ABSTRACT
Purpose: Interest in micro-invasive glaucoma surgery (MIGS) has exploded over the last 8 years with an increase in MIGS procedures of at least 400% in the United States, according to Medicare data. MIGS is an umbrella term that can cover many different types of surgeries. This review focuses on peer-reviewed evidence for Trabectome®, iStent inject®, Kahook Dual Blade®, XEN® Gel Stent, and Hydrus®. Methods: We present key recent studies evaluating the efficacy and safety of MIGS in various types of glaucoma patients with different stages of disease. Conclusion: We conclude that MIGS is generally safe and efficacious, although only some MIGS have been studied through randomized clinical trials. When comparing and contrasting the different MIGS procedures, large prospective studies are not yet the norm. High-quality large prospective studies involving MIGS will be an important next step as ophthalmologists decide how to incorporate MIGS into their surgical armamentarium.
INTRODUCTION
Micro-invasive glaucoma surgery (MIGS) presents a breakthrough opportunity for glaucoma surgeons to achieve lower intraocular pressure (IOP) and reduce medication burden without the risks and occasionally difficult postoperative course of traditional glaucoma surgeries, such as trabeculectomy and glaucoma drainage device implantation.Citation1 The US Medicare data demonstrate a significant trend towards MIGS over traditional incisional glaucoma surgeries. In 2017 alone, 174,788 glaucoma surgeries were performed. Of these surgeries, 13.1% were trabeculectomies, 11.4% were glaucoma drainage implants (GDIs), and 75.5% were MIGS.Citation2 Additionally, Centers for Medicare Services (CMS) collected data from all glaucoma surgeries performed in the US for Medicare beneficiaries from 2008 through 2016.Citation3 These data show a dramatic influx of MIGS procedures from 2012 to 2016, increasing by 426%. This large increase alone warrants a detailed, evidence-based review of the different devices available.
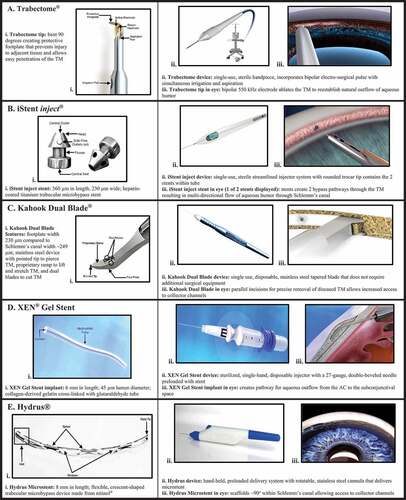
The term MIGS was created by Dr. Ike Ahmed in 2009, and it generally refers to a group of procedures with 5 aspects: ab interno, minimal disruption of normal anatomy, high safety profile, good efficacy, and quick recovery time.Citation4 Devices such as the iStent inject® and the Hydrus® would fit neatly into this definition. The term MIGS-plus may include other procedures conducted ab externo or that cause more than minimal disruption to the normal anatomy of the eye but still retain good efficacy, a high safety profile, and a relatively quick recovery for patients. Examples of these include the Trabectome®, the Kahook Dual Blade®, the XEN® Gel Stent as well as cyclodestructive procedures, the last of which have been reviewed recently and will not be discussed further.Citation5 Debate exists about which procedures truly classify as micro-invasive, but for the purpose of this review, the term MIGS will apply to all of the above. The relevant MIGS of this paper are further summarized in .
Figure 1. Summary of the different types of MIGS. A. Trabectome. B. iStent inject. C. Kahook Dual Blade. D. XEN Gel Stent. E. Hydrus
In general, MIGS do not reduce IOP as much as traditional incisional glaucoma surgeries, and therefore have been mostly reserved for mild-to-moderate glaucoma patients, although they have been studied in more severe forms as well. As the majority of MIGS procedures involve the trabecular meshwork, they have mostly been studied in open-angle glaucoma (OAG) subtypes, such as primary open-angle glaucoma (POAG), pigment dispersion glaucoma (PDG), and pseudoexfoliation glaucoma (PXG). That said, some studies have also included angle-closure glaucoma (ACG), normal-tension glaucoma (NTG), uveitic glaucoma, and even ocular hypertension (OHTN) patients. MIGS is frequently combined with cataract surgery, and their effect can be difficult to tease out from cataract surgery alone, which may reduce IOP by a mean 5 mmHg from an unmedicated, washed-out baseline.Citation6,Citation7 However, MIGS appears to consistently enhance the IOP reduction that cataract surgery alone provides.Citation6,Citation7 Nonetheless, active debate remains regarding the effectiveness and longevity of the various MIGS procedures. This paper presents selected peer-reviewed literature on the efficacy and safety of MIGS in adults. The literature has been selected by prioritizing prospective studies when available and otherwise choosing studies with larger sample sizes and longer-term follow-up. The goal of this review is to serve as a convenient reference for physicians who wish to incorporate the MIGS presented here into their clinical practice.
TRABECTOME®
The Trabectome, made available in 2006, was one of the first MIGS goniotomy devices developed. The ab interno trabeculectomy (AIT) instrument was FDA-approved in 2004 and started being used in 2006 to treat OAG in the US.Citation8,Citation9 The Trabectome uses electrocautery to remove a strip of the trabecular meshwork, generally over 90–120 degrees. The below studies are summarized in .
Table 1. Trabectome®
As Trabectome was one of the earliest MIGS to be developed, there has been more opportunity for its efficacy to be studied prospectively. As a standalone procedure, prospective studies have demonstrated Trabectome to decrease IOP by a mean of 22%–42% from baseline, and ≥20% IOP reduction can be observed in 23%–87% of the eyes with OAG over 1–2 years.Citation9,Citation10
Studies comparing Trabectome and phaco/Trabectome further support Trabectome’s role as an effective standalone procedure. One prospective study found that both Trabectome and phaco/Trabectome conferred reductions in IOP and IOP-lowering medication over 1 year. However, only the Trabectome group showed statistically significant reductions in both IOP and glaucoma medications at 1 year (p < .01, for both IOP and medications), whereas the phaco/Trabectome group showed declining trends for both variables yet did not meet statistical significance for either (p = .11 for IOP, p = .24 for medications).Citation11 A retrospective review of 1,340 eyes that had Trabectome with or without cataract surgery found that phaco/Trabectome reduced IOP by 1.29 ± 0.39 mmHg less than Trabectome alone (p < .01) over 12 months of follow-up.Citation12 On the other hand, a different retrospective review showed that both Trabectome and phaco/Trabectome groups had significant IOP and medication burden reductions from baseline over 1 year (p < .01), and that there was no statistically significant difference between the two groups (p ≥ .05).Citation13 Esfandari et al. published another retrospective interventional case series assessing phaco/Trabectome with 5 years of follow-up. At 5 years, 67.5% of the eyes had a ≥20% reduction in IOP, and the mean IOP had a significant reduction of 22% from baseline (p = .001).Citation14 Trabectome seems to perform just as well as phaco/Trabectome, or at worst, phaco/Trabectome may be slightly less effective than the standalone procedure.
Analyzing Trabectome’s performance across different glaucoma types and severities helps showcase the breadth of its efficacy. Trabectome has been found to be more effective in some subtypes and stages of OAG. In a retrospective analysis, Trabectome, with or without cataract surgery, showed PXG and steroid-induced glaucoma types to have significantly more IOP reduction than POAG at 1 year, with a reduction difference of 1.0 mmHg (p < .01).Citation12 The greater effect of Trabectome on PXG IOP reduction was also found in another retrospective study where PXG was associated with a higher success rate compared to other glaucoma types over the course of 5 years (p = .02).Citation14 When evaluating the effect of glaucoma severity on Trabectome’s performance, one retrospective study showed that eyes with severe glaucoma had an IOP reduction of 2.3 ± 0.2 mmHg more than eyes with less severe glaucoma at 1 year (p < .01).Citation12 Another study showed that in eyes with advanced OAG, IOP decreased 36% at 24 months, although medications were not reduced.Citation10 Trabectome has even been shown to be effective after a failed ab externo trabeculectomy with mitomycin C (MMC) in eyes with advanced glaucoma, lowering IOP by 19%–28% and reducing medications by a mean of 0.8–0.9.Citation11
When further evaluating medication burden reduction, Trabectome as a standalone procedure may reduce medications by 0–1.2 from baseline across any stage and type of OAG, in particular.Citation9–11,Citation13 Across the full spectrum of glaucoma, phaco/Trabectome may reduce medications by 0–0.8 from baseline.Citation11,Citation13,Citation14 In general, when looking at 12 months of follow-up, 19% of Trabectome and 24% of phaco/Trabectome patients showed statistically significant medication reduction from baseline for both groups (p < .01 for each group compared to baseline).Citation13 Based on the evidence provided in both prospective and retrospective studies, both Trabectome and phaco/Trabectome can significantly reduce medication burden over 1–5 years, although phaco/Trabectome may be slightly more effective in doing so.
In addition to assessing Trabectome’s efficacy across various glaucoma types and severities with or without cataract surgery, evaluating Trabectome’s performance against other MIGS is beneficial. Trabectome has been compared to a newer form of MIGS, the iStent inject®, both combined with cataract surgery. One study found that in eyes with all stages and types of glaucoma, phaco/Trabectome lowered IOP by 22.7%, which was sustained for 2 years, while the IOP reduction from iStent inject with cataract surgery (phaco/iStent inject) began to wear off at 6 months and became non-significant at 2 years.Citation15 Despite phaco/Trabectome’s IOP-lowering effect, the mean medication reduction between phaco/Trabectome and phaco/iStent inject was not statistically different.Citation15
The most frequent complication of Trabectome was bleeding in the form of hyphema (23%–48%), microhyphema (27%–77%), delayed-onset hyphema (5%), and intraoperative blood reflux (59%-100%).Citation9,Citation10,Citation14 Hyphema generally cleared between 1 and 10 days postoperatively.Citation12 A moderate proportion of eyes also went on to have subsequent glaucoma surgery during the follow-up period (15%–18%), and some eyes had IOP spikes >10 mmHg from baseline (5%–27%).Citation10,Citation11,Citation14
ISTENT INJECT®
The first-generation iStent® implant is a trabecular meshwork-bypass stent approved by the US FDA in 2012 for use in conjunction with cataract surgery for patients currently being treated with IOP-lowering medication and who have a diagnosis of mild-to-moderate OAG.Citation16 Most surgeons now use the second-generation iStent, called the iStent inject, which was approved by the FDA in June 2018. The iStent inject has two heparin-coated titanium 230-micron stents with a central lumen of 80 microns that are placed ab interno in combination with cataract surgery into two different regions of the trabecular meshwork. The iStent inject has demonstrated greater efficacy compared to its first-generation counterpart.Citation16,Citation17 Therefore, for the purpose of this review, we will focus on available data for the iStent inject. A number of studies summarized in have demonstrated the iStent inject to be an effective and safe option for glaucoma patients.
Table 2. iStent inject®
Prospective studies assessing phaco/iStent inject showed a significant mean IOP reduction of 2.8–7.0 mmHg over 1–2 years (p < .001).Citation6,Citation18 These studies, along with a retrospective study, reflect a range of 17.8%–31.0% IOP reduction from the baseline over 1–2 years.Citation6,Citation18,Citation19 Moreover, 54.5–75.8% of the eyes reached ≥20% IOP reduction at 2 years.Citation6,Citation19 Comparing phaco/iStent inject to cataract surgery alone, a procedure that can also lower IOP albeit modestly, phaco/iStent inject produced significantly greater reductions in IOP (an additional 1.6 mmHg) and glaucoma medication (0.5 medications less) over the course of 2 years compared to the results of cataract surgery alone (p < .001).Citation6
Although in the US the iStent inject is intended to be implanted in conjunction with cataract surgery (Glaukos), international, prospective studies have evaluated the iStent inject as a standalone procedure. In these studies, the mean IOP reduction ranges from 10.2 to 12.2 mmHg (39.7%–48.4%) over 1–3 years of follow-up.Citation20–22 Of these participants 72.0%–94.7% achieved ≥20% IOP reduction. One study compared the iStent inject as a standalone procedure to a medical therapy group, consisting of a fixed combination of latanoprost/timolol. Both groups met similar inclusion criteria, including a diagnosis of mild-to-moderate OAG. Ninety-seven percent were phakic, while uncontrolled on one glaucoma medication and a washout period of current glaucoma medications.Citation20 Approximately 95% of the patients in the iStent inject group reached a ≥20% IOP reduction without the need for glaucoma medications across 12 months. In contrast, 91.8% of the patients in the medical therapy group reached this IOP reduction across the same time period. Interestingly, the iStent inject group was more likely to reach ≥50% IOP reduction (p = .02).Citation20 Another prospective study examining the effectiveness of the iStent inject as a standalone procedure found that 72% of the subjects experienced a ≥20% IOP reduction and were free of IOP-lowering medications at 12 months.Citation21 In this same study, about 93% of the subjects experienced a ≥20% reduction at 12 months when medications were used.Citation21
Regarding medication burden reduction, the iStent inject as a standalone procedure showed a reduction of two or more medications and one medication, respectively, in 71.1% and 15.2% of the patients with uncontrolled OAG on at least two glaucoma medications, according to one prospective study with 12 months of follow-up.Citation21 Another prospective study looking at the iStent inject as a standalone procedure for patients with POAG, ACG, PXG, or other secondary glaucoma that was uncontrolled despite medication or surgical intervention showed that the mean medication burden after iStent inject decreased by 82% with the mean number of medications reduced by 2.4 at 3 years of follow-up (p < .0001), and 61% became medication-free at 3 years.Citation22 For phaco/iStent inject, the range of mean medication reduction was 1.2–1.7 over 1–2 years (p < .001 across all studies).Citation6,Citation18,Citation19 In the two prospective studies, 47% of the eyes from patients with mild-to-moderate POAG and 63.2% of the eyes from patients with any stage OAG were medication-free at 1 and 2 years, respectively.Citation6,Citation18 Similarly, a retrospective study of phaco/iStent inject found 81.1% of the eyes and 72.7% of the eyes to be medication-free at 12 and 24 months, respectively. The proportion of medication-free eyes was significantly increased from baseline in all types of glaucoma assessed, including POAG, PXG, NTG, and even OHTN (p < .001 at both follow-up points).Citation19
Neuhann et al. also found significant reductions in IOP at 24 months with phaco/iStent in all aforementioned subtypes of glaucoma except for NTG (p < .001).Citation19 However, the 10 eyes in the NTG group were all medication-free by 24 months even if their baseline medicated IOP did not change. Salimi et al. further investigated the breadth of the iStent inject’s effectiveness in a prospective study and found that phaco/iStent inject works across the full spectrum of glaucoma subtypes and severity. They showed that phaco/iStent inject lowers IOP and medication burden from baseline in patients with POAG, ACG, NTG, PXG, and PDG with varying degrees of severity (p < .001 across both variables and each subtype).Citation18 Additionally, the authors found no statistically significant differences for IOP reduction or medication burden between-group types and severities. With retrospective and prospective studies showing that the iStent inject can lower medication burden and decrease IOP to varying degrees across different glaucoma subtypes and severity levels, it may be that the iStent inject could be used more frequently and not only in mild-to-moderate POAG patients.
The efficacy of both the first-generation iStent implant and the iStent inject have been compared with older and newer types of MIGS. The Kahook Dual Blade® (KDB) with cataract surgery (phaco/KDB) appears to confer an additional 1.5 mmHg of IOP-lowering versus the iStent implant with cataract surgery (phaco/iStent) according to a retrospective review by Dorairaj et al.Citation23 However, in a smaller study by Lee et al., IOP-lowering appeared to be equal, although medication burden was lessened more in the KDB group (43.2% used ≥1 medication less in the KDB group compared to 17.2% in the iStent group).Citation23,Citation24 When we compare iStent inject to Hydrus as standalone procedures, Hydrus® was found to be more effective than the iStent inject according to the COMPARE study.Citation25 In this study, eyes were prospectively randomized to Hydrus or to the iStent inject. At 12 months, the mean IOP decreased significantly more from the screening and baseline IOP in the Hydrus group.Citation25 Studies comparing phaco/iStent inject versus phaco/Trabectome were discussed in the Trabectome section above.
In terms of the iStent inject’s safety profile, studies determined that its safety is comparable to that of cataract surgery alone.Citation6 The most common adverse effects reported include stent obstruction (6.2%–13.2%), IOP spike (5.2%–11%), corneal edema (10%), posterior capsular opacification (5.2%–11%), rebound iritis (6%), inflammation (5.7%), microhyphema (3.9%-5%), and BCVA worsening (1%–1.3%).Citation6,Citation18,Citation25 In terms of hyphema, none of these studies reported hyphemas occupying ≥10% of the anterior chamber. Depending on the study, between 1.6% and 5.1% of the patients required additional glaucoma surgery to control IOP.Citation17
KAHOOK DUAL BLADE®
The Kahook Dual Blade (KDB; New World Medical, Rancho Cucamonga, CA, USA) was made available in 2015 as a method to perform ab interno goniotomy and trabeculectomy. The blade removes a strip of trabecular meshwork generally 3–5 clock hours in length and can be used with or without cataract surgery. The below studies are summarized in . In terms of improvements to KDB, New World Medical announced in October 2020 the FDA’s approval of the KDB GLIDE™, which sought to improve ease of use and precision when excising the trabecular meshwork (New World Medical).
Table 3. Kahook Dual Blade®
The efficacy of KDB as a standalone procedure has largely been demonstrated through retrospective reviews with IOP reductions ranging from 4 to 11 mmHg, absolute IOP reductions between 14.5% and 36.0%, and follow-up periods of 6–12 months. The success of IOP reduction seems to depend on the type of glaucoma being treated, with 40%–100% of the eyes achieving a ≥20% reduction in IOP.Citation26,Citation27 Eyes with OAG and its subtypes appear to reach the 20% reduction mark 42%–72% of the time, whereas ACG patients appear to reach that 20% reduction mark up to 100% of the time.Citation26–28 When the uveitic glaucoma patients with elevated IOP were studied, only about 38% of them achieved the 20% reduction mark.Citation29 Although the retrospective studies referenced above focus on KDB as a standalone procedure, KDB has been shown to be similarly effective with cataract surgery. Using the 20% IOP reduction mark as a success standpoint, phaco/KDB demonstrated that 72% of the eyes had ≥20% IOP reduction, which was not statistically different from KDB alone in which 69% had ≥20% IOP reduction.Citation28 Overall, phaco/KDB has demonstrated absolute IOP reductions between 14.5% and 24% in retrospective studies focusing on OAG patients.Citation24,Citation26,Citation27,Citation30 In terms of medication reduction, as a standalone procedure, KDB may reduce medications by 0–1, and phaco/KDB may reduce medications by 0.1–2.1 in glaucoma of all types and severities.Citation23,Citation24,Citation28–30
In general, the severity and type of glaucoma have not been significantly correlated with KDB success rates, although most studies were done in mild-to-moderate glaucoma or OHTN patients.Citation28,Citation30 KDB has been shown to be effective in severe/refractive OAG and ACG, reducing IOP by up to 24% in these patients.Citation31 Across glaucoma severities of mild, moderate, severe, and indeterminate, there was no statistically significant difference between groups and the majority of eyes achieved success and maintained IOP-lowering effects at 12 months of follow-up. Additionally, the majority of eyes for the different glaucoma subtypes studied reached success benchmarks, with no significant difference between groups.Citation28 Studies have shown that a higher baseline IOP has been predictive of larger IOP reductions by KDB regardless of glaucoma severity or subtype.Citation28,Citation30
KDB has been studied in comparison to the first-generation iStent and to 360° ab interno trabeculectomy via both TRAB™360 or gonioscopy-assisted transluminal trabeculectomy (GATT) in OAG. The phaco/iStent versus phaco/KDB study is described in the iStent inject section of this review.Citation23,Citation24 Comparing KDB to TRAB™360 or GATT, all combined with cataract surgery, significantly more KDB eyes achieved the target IOP of ≤18 mmHg (p = .04) and ≤15 mmHg (p = .003) at 6 months of follow-up.Citation32 Due to space constraints, ab interno trabeculectomy via TRAB™360 and GATT will not be discussed in detail in this review.
The most common complication of KDB was hyphema, which occurred 6%–19% of the time, with the majority resolving by postoperative month 1.Citation23,Citation24,Citation26–30 Another complication was surgical failure, with patients requiring further glaucoma surgery in 4%–25% of the cases.Citation23,Citation24,Citation26–30 The surgical failure rate appears to be highest in the uveitic group. Other reported complications include IOP spikes (1%–18%), Descemet’s membrane tears (3.8%), and cystoid macular edema (2%–6%).Citation23,Citation24,Citation26–30
XEN® GEL STENT
The XEN Gel Stent (XGS, Allergan INC, Dublin, Ireland) is a 6 mm porcine collagen implant cross-linked with glutaraldehyde, approved by the US FDA in November 2016. It is placed either ab interno or ab externo, with or without opening conjunctiva, to drain fluid into the subconjunctival space in a controlled manner through a 45-micron lumen. It is approved for refractory glaucoma patients, defined as patients who failed previous surgery or maximum tolerated medical treatment. The studies below are summarized in .
Table 4. XEN® Gel Stent
For ab interno placement of the XGS without opening conjunctiva, which remains the most common placement method both as a standalone procedure (XGS) and combined with cataract surgery (phaco/XGS), retrospective and prospective studies show that 44.6%–97.4% of the patients with mild-to-moderate POAG achieved an IOP reduction ≥20% from baseline over 1–2 years.Citation33–35 One retrospective study found significant reductions in IOP as well as medication burden for both XGS alone and phaco/XGS groups at 2 years (p < .001 and p = .009, respectively).Citation34 Reitsamer et al. found that 44.7% of all eyes were medication-free at 2 years, with no statistically significant difference between the XGS alone and phaco/XGS groups.Citation33 Of note, these studies excluded patients with prior incisional surgery.
One retrospective study compared the XGS placements ab externo without opening conjunctiva to ab interno without opening conjunctiva. This study showed that both methods significantly lowered IOP and medication burden over 1 year (p < .05) with no statistically significant difference between groups.Citation35 However, one key difference between the groups was the number of participants requiring needling post-surgery. At 12 months, only 27.9% of XGS ab externo with closed conjunctiva patients required needling, versus 45.5% for XGS ab interno with closed conjunctiva (p < .05).Citation35 This study suggests that ab externo placement of the XGS may reduce needling rates, although this warrants further investigation.
The US Pivotal study, which aided XGS’s FDA approval in the US, assessed XGS placement ab interno with opening of conjunctiva in patients with refractory glaucoma. This study included patients who failed prior glaucoma surgery, as opposed to the previously discussed studies, which excluded prior glaucoma surgery from subject inclusion criteria. Specifically, 84.6% of the patients included had failed a prior glaucoma surgery, and 56.9% were on ≥4 IOP-lowering agents.Citation36 Patients were treated with 0.2 mg/ml MMC before XGS implantation. At 12 months, 75.4% of the patients experienced ≥20% IOP-lowering from baseline on the same or fewer medications with a mean IOP reduction of about 9 mmHg. Overall, 31.5% of the patients required needling by 12 months.Citation36
Few studies have looked at ab externo XGS placement with opening conjunctiva. One review paper covered a retrospective cohort study with 45 patients who had previously failed glaucoma surgery and had conjunctival scarring.Citation37 The patients underwent standalone XGS ab externo with open conjunctiva and were followed for 12 months. At 12 months, 71% of the patients had an IOP reduction ≥20% or had an IOP less than 18 mmHg on no glaucoma medications. About 96% of the patients met these success criteria when IOP-lowering medications were used. Although data have yet to be published, the study’s surgeons agreed that their needling rates have declined using the ab externo, open conjunctiva method, with one author further observing less than 5% of his patients requiring needling. Future comparative studies would help provide insight regarding whether an open or closed conjunctiva approach would be more beneficial for the ab externo technique.Citation37
There have been mixed results on the effect of concurrent cataract surgery with XGS. In one prospective study discussed above, patients with mild-to-moderate POAG without a history of prior IOP-lowering surgery underwent phaco/XGS.Citation33 At 2 years of follow-up, no significant differences were found between phaco/XGS and XGS alone groups for IOP reduction, medication burden, or needling rates. Notably, pseudophakic patients who received XGS alone had similar outcomes to patients who underwent phaco/XGS and to phakic patients who underwent XGS alone.Citation33 In contrast, another prospective study found only 56.1% of phaco/XGS had clinical success at 1 year, which was statistically significantly lower than the results they obtained with the standalone XGS (p < .01).Citation38 For both prospective studies, the surgeons performed phacoemulsification followed by the XGS implanted ab interno with closed conjunctiva. MMC was used in all patients in both studies though at different doses, with the majority receiving 0.1 mg/ml in the first study and 0.2 mg/ml in the second. Regarding the first study, Reitsamer et al. found similar results across XGS alone and phaco/XGS groups for reduction of IOP and IOP-lowering medications at all postoperative visits up to 24 months (p > .4, between-group comparison). The overall absolute IOP reduction from baseline was 29.3% at 12 months, which was similar to Mansouri et al.’s finding of 31% reduction at 12 months. They observed no significant differences in needling rates between groups at 24 months (p > .5, between-group comparison). Mansouri et al. observed a larger IOP-lowering effect in the XGS alone group versus phaco/XGS. However, they stated that this difference could be explained by the higher preoperative IOP and baseline number of medications in the XGS alone group compared to the phaco/XGS group, 20.0 versus 18.0 mmHg and 2.5 versus 2.0, respectively. Unlike Mansouri et al., the between-group preoperative IOP values and the number of IOP-lowering medications are comparable to each other (refer to ). Similar to Reitsamer et al.’s findings, there was no statistically significant association between surgical success and needling (p = .22).Citation33,Citation38
When directly compared to other MIGS in studies, the XGS has been found to be more effective than GATT at lowering IOP. Olgun et al. performed a retrospective study to assess the efficacy of the XGS ab interno with closed conjunctiva compared to GATT, both with or without cataract surgery in patients with OAG.Citation34 Both groups demonstrated significant IOP reductions at 2 years compared to the baseline (p < .001). However, at all postoperative visits, XGS produced significantly lower mean IOP values than did GATT (p < .001). Additionally, both XGS alone and phaco/XGS groups showed more improvement in BCVA than both equivalent GATT groups (p = .003 and 0.012, respectively).Citation34 All groups had a low number of adverse events reported. This study supports both types of MIGS as safe and efficacious procedures for patients with OAG, with XGS being potentially more favorable for patients who require lower target IOP values.
Needling is one of the most common complications of the XGS, required for 27.9%–45.5% of the patients.Citation33–36 Hyphema occurred 4.6%–28.0% of the time. Other adverse effects include hypotony that usually self-resolves (20.2–24.6%), wound leak or dehiscence (9.2%), and problems with implant positioning (1.8%–4.7%).Citation34,Citation35 Corneal edema, subconjunctival hemorrhage, endophthalmitis, and iridodialysis all occurred ≤1.5% of the time.Citation33,Citation34,Citation36 Overall, 1.5%–13.8% of XGS patients studied over 1–2 years required additional glaucoma surgery to control IOP.
HYDRUS®
The Hydrus Microstent (Ivantis, Inc, Irvine, CA) received FDA approval in August 2018. It is a nitinol trabecular bypass device approved in the US for mild-to-moderate POAG patients undergoing concurrent cataract surgery. It is inserted into Schlemm’s canal spanning 90°. The studies below are summarized in .
Table 5. Hydrus®
Standalone Hydrus was shown to produce significant IOP and medication reductions in a prospective study across phakic and pseudophakic patients with mild-to-moderate OAG, including POAG, PXG, and PDG patients. About 46.6% of the patients were medication-free at 12 months. Additionally, 39.7% of the patients met complete surgical success with ≥20% IOP reduction from baseline and no IOP-lowering medications.Citation25
Several prospective studies have compared Hydrus with cataract surgery (phaco/Hydrus) to cataract surgery alone.Citation7,Citation39,Citation40 These studies show that phaco/Hydrus can significantly lower IOP 7.6–8.1 mmHg from baseline over 2–3 years. Additionally, each study supports a favorable outcome of phaco/Hydrus compared to cataract surgery alone. At 2–3 years, 64.0%–78.5% of phaco/Hydrus eyes had an IOP reduction ≥20% versus only 46.0%–57.8% of eyes that underwent cataract surgery alone (p < .001 for two studies, and p = .05 for one study). About 55.8%–78.5% of phaco/Hydrus eyes were also medication-free at 2–3 years versus 30.0%–39.2% that had cataract surgery alone (p < .001 and p = .02).Citation39,Citation40 One prospective study also showed that Hydrus conferred an additional 2.3 mmHg reduction in IOP over cataract surgery and an additional reduction in medications of 0.4 (p < .001 for both variables).Citation7 When studying phaco/Hydrus versus cataract surgery alone, Jones et al. observed significantly lower IOP reduction in both groups for patients who underwent SLT prior to the study compared to eyes without a history of SLT. However, phaco/Hydrus eyes with or without a history of SLT still have statistically significant IOP reductions compared to cataract surgery alone.Citation39
Phaco/Hydrus and cataract surgery alone appear to have similar safety profiles.Citation7,Citation39,Citation40 The most common complications reported concerning the Hydrus Microstent are synechiae (6.8%–14.9%), uveitis or iritis (4.6%–5.6%), device obstruction (1.8%–5.4%), and hyphema (1.4%–1.6%). Additionally, 0–4% of the patients required additional glaucoma surgery to control IOP.Citation7,Citation39,Citation40 Interestingly, phaco/Hydrus appeared to confer some protection against IOP spikes, defined as >10 mmHg above baseline IOP. Only 0.5%–0.9% of phaco/Hydrus eyes experienced an IOP spike, whereas 2.7% of eyes that underwent cataract surgery alone and 4.1% of eyes that underwent standalone Hydrus experienced an IOP spike when the various studies are examined.Citation7,Citation25,Citation39,Citation40 This comparison may be unfair as each study had different parameters, but these data suggest that phaco/Hydrus may be protective against postoperative day 1 IOP spikes.
CONCLUSION
This review summarized data from studies evaluating the various MIGS in the adult glaucoma population and across the full spectrum of disease. In general, MIGS were found to be efficacious and safe, although it is still difficult to know which type of patient will benefit most from a specific type of MIGS. Further prospective randomized comparative trials are needed to better answer that question. Additional trials are particularly important as the breadth and popularity of MIGS have broadened dramatically over the last 8 years and will likely continue to do so.
Sources of Support
With grateful appreciation to Mr. Joseph Leitch, Mrs. Cathey S. Leitch, Mr. Chad Gifford, Mrs. Anne Gifford, and Mr. Stephen Traynor for their philanthropic support of this work.
Disclosure of Interest
The authors report no conflict of interest.
Figure References
1. Trabectome® Pack. MicroSurgical Technology. https://microsurgical.com/products/mst-products/trabectome/. Accessed February 27, 2021.
2. iStent inject v iStent inject W Comparison Sheet.pdf. Showpad Online Platform. https://glaukos.showpad.com/share/mDEzN8eY4BnobpFGsmg9E. Accessed February 27, 2021.
3. iStent inject®. Glaukos. https://www.glaukos.com/enca/healthcare-professionals/istent-inject/. Published June 15, 2017. Accessed February 27, 2021.
4. Center for Devices and Radiological Health. iStent inject Trabecular Micro-Bypass System (Model G2-M-IS). U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/recently-approved-devices/istent-inject-trabecular-micro-bypass-system-model-g2-m-p170043. Accessed February 27, 2021.
5. Kahook Dual Blade®: Excisional Goniotomy for Implant Free Surgery. New World Medical. https://www.newworldmedical.com/kahook-dual-blade/. Published February 2, 2021. Accessed February 27, 2021.
6. About Xen. Xen Gel Stent. https://hcp.xengelstent.com/about-xen. Accessed February 27, 2021.
7. The Hydrus® Microstent Procedure. Ivantis. https://www.ivantisinc.com/healthcare-professionals/hydrus-procedure/. Published January 26, 2021. Accessed February 27, 2021.
Acknowledgments
Elisabeth Hansen, BA, who served as a proofreader of this work.
References
- Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012 May;153(5):789–803.
- Ma AK, Lee JH, Warren JL, Teng CC. GlaucoMap – distribution of glaucoma surgical procedures in the United States. Clin Ophthalmol. 2020;Volume 14:2551–2560. doi:10.2147/OPTH.S257361.
- Rathi S, Andrews CA, Greenfield DS, Stein JD. Trends in Glaucoma surgeries performed by Glaucoma subspecialists versus nonsubspecialists on medicare beneficiaries from 2008 through 2016. Ophthalmology. 2020;128(1):30–38. doi:10.1016/j.ophtha.2020.06.051.
- Saheb H, Ahmed IIK. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012 March;23(2):96–104. doi:10.1097/ICU.0b013e32834ff1e7.
- Anand N, Klug E, Nirappel A, et al. A Review of Cyclodestructive Procedures for the Treatment of Glaucoma. Seminars in Ophthalmology. 2020;25(5–6):261–275.
- Samuelson TW, Sarkisian SR, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular mico-bypass in primary open-angle glaucoma and cataract: two year results. Ophthalmology. 2019;126(6):811–821. doi:10.1016/j.ophtha.2019.03.006.
- Samuelson TW, Chang DF, Marquis R, et al. A schlemm canal microstent for intraocular pressure reduction in primary open-angle Glaucoma and cataract: the HORIZON study. Ophthalmology. 2019;126(1):29–37.doi:10.1016/j.ophtha.2018.05.012.
- Schehlein EM, Kaleem MA, Swamy R, Saeedi OJ. Microinvasive Glaucoma surgery: an evidence-based assessment. Expert Rev Ophthalmol. 2017;12(4):331–343. doi:10.1080/17469899.2017.1335597.
- Minckler D, Mosaed S, Dustin L, Francis B, Group TS. Trabectome (Trabeculectomy-Internal Approach): additional experience and extended follow-up. Trans Am Ophthalmol Soc. 2008;106:149–160.
- Mizoguchi T, Nishigaki S, Sato T, Wakiyama H, Ogino N. Clinical results of Trabectome surgery for open-angle glaucoma. Clin Ophthalmol. 2015;9:1889–1894. doi:10.2147/OPTH.S83958.
- Bussel II, Kaplowitz K, Schuman JS, Loewen NA. Outcomes of ab interno trabeculectomy with the trabectome after failed trabeculectomy. Br J Ophthalmol. 2015;99(2):258–262. doi:10.1136/bjophthalmol-2013-304717.
- Dang Y, Roy P, Bussel II, Loewen RT, Parikh H, Loewen NA. Combined analysis of trabectome and phaco-trabectome outcomes by glaucoma severity. F1000Res. 2016;5:762. doi:10.12688/f1000research.8448.2.
- Parikh HA, Bussel II, Schuman JS, Brown EN, Loewen NA. Coarsened exact matching of phaco-trabectome to trabectome in phakic patients: lack of additional pressure reduction from phacoemulsification. Plos One. 2016 Feb;11(2):e0149384. doi:10.1371/journal.pone.0149384.
- Esfandari H, Shah P, Torkian P, et al. Five-year clinical outcomes of combined phacoemulsification and trabectome surgery at a single glaucoma center. Graefes Arch Clin Exp Ophthalmol. 2019;257(2):357–362. doi:10.1007/s00417-018-4146-y.
- Yousef AY, Strzalkowska A, Hillenkamp J, Rosentreter A, Loewen NA. Comparison of a second-generation trabecular bypass (iStent inject) to ab interno trabeculectomy (Trabectome) by exact matching. Graefe’s Archive for Clinical and Experimental Ophthalmology. Arch Clin Exp Ophthalmol. 2020;258(12):2775–2780. doi:10.1007/s00417-020-04933-z. 2020.
- Real-world Case MD. Series of iStent or iStent inject Trabecular micro-bypass stents combined with cataract surgery. Ophthalmol Ther. 2019;8(4):549–561. doi:10.1007/s40123-019-00208-x.
- Guedes RAP, Gravina DM, Lake JC, Guedes VMP, Chaoubah A. Intermediate results of iStent or iStent inject implantation combined with cataract surgery in a real-world setting: a longitudinal retrospective study. Ophthalmol Ther. 2019;8(1):87–100. doi:10.1007/s40123-019-0166-x.
- Salimi A, Lapointe J, One-Year HP. Outcomes of second-generation trabecular micro-bypass stents (iStent Inject) implantation with cataract surgery in different Glaucoma subtypes and severities. Ophthalmol Ther. 2019;8(4):563–575. doi:10.1007/s40123-019-00214-z.
- Neuhann R, Neuhann T. Second-generation trabecular micro-bypass stent implantation: retrospective analysis after 12- and 24-month follow-up. Eye and Vision. 2020;7(1):1. doi:10.1186/s40662-019-0169-7.
- Fea AM, Belda JI, Rękas M, et al. Prospective unmasked randomized evaluation of the iStent inject (®) versus two ocular hypotensive agents in patients with primary open-angle glaucoma. Clinical Ophthalmology. 2014;8:875–882. Published 2014 May 7. doi:10.2147/OPTH.S59932
- Voskanyan L, García-Feijoó J, Belda JI, Fea A, Jüneman A, Prospective BC. Unmasked Evaluation of the iStent Inject system for open-angle Glaucoma: synergy trial. Adv Ther. 2014;31(2):189–201. doi:10.1007/s12325-014-0095-y.
- Hengerer FH, Auffarth GU, Riffel C, Second-Generation Trabecular C-HI. Micro-Bypass stents as standalone treatment for Glaucoma: a 36-Month Prospective Study. Adv Ther. 2019;36(7):1606–1617. doi:10.1007/s12325-019-00984-9.
- Dorairaj SK, Kahook MY, Williamson BK, Seibold LK, ElMallah MK, Singh IP. A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction. Clin Ophthalmol. 2018;12:791–797.
- Lee D, King J, Thomsen S, Hirabayashi M, Comparison AJ. Of surgical outcomes between excisional goniotomy using the Kahook Dual Blade and iStent Trabecular micro-bypass stent in combination with phacoemulsification. Clin Ophthalmol. 2019;13:2097–2102. doi:10.2147/OPTH.S224109.
- Ahmed IIK, Fea A, Au L, et al. A prospective randomized trial comparing Hydrus and iStent microinvasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: the COMPARE study. Ophthalmology. 2020;127(1):52–56. doi:10.1016/j.ophtha.2019.04.034.
- Dorairaj S, Tam MD. Kahook Dual Blade Excisional Goniotomy and Goniosynechialysis combined with phacoemulsification for angle-closure Glaucoma: 6-month results. J Glaucoma. 2019;28(7):643–646. doi:10.1097/IJG.0000000000001256.
- ElMallah MK, Berdahl JP, Williamson BK. et al. Twelve-month outcomes of stand-alone excisional goniotomy in mild to severe Glaucoma. Clin Ophthalmol. 2020;14:1891–1897. doi:10.2147/OPTH.S256423.
- Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of Kahook Dual Blade Goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma. 2018;1(1):75–81.doi:10.1016/j.ogla.2018.06.006.
- Miller VJ, Young CEC, SooHoo JR, et al. Efficacy of Goniotomy with Kahook Dual Blade in patients with uveitis-associated ocular hypertension. J Glaucoma. 2019;28(8):744–748.doi:10.1097/IJG.0000000000001298.
- Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of goniotomy performed with the Kahook Dual Blade as a stand-alone Glaucoma procedure. Adv Ther. 2018;35(11):2093–2102.doi:10.1007/s12325-018-0803-0.
- Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma. 2018;27(10):849–855.doi:10.1097/IJG.0000000000001019.
- Hirabayashi MT, Lee D, King JT, Thomsen S, An JA. Comparison Of Surgical Outcomes Of 360° Circumferential Trabeculotomy Versus Sectoral Excisional Goniotomy With The Kahook Dual Blade At 6 Months. Clin Ophthalmol. 2019;13:2017–2024. doi:10.2147/OPTH.S208468.
- Reitsamer H, Sng C, Lenzhofer M, Barton K, Stalmans I, Group AS. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):983–996. doi:10.1007/s00417-019-04251-z.
- Olgun A, Aktas Z, Ucgul A. XEN gel implant versus gonioscopy-assisted transluminal trabeculotomy for the treatment of open-angle glaucoma. Int Ophthalmol. 2020;40(5):1085–1093. doi:10.1007/s10792-019-01271-w.
- Ucar F, Cetinkaya S. Xen implantation in patients with primary open-angle glaucoma: comparison of two different techniques. Int Ophthalmol. 2020;40(10):2487–2494. doi:10.1007/s10792-020-01427-z.
- Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–26. doi:10.1016/j.ajo.2017.07.023.
- Panarelli JF, Yan DB, Francis B, Craven ER. XEN gel stent open conjunctiva technique: a practical approach paper. Adv Ther. 2020;37(5):2538–2549. doi:10.1007/s12325-020-01278-1.
- Mansouri K, Guidotti J, Rao HL, et al. Prospective evaluation of standalone XEN gel implant and combined phacoemulsification-XEN gel implant surgery: 1-year results. J Glaucoma. Feb 2018;27(2):140–147. doi:10.1097/IJG.0000000000000858.
- Jones J, Koch DD, Vold S, et al. Results from the United States cohort of the HORIZON trial of a schlemm canal microstent to reduce intraocular pressure in primary open-angle glaucoma. J Cataract Refrac Surg. 2019;45(9):1305–1315. doi:10.1016/j.jcrs.2019.03.024.
- Laspas P, Garcia-Feijoo J, Martinez-de-la-casa JM, et al. Three-year results of hydrus microstent with phacoemulsification. Ophthalmology Glaucoma. 2019;2(6):440–442. doi:10.1016/j.ogla.2019.08.006.
