Introduction
Lisch nodules are melanocytic hamartomas on the iris surface.Citation1 They are the most common ophthalmic manifestation of Neurofibromatosis type 1 (NF1), a genetic neurocutaneous disease.Citation2 Occasionally, the nodules are also present in other conditions such as Cushing’s syndrome.Citation3
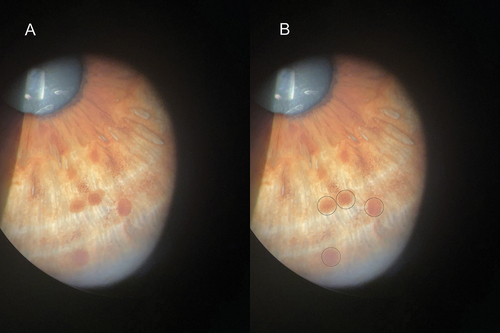
The nodules tend to form inferiorly on the iris.Citation4 In lighter irides they appear copper with blurry margins. In darker eyes they are cream and well demarcated.Citation1 Histologically, the nodules are like naevi which occur more posteriorly within the iris.Citation5 Optical coherence tomography (OCT) localises Lisch nodules to the iris anterior border.Citation6 Bilateral presentation is typical, however unilateral cases can occur in both children and adults.Citation7
Case report
Examination of an asymptomatic 50-year-old male revealed a cluster of brown circular nodules on the right peripheral iris surface between 4 and 6 o’clock (). The nodules had a smooth domed morphology with faded borders consistent with Lisch nodules. The patient did not have a family history of NF1.
There were no prominent corneal nerves, iris heterochromia, gonioscopic angle vessels or keratic precipitates. The patient had healthy optic nerves, normal pupil reflexes and no choroidal abnormalities. Visual field testing and posterior OCT were unremarkable. There was no evidence of plexiform neurofibroma affecting the eyelid, orbit, periorbita or face. Ophthalmoplegia and proptosis were not present.
Upon discussion, the patient elected to consult their general practitioner who would facilitate magnetic resonance imaging and dermatological evaluation. Future correspondence of these results was requested with the general practitioner. Additionally, annual eye examinations and screening of first-degree relatives was recommended.
Discussion
Lisch nodules may become more numerous over time.Citation2 They should be differentiated from naevi and variants including melanocytoma. These are typically larger, penetrate iris stroma and have potential for malignancy.Citation5,Citation8 Tapioca naevi may appear similar, although they have a more transparent glistening quality.Citation9 The domed morphology of Lisch nodules differs from flat iris freckles and they are larger than iris mammillations.Citation6,Citation10 A lack of inflammatory findings will rule out the possibility of uveitic Busacca nodules, a feature of Sarcoidosis.Citation11
Patients with Lisch nodules require screening for cutaneous signs of NF1, which include Café au lait macules. These are flat light brown patches of melanocytes.Citation12 Other NF1 findings include, distinctive freckling of the groin or armpit region, tumours on the skin (neurofibromas) and bone deformities.Citation12
Ocular complications in NF1 patients can occur in the form of optic pathway glioma, orbital neurofibromas, orbital bone dysplasia and congenital glaucoma.Citation13 Potentially fatal complications such as melanoma and central nervous system tumours occur in up to 25% of all Neurofibromatosis patients.Citation13
Unilateral Lisch nodules in patients over 16 years can be indicative of a segmental form of NF1 caused by somatic mosaicism.Citation12,Citation13 Here, post zygotic mutation of the NF1 gene leads to a mosaic of normal and affected cells within a region of the body.Citation14 Segmental NF1 is 10–15 times less prevalent, is typically not transmitted to progeny and has a lower incidence of systemic complications.Citation14,Citation15 Nevertheless there remains an increased risk of malignancies such as peripheral nerve sheath tumour.Citation15 These patients require annual eye examinations targeted at detecting visual pathway glioma. Workup including visual fields, OCT and fundoscopy are thus indicated.Citation16
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ragge NK, Falk RE, Cohen WE et al. Images of lisch nodules across the spectrum. Eye 1993; 7: 95–101. doi:10.1038/eye.1993.20.
- Lubs ML, Bauer MS, Formas ME et al. Lisch nodules in neurofibromatosis type 1. N Engl J Med 1991; 324: 1264–1266. doi:10.1056/NEJM199105023241807.
- Bouzas EA, Mastorakos G, Chrousos GP et al. Lisch nodules in Cushing’s disease. Arch Ophthalmol Chic 1993; 111: 439–440. doi:10.1001/archopht.1993.01090040029018.
- Boley S, Sloan JL, Pemov A et al. A quantitative assessment of the burden and distribution of lisch nodules in adults with neurofibromatosis type 1. Invest Ophthalmol Vis Sci 2009; 50: 5035–5043. doi:10.1167/iovs.09-3650.
- Karaconji T, Whist E, Jamieson RV et al. Neurofibromatosis type 1: review and update on emerging therapies. Asia-Pac J Ophthalmol 2019; 8: 62–72. doi:10.22608/APO.2018182.
- Mansour AM, Shields C. Optical coherence tomography of iris mammillations. Case Rep 2018; bcr–226591. doi:10.1136/bcr-2018-226591.
- Ceuterick SD, Den Ende Jj V, Smets RME. Clinical and genetic significance of unilateral lisch nodules. Bull Soc Belge Ophtalmol 2005; 295: 49–53.
- Shields CL, Shields PW, Manalac J et al. Review of cystic and solid tumors of the iris. Oman J Ophthalmol 2013; 6: 159–164. doi:10.4103/0974-620X.122269.
- Shields JA, Shields CL. Intraocular tumors: an atlas and textbook. Philadelphia (PA): Lippincott Williams & Wilkins; 2015.
- Edwards M, Cha D, Krithika S et al. Analysis of iris surface features in populations of diverse ancestry. R Soc Open Sci 2016; 3: 150424. doi:10.1098/rsos.150424.
- Herbort CP, Rao NA, Mochizuki M et al. International criteria for the diagnosis of ocular sarcoidosis: results of the first international workshop on ocular sarcoidosis (IWOS). Ocul Immunol Inflamm 2009; 17: 160–169. doi:10.1080/09273940902818861.
- Legius E, Messiaen L, Wolkenstein P et al. Revised diagnostic criteria for neurofibromatosis type 1 and legius syndrome: an international consensus recommendation. Genet Med Off J Am Coll Med Genet 2021; 23: 1506–1513. doi:10.1038/s41436-021-01170-5.
- Huson S, Jones D, Beck L. Ophthalmic manifestations of neurofibromatosis. Br J Ophthalmol 1987; 71: 235–238. doi:10.1136/bjo.71.3.235.
- Freed D, Stevens EL, Pevsner J. Somatic mosaicism in the human genome. Genes 2014; 5: 1064–1094. doi:10.3390/genes5041064.
- Gayathri A, Ramachandran R, Narasimhan M. Segmental neurofibromatosis with lisch nodules. Med J Armed Forces India 2023; 79: 356–359. doi:10.1016/j.mjafi.2020.11.021.
- Caen S, Cassiman C, Legius E et al. Comparative study of the ophthalmological examinations in neurofibromatosis type 1. Proposal for a new screening algorithm. Eur J Paediatr Neurol 2015; 19: 415–422. doi: 10.1016/j.ejpn.2015.03.002