Vision loss leads to reduced quality of life with one metric to quantify this loss being disability-adjusted life years (DALYs): the number of vision-related loss of healthy years of life due to illness or disability and possibly premature death. In 2009, it was estimated that vision loss in Australia has led to over 58,000 DALYs (6,738 years of life lost and 51,409 years living with disability).Citation1 Optometrists have an integral part to play in eyecare delivery, including the diagnosis and management of eye conditions leading to DALYs. Early detection and suitable management minimise DALYs.
This special issue focusses on one of these sight-threatening eye conditions, glaucoma, with articles covering innovative testing/diagnostic techniques, glaucoma care delivery, as well as those that deepen our understanding of the mechanisms of glaucomatous damage and various functional deficits. Michael Twa recently wrote an Editorial highlighted that the discovery and dissemination of new knowledge provides the evidence base to improve clinical care and guide the self-determination of the optometric profession. In this regard, this glaucoma special issue will stimulate thinking towards better ways to deliver excellent eyecare through an improved understanding of basic and clinical science.
Prevalence and disease burden
Vision impairment from loss of retinal cells is among the most devastating disabilities, constituting a tremendous financial and emotional burden to the individual, their family, and the community.Citation1,Citation2 In 2009 dollars, it was estimated that the monetary cost of vision loss in Australia was $9.4 billion.Citation1 In Australia and other developed countries, an ageing and expanding population means that there is a concurrent rise in the prevalence and incidence of age-related blinding eye diseases such as glaucoma, which is predicted to rise to 111.8 million worldwide in 2040.Citation3
How are we doing in glaucoma diagnosis?
Mitchell et al.Citation4 in 1996 showed that about one half of those with glaucoma were undiagnosed from the Blue Mountains Eye Study (BMES). It is concerning that such high rates of underdiagnosis exist in Australia and other developed countries. In addition, we should be cognisant of the reported high rates of overdiagnosis.
Comparing the glaucoma undiagnosed rate in Australia 20 odd years after the original BMES, in a 2019 publication the undiagnosed glaucoma rate in Australia for the indigenous population was 72% and in the non-indigenous population was 46.6%.Citation5 More importantly, about one half of those who were undiagnosed self-reported that they had seen an optometrist or an ophthalmologist in the past 12 months.Citation5 Despite being aware of the high undiagnosed rate for over 20 years, recent studies continue to find high rates of undetected glaucoma within our community, even in those who have seen an optometrist or ophthalmologist in the past 12 months.
Clinical acumen, technology, collaborative care and more
The classification of normal versus glaucoma/other optic neuropathies and disease progression continue to evolve due to the introduction of new instrumentation, testing algorithms, regulatory testing requirements and overall evolution of our understanding of the disease ().Citation6 Phu et al.Citation6 provide an update of past and current glaucoma diagnostic criteria and proposed the adoption of a personalised approach in the diagnosis and management of glaucoma. To this end, optometrists have demonstrated a marked increase in using newer diagnostic techniques to assist in glaucoma diagnosis. Newer imaging technologies provide new useful insights such as clinical information from OCT-angiography (). These new technologies are evolving our understanding of glaucoma pathogenesis and assisting in developing improved clinical phenotyping for early detection.
Figure 1. A case example of a 39 year old who presented a diagnostic conundrum of glaucoma versus non-glaucomatous optic neuropathy. The patient was myopic, with a tilted and torted disc. An inferior retinal nerve fibre layer (RNFL) defect was appreciable on fundoscopic examination (black outline), with a correspondingly enlarged cup, but these features overlap with myopic optic neuropathy (‘how can clinicians distinguish between glaucoma and other optic disc variations?’). There was a concordant superior visual field defect found on visual field testing using both 24–2 and 10–2 test grids (‘when should clinicians be using the 10–2 test grid for glaucoma?’). Optical coherence tomography (OCT) imaging revealed statistically significant RNFL and ganglion cell-inner plexiform layer (GCIPL) thinning (green arrows), the pattern of which could potentially be differentiated using artificial intelligence (AI) models (‘what is the role of AI on integrating multimodal ocular imaging?’). OCT angiography can provide further information on retinal blood flow loss (orange arrows), which may assist in differentially diagnosing glaucoma from other optic nerve disease (‘what can OCT-angiography reveal about glaucoma?’). Images of people modified from Microsoft Office stock images.
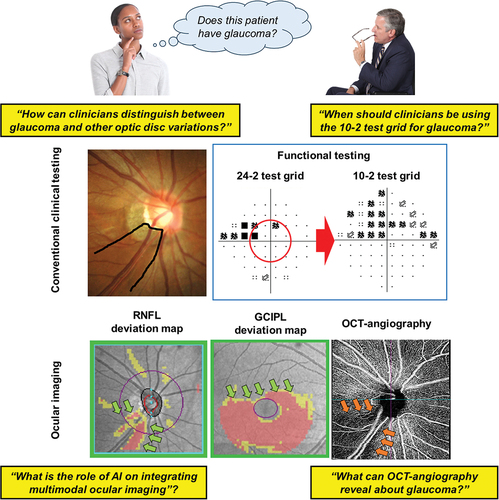
A major challenge in glaucoma visual field assessment is in deciding when to use different test grids: specifically, when the central 10–2 test grid might be more suitable or should be added to testing after the standard 24–2 test grid (). In this issue, Phu et al.Citation7 introduce the functional vulnerability zone concept in central vision and provide guidelines to assist clinicians (including a primary worksheet), to visualise the likelihood of a 10–2 test grid being useful for monitoring glaucoma.
Several papers in this issue focus on health care delivery and the clinical acumen of optometrists. When comparing glaucoma accredited optometrists in New Zealand and glaucoma specialists, there was overall agreement in most areas assessed (intraocular pressure [IOP], visual field and overall status of the disease) but less so on the interpretation of optical coherence tomography (OCT) images.Citation8 Thus, optometrists with appropriate training can make similar decisions in managing glaucoma patients with sub-speciality trained glaucoma ophthalmologists within a collaborative care model.
One way that may improve the undiagnosed glaucoma rate is more and improved collaborative care approaches. In this issue, studies support previous work showing the effectiveness of collaborative care and provide guidance on clinical skill levels and application of testing protocols (gonioscopy continuing to require attention). Given the effectiveness of optometry-ophthalmology collaborative care, it may be useful for the eyecare professions to work collaboratively and develop strategies to reduce the rate of undiagnosed glaucoma.
Identifying conversion to glaucoma or its progression remains a key goal of glaucoma clinical care and in this regard emerging technologies and artificial intelligence (AI) algorithms may be useful (). In this special issue, Hasan et al.Citation9 discuss core AI principles and provide a comprehensive review of available literature on glaucoma diagnosis. The use of AI in healthcare is almost exponentially increasing with performance matching or surpassing expert human performance. For example, in glaucoma, the AI diagnostic accuracy ranges from 67% to 98% and the area under the curve (AUC) metric of 0.71–0.98. This compares with human performance for an accuracy of 71.5% and an AUC of 0.86.Citation9 The improvement and validation of AI in glaucoma will further assist clinical diagnosis and management.
It is also important to consider functional vision deficits in activities of daily living with several manuscripts in this special issue providing useful information on this topic. Several articles also contribute to an improved understanding of the risk factors for glaucoma, for example, aqueous humour dynamics in myopia and the impact of various naturally occurring antioxidants on cell function. The impact of age on ganglion cell function with and without IOP elevation has improved our understanding the molecular pathways underlying age-related susceptibility in glaucoma, including the role of oxidative stress on neural, glial cells and the retinal vasculature.Citation10
In summary, glaucoma is a leading cause of irreversible vision loss. The increase in glaucoma prevalence due to the ageing population is placing pressure on health care delivery. Strategies to improve diagnosis and management include the use of AI and new clinical systems that are emerging through a constantly changing evidence base. Future clinical guidelines that involve intra- and inter-professional collaboration will lead to improved patient outcomes. Finally, a deeper understanding of disease mechanisms may yet yield novel therapies.
References
- Access Economics. Clear focus. The economic impact of vision loss in Australia in 2009. [accessed 2023 Dec 16]. https://www.vision2020australia.org.au/wp-content/uploads/2019/06/Access_Economics_Clear_Focus_Full_Report.pdf.
- Nyman SR, Gosney MA, Victor CR. Psychosocial impact of visual impairment in working-age adults. Br J Ophthalmol 2010; 94: 1427–1431. doi:10.1136/bjo.2009.164814.
- Tham YC, Li X, Wong TY et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014; 121: 2081–2090. doi:10.1016/j.ophtha.2014.05.013.
- Mitchell P, Smith W, Attebo K et al. Prevalence of open-angle glaucoma in Australia. The blue mountains eye study. Ophthalmology 1996; 103: 1661–1669. doi:10.1016/S0161-6420(96)30449-1.
- Keel S, Xie J, Foreman J et al. Prevalence of glaucoma in the Australian national eye health survey. Br J Ophthalmol 2019; 103: 191–195. doi:10.1136/bjophthalmol-2017-311786.
- Phu J, Agar A, Wang H et al. Management of open-angle glaucoma by primary eye-care practitioners: toward a personalised medicine approach. Clin Exp Optom 2021; 104: 367–84. doi:10.1111/cxo.13114.
- Phu J, Rafla D, Kalloniatis M. Which glaucoma patients benefit from 10-2 visual field testing? Proposing the functional vulnerability zone framework. Clin Exp Optom 2024; 1–13. (in press). doi:10.1080/08164622.2023.2288183.
- Green S, Ng RJ, Phillips G et al. Glaucoma Agreement in New Zealand (GAINZ). Clin Exp Optom 2024; 1–9. (in press). doi:10.1080/08164622.2023.2291063.
- Hasan Md M, Phu J, Sowmya A et al. Artificial intelligence in the diagnosis of glaucoma and neurodegenerative diseases. Clin Exp Optom 2024; 1–17. (in press). doi:10.1080/08164622.2023.2235346.
- van Koeverden ΑΚ, Afiat BA, Nguyen CTO et al. Understanding how ageing impacts ganglion cell susceptibility to injury in glaucoma. Clin Exp Optom 2024; 1–9. (in press). doi:10.1080/08164622.2023.2279734.
