi:10.5694/mja12.10799
- Toomey M, Ho KC, Gyawali R et al. Level of appropriate primary diabetic eyecare delivered and achievable in optometry practices in Australia. Clin Exp Optom 2022; 1–9. doi:10.1080/08164622.2022.2033107
- Gyawali R, Ho KC, Toomey M et al. Level of appropriate primary diabetic eyecare delivered and achievable in optometry practices in Australia. Clin Exp Optom 2022; 1–7.
- O’cathain A, Croot L, Sworn K et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud 2019; 5: 41. doi:10.1186/s40814-019-0425-6
- Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. Great Britain: Sliverback Publishing; 2014.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci 2011; 6: 42. doi:10.1186/1748-5908-6-42
- Tabak RG, Khoong EC, Chambers DA et al. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 2012; 43: 337–350. doi:10.1016/j.amepre.2012.05.024
- Duncan EM, Cassie H, Pooley J et al. Areas for improvement in community optometry: flashes and floaters take priority. Ophthalmic Physiol Opt 2018; 38: 411–421. doi:10.1111/opo.12564
- French SD, Green SE, O’connor DA et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the theoretical domains framework. Implementation Sci 2012; 7: 38. doi:10.1186/1748-5908-7-38
- Graham-Rowe E, Lorencatto F, Lawrenson JG et al. Barriers to and enablers of diabetic retinopathy screening attendance: a systematic review of published and grey literature. Diabet Med 2018; 35: 1308–1319. doi:10.1111/dme.13686
- Dennis S, Reddel HK, Middleton S et al. Barriers and outcomes of an evidence-based approach to diagnosis and management of chronic obstructive pulmonary disease (COPD) in Australia: a qualitative study. Fam Pract 2016; 34: 485–490. doi:10.1093/fampra/cmw103
- Lawrenson JG, Graham-Rowe E, Lorencatto F et al. What works to increase attendance for diabetic retinopathy screening? An evidence synthesis and economic analysis. Health Technol Assess 2018; 22: 1–160. doi:10.3310/hta22290
- Atkins L, Francis J, Islam R et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implementation Sci 2017; 12: 77. doi:10.1186/s13012-017-0605-9
- Gyawali R, Toomey M, Stapleton F et al. Multiple things going on at the same time: determinants of appropriate primary diabetic eyecare delivery. Ophthalmic Physiol Opt 2022; 42: 71–81. doi:10.1111/opo.12912
- Kennie-Kaulbach N, Cormier R, Kits O et al. Influencers on deprescribing practice of primary healthcare providers in nova scotia: an examination using behavior change frameworks. Med Access @ Point Care 2020; 4: 2399202620922507. doi:10.1177/2399202620922507
- McSherry LA, Dombrowski SU, Francis JJ et al. ‘It’s a can of worms’: understanding primary care practitioners’ behaviours in relation to HPV using the theoretical domains framework. Implementation Sci 2012; 7: 73. doi:10.1186/1748-5908-7-73
- Buetow S. Thematic analysis and its reconceptualization as ‘saliency analysis’. J Health Serv Res Policy 2010; 15: 123–125. doi:10.1258/jhsrp.2009.009081
- Skivington K, Matthews L, Simpson SA et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ 2021; 374: 2061. doi:10.1136/bmj.n2061
- Cane J, O’connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci 2012; 7: 37. doi:10.1186/1748-5908-7-37
- Michie S, Richardson M, Johnston M et al. The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for reporting of behaviour change interventions. Ann Behav Med 2013; 46: 81–95. doi:10.1007/s12160-013-9486-6
- Carey RN, Connell LE, Johnston M et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med 2019; 53: 693–707.
- Ekberg K, Timmer B, Schuetz S et al. Use of the behaviour change wheel to design an intervention to improve the implementation of family-centred care in adult audiology services. Int J Audiol 2021; 60: 20–29. doi:10.1080/14992027.2020.1844321
- Wang H, Blake H, Chattopadhyay K. Development of a school-based intervention to increase physical activity levels among Chinese children: a systematic iterative process based on behavior change wheel and theoretical domains framework. Public Health Front 2021; 9: doi:10.3389/fpubh.2021.610245
- Kaulio MA. Customer, consumer and user involvement in product development: a framework and a review of selected methods. Total Qual Manag 1998; 9: 141–149. doi:10.1080/0954412989333
- Boyd H, McKernon S, Mullin B et al. Improving healthcare through the use of co-design. N Z Med 2012; 125: 76–87.
- Gray D, Brown S, Macanufo J. Gamestorming: a playbook for innovators, rulebreakers, and changemakers. Sebastopol, CA: O’Reilly Media; 2010.
- van Someren MW, Barnard YF, Sandberg JAC. The think aloud method. A practical guide to modelling cognitive processes. London: Academic Press; 1994.
- Optometry Board of Australia. Guidelines: continuing professional development. In. [Online]: Optometry Board of Australia, 2019.
- Gocuk SA, Lee J-H, Keller PR et al. Clinical audit as an educative tool for optometrists: an intervention study in age-related macular degeneration. Ophthalmic Physiol Opt 2021; 41: 53–72. doi:10.1111/opo.12754
- Gagliardi AR, Brouwers MC, Finelli A et al. Physician self-audit: a scoping review. J Contin Educ Health Prof 2011; 31: 31. doi:10.1002/chp.20138
- Alhoqail RA. Self-audit in plastic surgery: toward total quality management of personal professional practice. J Craniofac Surg 2011; 22: 409–414. doi:10.1097/SCS.0b013e318207434b
- Craig P, Dieppe P, Macintyre S et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ 2008; 337: a1655. doi:10.1136/bmj.a1655
- Moore GF, Audrey S, Barker M et al. Process evaluation of complex interventions: medical research council guidance. BMJ 2015; 350: h1258. doi:10.1136/bmj.h1258
- Maatouk CM, Hentati F, Urbano CA et al. Effects of quality improvement education in diabetic retinopathy on routine clinical practice patterns of optometrists. Optom Vis Sci 2020; 97: 936–943. doi:10.1097/OPX.0000000000001595
- Proctor E, Silmere H, Raghavan R et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin Policy Mental Health Mental Health Services Res 2011; 38: 65–76. doi:10.1007/s10488-010-0319-7
- World Health Organization. Nine steps for developing a scaling-up strategy. WHO 2010.
- McKay H, Naylor PJ, Lau E et al. Implementation and scale-up of physical activity and behavioural nutrition interventions: an evaluation roadmap. Int J Behav Nutr Phys Act 2019; 16: 102. doi:10.1186/s12966-019-0868-4
- Milat AJ, Bauman A, Redman S. Narrative review of models and success factors for scaling up public health interventions. Implementation Sci 2015; 10: 113. doi:10.1186/s13012-015-0301-6
- Zamboni K, Schellenberg J, Hanson C et al. Assessing scalability of an intervention: why, how and who? Health Policy Plan 2019; 34: 544–552. doi:10.1093/heapol/czz068
- Milat AJ, Newson R, King L et al. A guide to scaling up population health interventions 2016; 26: e2611604.
- Indig D, Lee K, Grunseit A et al. Pathways for scaling up public health interventions. BMC Public Health 2017; 18: 68. doi:10.1186/s12889-017-4572-5
- Davidoff F, Dixon-Woods M, Leviton L et al. Demystifying theory and its use in improvement. BMJ Quality & Safety 2015; 24: 228–238. doi:10.1136/bmjqs-2014-003627
- Moullin JC, Dickson KS, Stadnick NA et al. Ten Recommendations for using implementation frameworks in research and practice. Implement Sci Comms 2020; 1: 42. doi:10.1186/s43058-020-00023-7
- Birken SA, Rohweder CL, Powell BJ et al. T-CaST: an implementation theory comparison and selection tool. Implementation Sci 2018; 13: 143. doi:10.1186/s13012-018-0836-4
- Powell BJ, Waltz TJ, Chinman MJ et al. A refined compilation of implementation strategies: results from the expert recommendations for Implementation Change (ERIC) project. Implementation Sci 2015; 10: 21. doi:10.1186/s13012-015-0209-1
- Colquhoun HL, Squires JE, Kolehmainen N et al. Methods for designing interventions to change healthcare professionals’ behaviour: a systematic review. Implementation Sci 2017; 12: 30. doi:10.1186/s13012-017-0560-5
- Phillips CJ, Marshall AP, Chaves NJ et al. Experiences of using the theoretical domains framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc 2015; 8: 139–146. doi:10.2147/JMDH.S78458
- Whittal A, Atkins L, Herber OR. What the guide does not tell you: reflections on and lessons learned from applying the COM-B behavior model for designing real life interventions. Transl Behav Med 2021; 11: 1122–1126. doi:10.1093/tbm/ibaa116
- Lazo-Porras M, Perez-Leon S, Cardenas MK et al. Lessons learned about co-creation: developing a complex intervention in rural peru. Glob Health Action 2020; 13: 1754016. doi:10.1080/16549716.2020.1754016
- Kirk J, Bandholm T, Andersen O et al. Challenges in co-designing an intervention to increase mobility in older patients: a qualitative study. J Health Organ Manag 2021; 35: 140–162. doi:10.1108/JHOM-02-2020-0049
- Kennedy A, Cosgrave C, Macdonald J et al. Translating co-design from face-to-face to online: an Australian primary producer project conducted during COVID-19. Int J Environ Res Public Health 2021; 18: 4147. doi:10.3390/ijerph18084147
- Schmid KL, Backhouse S, Cochrane AL et al. A snapshot of optometry teaching in Australia and New Zealand in response to COVID-19. Clin Exp Optom 2021; 104: 723–727. doi:10.1080/08164622.2021.1878859
- Efron N, Efron SE. Optometry in times of pandemic: Spanish flu (1919) versus COVID-19 (2020). Clin Exp Optom 2020; 103: 399–404. doi:10.1111/cxo.13094
- Australian Communications and Media Authority. Communications and media in Australia: how we use the internet. In. Available: acma.gov.au/research, 2021.
- Yokota F, Biyani M, Islam R et al. Lessons learned from co-design and co-production in a portable health clinic research project in Jaipur District, India (2016–2018). Sustainability 2018; 10: 4148. doi:10.3390/su10114148
