ABSTRACT
Purpose
To report rapid resolution of corneal clearing with the application of a modified technique of compression sutures in large hydrops.
Methods
Interventional case series of seven patients.
Results
Three patients had acute hydrops secondary to keratoconus, three had pellucid marginal corneal degeneration and another one had ectasia of undetermined etiology. A thorough slit-lamp evaluation and anterior segment optical coherence tomography was performed. The surgical technique involved paracentesis, anterior chamber decompression, compression suture placement within the stroma against the background of partial air fill in the anterior chamber, and bandage contact lens application. All eyes showed a remarkable reduction in corneal edema at 1 h (documented in four eyes) and 1 day (documented on the rest), which continued to improve in further follow up.
Conclusions
The modified technique of compression sutures facilitate rapid recovery of corneal edema in acute hydrops seen in keratoconus and pellucid marginal corneal degeneration. The physiologic basis is akin to the external tamponade achieved with buckle in retinal detachment surgeries.
Introduction
Acute hydrops occurs due to a sudden split in the Descemet membrane and Dua-Fine layer resulting in the ingress of aqueous within the corneal stroma.Citation1,Citation2 A large tear can result in near-total corneal edema that may either take several months to resolve or sometimes may not resolve. Prolonged edema in the peripheral cornea is an inciting stimulus for corneal vascularizationCitation3 that may pose challenges for future visual rehabilitation in cases where keratoplasty is required.
Several different approaches to the management of hydrops have been described.Citation4 Conservative management with topical hypertonic saline, steroids, and anti-glaucoma medications is traditionally advocated in most eyes and is generally practiced for more minor tears with a limited area of corneal edema.Citation5 Descemetopexy using long-acting gases, such as perflurocarbon (C3F8) and sulfur hexafluride (SF6) in iso-expansile concentrations (14% and 20%, respectively), has variable success in faster resolution of edema and is indicated in hydrops with small-sized tears.Citation6 The efficacy of long-standing gases is attributed to uncurling of detached Descemet membrane and subsequent migration of endothelial cells to the defect area that occurs with time.Citation7 Another surgical intervention that is proposed is full thickness compression sutures with or without intracameral long-acting gases.Citation8–10
We herein, report seven patients with large area of corneal hydrops who showed a dramatic resolution of corneal edema (characterized by the restoration of corneal clarity within a day) with a modified technique of compression sutures. Further, we have attempted to describe and explain the mechanism of rapid resolution of edema with the placement of compression sutures in cases with a large area of hydrops.
Materials and Methods
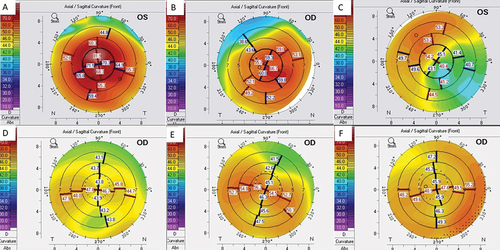
The study aims to describe the early postoperative outcomes of compression sutures in the management of corneal hydrops in seven patients. Three patients (Patients 1, 2, and 5) had hydrops secondary to keratoconus, three (Patients 4, 6, and 7) had pellucid marginal corneal degeneration, and one patient (Patient 3) had corneal ectasia of undetermined etiology (ectasia associated with posterior lamellar opacification). shows the corneal topography (Oculyser) of the unaffected eyes of the six patients (one patient, Patient 5, could not cooperate for the investigation). Slit-lamp evaluation and anterior segment optical coherence tomography (Optovue OCT, Inc., Fremont, CA) was performed to characterize the edema, pachymetry and localize the site of tear whenever possible prior to surgical intervention.
Figure 1. (a-f): Corneal topography of the contralateral eye of the patients; a- Patient 1, b-Patient 2, c-Patient 3, d-Patient 4, e-Patient-6, f-Patient 7 (Patient 5 with Down’s syndrome could not cooperate for topography).
Surgical Technique
Four patients (Patients 2, 4, 6, and 7) had surgery under local anesthesia, and three (Patients 1, 3, and 5) were operated on general anesthesia. A paracentesis was made to decompress the anterior chamber, and a small amount of air was injected to ascertain the level of the posterior membrane. The placement of compression sutures was based on the pattern of corneal edema and presumed localization of posterior membrane tear as noted on clinical slit-lamp findings. In three patients with keratoconus, the sutures were placed in an arcuate manner (alignment directed parallel to limbus), starting from the peripheral cornea inferiorly to the center, while in the other three patients with pellucid margin corneal degeneration, the sutures were placed radially to approximate the crescentic breach in posterior membrane. Care was taken to apply the compression sutures within the stromal tissue and not the posterior membrane. This was guided by the air reflex in the anterior chamber. After the placement of compression sutures, the air bubble was checked for mobility across the angles circumferentially. A small air bubble of size ~25–30% was left behind in the anterior chamber, and a bandage contact lens was placed at the end of surgery. Supine position was advised for approximately 30–45 min postoperatively. Slit-lamp photography was taken after 1 h in four eyes and postoperative day 1 in the rest others. In the follow-up period, the compression sutures were removed when loosening was noted and all sutures were out when edema resolved completely and scarring was noted.
The clinical detail of each patient is described.
Patient 1 ()
An 11-year-old boy with keratoconus () presented with acute hydrops of threedays duration (). He was initially treated with topical steroids and anti-glaucoma medications. However, at one month, a significant worsening of corneal edema that progressed to involve near-total cornea was noted (). The child underwent corneal compression suturing surgery under general anesthesia. After an initial paracentesis and anterior chamber decompression, a partial air fill was performed to guide the depth of sutures. Several compression sutures were taken in an arcuate manner from peripheral to central cornea at 4, 6, and 8 clock areas. In the end, a small air bubble of ~25% anterior chamber volume was retained. On first postoperative day 1 (), the peripheral corneal edema cleared remarkably. A small air bubble of <10% anterior chamber volume was present superiorly. The edema continued to resolve rapidly at five days after intervention () and thereafter. The serial optical coherence tomography corresponding to clinical images 2, A-D are presented in , respectively.
Figure 2. (a-c)- a: Slit-lamp photograph of the right eye when patient presented with a three-day history of acute hydrops; b: Slit-lamp photograph of the right eye after one month of conservative management showed marked increase in corneal edema; c: Slit-lamp photograph at first postoperative day showing rapid clearing of the peripheral cornea; d: Clinical picture on the fifth postoperative day showing further clearing of peripheral cornea. The optical coherence tomography pictures at first visit, one month after conservative treatment, postoperative day 1 and day 5 are depicted in e, f, g, and h, respectively.
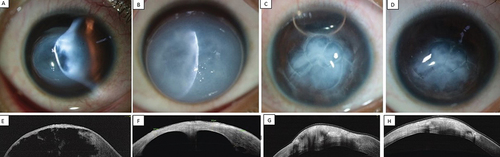
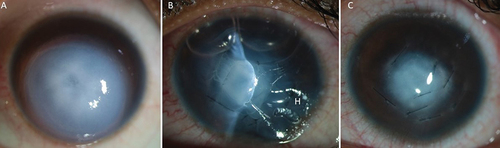
Patient 2 ()
A 16-year-old girl with keratoconus () presented with acute hydrops in the right eye of fourdays duration. She had descemetopexy with C3F8; however, an increase in edema was noted at oneweek (). She was undertaken for compression sutures under local anesthesia. After a paracentesis, a small amount of air was injected into the anterior chamber to gauge the depth of anterior stroma. Compression sutures were applied from peripheral to central cornea in an arcuate manner. The patient was positioned supine for 30 min postoperatively. Clinical slit-lamp photographs and anterior segment OCT performed at 1 h after the procedure showed significant resolution in the peripheral cornea (). The peripheral corneal edema cleared remarkably on the first postoperative day () and continued to clear in the follow-up period.
Patient 3 ()
An 8-year-old boy presented with complaints of a sudden loss of vision and whiteness in his eye following an injury with a ball twoweeks ago. Clinical slit-lamp examination revealed diffuse corneal edema and a circumferential area of transparency in the mid-peripheral cornea (). Anterior segment OCT showed dehiscence at the posterior membrane level corresponding to the circular area of stromal transparency. The other eye of the patient revealed thin cornea, ectasia () associated with posterior lamellar opacification. The edema progressively increased in a week. Compression sutures were applied radially to approximate the edges of circumferential split at Descemet membrane plane. On postoperative day 1 () a significant reduction in corneal edema was noted that resolved completely at oneweek ().
Figure 4. (a-f)- a: Slit-lamp photograph of the right eye when patient presented with a two-week history of increasing hydrops following blunt injury. The mid peripheral cornea shows circular area of differential transparency corresponding to posterior membrane dehiscence; b: Slit-lamp photograph of the right eye on first postoperative day shows remarkable resolution of corneal edema; c: Slit-lamp photograph at 1-week postoperative period shows improvement in corneal clarity; d-f: The corresponding optical coherence tomography pictures at pre-op, day 1 and 1 week are shown in d, e, and f, respectively.
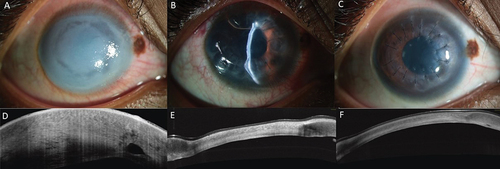
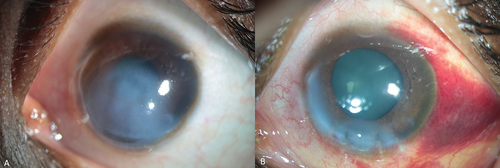
Patient 4 ()
A 27-year-old female presented with sudden whiteness and reduced vision in the left eye for 10 days. Clinical examination revealed corneal edema due to acute hydrops localized to three-fourth of the cornea. An crescentic peripheral tear could be appreciated (differential reflex noted) on slit-lamp evaluation (). Anterior segment OCT showed increased corneal thickness due to the stromal fluid (). The opposite eye showed peripheral thinning and ectasia suggestive of pellucid marginal degeneration (). Seven radial compression sutures were applied. Slit-lamp photographs captured 1 h after the procedure showed reduced corneal edema (). Next day, the cornea cleared remarkably with a clear visual axis ().
Figure 5. (a-f)- a: Slit-lamp photograph of the right eye when patient presented with a 10 days history of spontaneous hydrops shows an area of differential transparency in the mid periphery; b: Slit-lamp photograph of the right eye 1 h after the surgery shows remarkable reduction of corneal edema; c: Slit-lamp photograph on the first postoperative day shows clear visual axis; d-f: The corresponding optical coherence tomography pictures at pre-op, 1 h and 1 day are shown in d, e, and f, respectively.
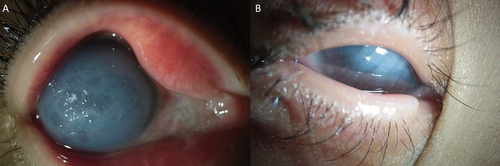
Patient 5 ()
A 13-year-old female with Down syndrome presented with sudden whitening in the right eye. The parents reported that the patient was habituated to rubbing her eyes. External torchlight examination was performed as patient was reluctant for slit-lamp evaluation. Clinical diagnosis of acute hydrops involving near-total cornea () was made. Compression sutures were taken from peripheral to central cornea, followed by tarsorrhaphy to retain the bandage contact lens. The external digital photograph of the right eye on first postoperative day showed resolution of peripheral corneal edema ().
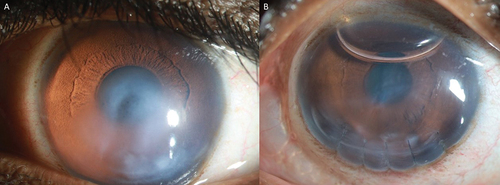
Patient 6()
A 42-year-old female complained of sudden loss of vision in the left eye of fourdays duration. At presentation, her visual acuity was hand motions in the left eye. The left eye showed hydrops that involved the visual axis (). The other eye showed a peripheral thinning inferiorly and topography was suggestive of pellucid marginal degeneration (). Compression sutures were applied radially in the peripheral cornea. The clinical picture at 1 h after the surgery showed a marked resolution of central corneal edema ().
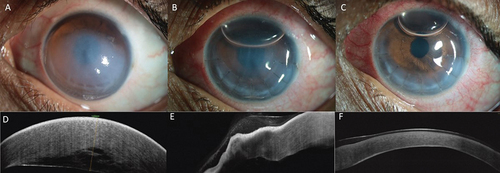
Patient 7()
A 31-year-old male complained of sudden loss of vision in the left eye of twodays duration. At presentation, his visual acuity was hand motions in the left eye. The left eye showed hydrops that involved the visual axis (). The other eye showed a peripheral thinning inferiorly and topography was suggestive of pellucid marginal degeneration (). Compression sutures were applied radially in the peripheral cornea. The clinical picture at 1 h after the surgery showed a marked resolution of central corneal edema ().
Discussion
The goal of any surgical intervention in management of acute hydrops is to resolve the edema in the shortest time. The surgical technique described here involved partial air fill (with 100% air composition) in delineating the depth better, and only a small amount of air (~30%) was retained after surgery, which reduced to <10% on the first postoperative day. Using long-acting pneumatic tamponade gases or complete anterior chamber with air fill alone in large acute hydrops has not been reported to show a response in a day. Further, the disadvantage of descemetopexy with the long-acting gases is the propensity to cause pupillary block and raised intraocular pressure that could lead to other complications such as fixed dilated pupil and cataract.Citation7 In such cases, a surgical peripheral iridectomy is required, which can be avoided in the currently described technique. Besides, prolonged air contact with posterior corneal surface can have endothelial toxicityCitation11 and accelerate cataractogenesis. Also, the tamponade gases may not be effective in those with a large area of tear, especially when it exists in the inferior mid-peripheral parts of cornea.
The dramatic resolution of peripheral corneal edema in the initial 1 h (documented in four eyes, Patients 2, 4, 6, and 7) and first postoperative day (as documented in the remaining eyes) and rapid resolution over the next few days, occurred due to a combination of several factors. We believe the most critical factor in these cases was the placement of compression sutures against the background of the anchoring air bubble during surgery. Compression sutures help bring the edematous and biomechanically weak cornea in closer proximity to the endothelial layer, thereby facilitating the natural process and endothelial pump mechanism of fluid absorption. As the peripheral anterior chamber depth is shallow, the placement of compression sutures in the peripheral part of the cornea in large hydrops reduces the depth of separation of posterior membrane from anterior cornea. The physiological mechanism of efficacy of compression sutures is analogous to external tamponade performed using the scleral buckle in retinal detachment surgeries and air bubble in anterior chamber facilitating this process.
The orientation of compression sutures in the patients described here, depended on the nature of ectatic condition, and the presumed localization of the posterior membrane split. In keratoconus, the posterior membrane break is most likely in the central or paracentral cornea, compared to Pellucid marginal degeneration where it is crescentic in the peripheral cornea. Hence, in keratoconus with hydrops involving the peripheral cornea, the suture placement was done from periphery to center aligning the sutures parallel to the limbus, whereas the sutures were placed radially in eyes with Pellucid marginal degeneration. The application of compression sutures has been described in the management of hydrops. The distinct features of the present technique and study are:
Rapidity of corneal clearance in an hour after the surgery (four eyes) and one day in remaining others. The slit-lamp photography was captured at 1 h after the surgery in four eyes and on day 1 in the rest others.
The technique of compression sutures is effective in Pellucid marginal corneal degeneration.
The technique of compression sutures is modified to partial thickness sutures in the stroma and minimal use of air (<1/3rd) in anterior chamber, without the use of C3F8 gases. This eliminates the gas bubble-related complications in the immediate postoperative period.
While most cases of acute hydrops resolve gradually with observation alone, surgical intervention with compression sutures to hasten the resolution of hydrops should be considered, especially in large area of corneal involvement that extends to the peripheral cornea. Rapid resolution of edema will help in quicker visual rehabilitation and prevent development of corneal vascularization associated with long-standing peripheral edema.
Author Contributions
The corresponding author states that authorship credit of this manuscript was based on 1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the version to be published. All listed authors met conditions 1, 2, and 3. All persons designated as authors qualify for authorship, and all those who qualify are listed. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Dua HS, Sinha R, D’Souza S, et al. “Descemet membrane detachment”: a novel concept in diagnosis and classification. Am J Ophthalmol. 2020;218:84–98. doi:10.1016/j.ajo.2020.05.038.
- Yanoff M, Sassani J. Cornea and sclera, normal anatomy. In: Yanoff M, Sassani J, eds. Ocular Pathology E-book. 8th ed. US: Elsevier; 2019:272–274.
- Rowson NJ, Dart JK, Buckley RJ. Corneal neovascularisation in acute hydrops. Eye (Lond). 1992;6(Pt 4):404–406. doi:10.1038/eye.1992.83.
- Fan Gaskin JC, Patel DV, McGhee CN. Acute corneal hydrops in keratoconus - new perspectives. Am J Ophthalmol. 2014;157(5):921–928. doi:10.1016/j.ajo.2014.01.017.
- Tuift SJ, Gregory WM, Buckley RJ. Acute corneal hydrops in keratoconus. Ophthalmology. 1994;101:1738–1744. doi:10.1016/S0161-6420(94)31110-9.
- Maharana PK, Sharma N, Vajpayee RB. Acute corneal hydrops in keratoconus. Indian J Ophthalmol. 2013;61(8):461–464. doi:10.4103/0301-4738.116062.
- Basu S, Vaddavalli PK, Ramappa M, Shah S, Murthy SI, Sangwan VS. Intracameral perfluoropropane gas in the treatment of acute corneal hydrops. Ophthalmology. 2011;118(5):934–939. doi:10.1016/j.ophtha.2010.09.030.
- Rajaraman R, Singh S, Raghavan A, Karkhanis A. Efficacy and safety of intracameral perfluoropropane (C3F8) tamponade and compression sutures for the management of acute corneal hydrops. Cornea. 2009;28(3):317–320. doi:10.1097/ICO.0b013e31818ada0b.
- Subudhi P, Khan Z, Subudhi BNR, Sitaram S. To show the efficacy of compressive sutures alone in the management of acute hydrops in a keratoconus patient. BMJ Case Rep. 2017 May 4;2017:bcr2016218843. doi:10.1136/bcr-2016-218843.
- Vajpayee RB, Maharana PK, Kaweri L, Sharma N, Jhanji V. Intrastromal fluid drainage with air tamponade: anterior segment optical coherence tomography guided technique for the management of acute corneal hydrops. Br J Ophthalmol. 2013;97(7):834–836. doi:10.1136/bjophthalmol-2013-303272.
- Kopsachilis N, Tsaousis KT, Tsinopoulos IT, Welge-Luessen U. Air toxicity for primary human-cultured corneal endothelial cells: an in vitro model. Cornea. 2013;32(4):e31–5. doi:10.1097/ICO.0b013e31826895f8.