ABSTRACT
Purpose
We conducted a systematic search of literature to understand the various methods of imaging of the ciliary body.
Methods
PubMed, Science Direct, Cochrane Library and Google Scholar were searched comprehensively and systematically to find studies related to the various modalities of ciliary body imaging.
Results
The various ciliary body parameters that have been described are Ciliary body thickness, Ciliary body length, ciliary muscle thickness, ciliary process length, ciliary muscle length, ciliary muscle anterior length, trabecular ciliary process distance and Iris ciliary process distance. The various angles which have been measured, which mostly have a significance in Primary angle closure glaucoma (PACG) are Iris ciliary angle, Trabecular ciliary angle, scleral ciliary process angle. Various authors have defined them in various ways with subtle differences. Plateau iris and PACG mechanisms, not forgetting malignant glaucoma are better understood with imaging of the ciliary body using the ultrasound biomicroscopy (UBM). The anterior segment optical coherence tomography (ASOCT) imaging of the ciliary body has been described albeit with its own disadvantages. A few other fields dependant on the importance of ciliary body imaging are intravitreal injections, pars plana vitrectomy, measurements for implantable collamer lens (ICL) and of utmost importance, the differentiating features of ciliary body masses.
Conclusion
The UBM is still preferred over the ASOCT for imaging of the ciliary body. A lot of lacunae of knowledge still exists and consensus has to be reached on defining all the parameters universally. Future studies will be able to shed more light on the role of the ciliary body in the many ocular disorders mentioned in this review.
INTRODUCTION
Imaging of the ciliary body, along with the surrounding structures, is something which still eludes ophthalmologists. Autopsy measurements of the ciliary body, unlike in-vivo measurements, show a variation in ciliary body length (CBL) of 4.5–6.3 mm and are therefore not reliable.Citation1 The ultrasound biomicroscopy (UBM) was developed by Pavlin et al. in the 1990s.2Citation2 It uses a frequency of 35–100 MHz, unlike the usual B-scan frequency of 10 MHz. It has varied utility in evaluating various conditions of the eye, ranging from the ocular adnexa to the anterior vitreous and the adjoining retina. It’s major role is in the field of glaucoma, aiding in the identification of the various mechanisms of angle closure, plateau iris syndrome and malignant glaucoma.Citation3–6 It’s crucial role in the diagnosis of ocular neoplasms cannot be omitted. However, there are more questions than answers till date.
The boon of the UBM is that it has helped us to have a glimpse of the ciliary body, albeit the lower resolution compared to the anterior segment optical coherence tomography (ASOCT). Newer spectral domain ASOCT has however been able to measure the CBL but with its own limitations.Citation7
To study pathologic changes, normative values are a necessity. Carrying out measurements in normal eyes can aid in determining and differentiating the normal from the abnormal. Quite a few studies on normative data for ciliary body have been conducted.Citation8,Citation9 Their main drawbacks include ethnical differences, effect of accommodation on CB parameters, no standardized settings for lighting of the examination room and intra and inter-observer variations.
A few other fields, that benefit from ciliary body imaging, are precision for intravitreal injections, pars plana vitrectomy (PPV) and microincision vitrectomy surgery (MIVS).Citation7,Citation8,Citation10 Not to forget the importance of sulcus to sulcus (STS) measurements for planning implantable collamer lenses (ICL), and for assessing the position of glued or scleral fixated intraocular lenses.Citation11,Citation12 The knowledge of the precise parameters of CBL and ciliary body thickness (CBT) would prevent accidental trauma to the crystalline lens and retina during these procedures.Citation8
An evil and a boon, the UBM being a contact procedure, which is operator dependent, is however still capable of giving an insight into the structures behind the iris and shed some light on the role they have to play in anterior chamber angle dynamics. Qualitative examinations have added to the sea of knowledge but they are bound down by reduced reproducibility. While quantitative ones may overcome one hurdle another comes in the way of the iris and ciliary body being mobile structures. This mobility may be somewhat diminished by maintaining near perfect dark room conditions or attempting to control accommodation. With these and the many more benefits and drawbacks of this imaging we intend to analyze the different methods of obtaining the scan. Various authors have defined different parameters and we have enlisted them to give us a better insight on the most ideal and appropriate technique with the most suitable conditions to give us a good quality image of the ciliary body, an enigma waiting to be unravelled.
METHODS OF LITERATURE SEARCH
PubMed, Science Direct, Cochrane Library and Google Scholar were searched for relevant keywords. The search string included one or a combination of the following terms: ultrasound biomicroscopy, ciliary body, ciliary processes, ciliary muscle, anterior chamber angle, ciliary body imaging, ciliary body glaucoma, angle closure glaucoma, normal ciliary body, secondary glaucoma, laser peripheral iridotomy, plateau iris syndrome, malignant glaucoma, ciliary body diabetic retinopathy, ciliary body myopia, ciliary body accommodation, ciliary body hypermetropia, ciliary body transscleral cyclophotocoagulation, anterior segment optical coherence tomography ciliary body, ASOCT ciliary body, spectral domain ASOCT ciliary body and ICL vault ciliary body.
The publication years of the articles were from 1991 to 2021. Furthermore, a manual search on the references of a few selected articles was also done. In this review we focused on the various methods employed for obtaining the scans, the various inclusion and exclusion criteria by the authors and the relevant and important parameters of the ciliary body which were measured. We also delved into the results obtained by various authors and how these results are relevant in clinical scenarios. Finally, the limitations were set down and in the future directions, we argue that more research and studies are warranted to better understand the role of the ciliary body in various ocular conditions, especially in various glaucomas.
OBSERVATIONS
Methods of Examination of Subjects
Normal subjects recruited were either medical students, physicians or patients who would come for a routine check-up.Citation8 Various exclusion criteria were of course highly dependent on the aim of the study but most studies would exclude subjects with a history of any ocular disease (except for refractive error), a history of having undergone various laser procedures (excluding studies which studied post laser peripheral iridotomy),Citation3,Citation5 any intraocular surgeries (excluding studies of malignant glaucoma, post ICL, post PPV, post transscleral cyclophotocoagulation, TSCPC), those giving a history of trauma to the eye, systemic diseases that may affect visual function, use of systemic or ocular medication (excluding some studies where topical glaucoma medications were considered),Citation8,Citation10,Citation11 uveitis, inflammatory connective tissue disorders, history of intravitreal steroid or anti-vascular endothelial growth factor (anti-VEGF).Citation10 Studies related to accommodation excluded patients with refractive errors greater than +6.00 DS or −10.00 DS, and/or oblique cylinders >0.50 DC or orthogonal cylinders >1.50 DC.Citation13
All studies preferably performed examinations with the patient in the supine position, to negate any effects of gravity on the findings. Topical anaesthetic eyedrops are a must in UBM imaging, as it is a contact procedure. The anaesthetic agent used was 0.5% proparacaine. An immersion cup (rubber) was essential to immerse the UBM probe and firm pressure was required to inhibit leakage of fluid during the examination. The fluid filled in the immersion cup varied from normal saline to 2% methyl celluloseCitation14 or contact lens solution.Citation9 In a majority of the studies, the probe frequency used was 50 MHz,Citation3–5,Citation12,Citation14–21 a small proportion however using, 359,Citation10 and 30 MHz.Citation8 The higher frequency 50 MHz probe does have the disadvantage of a decreased penetration as compared to the 35 MHz or 30 MHz probe but has the advantage of better resolution. In all studies, the probe was placed in the radial or longitudinal position, at 3, 6, 9 and 12 o clock, for capturing the images. Additionally, some authors chose to perform a central scan at the centre of the cornea.Citation8 Following this, in-built calipers were employed for taking measurements. In most studies, a target was placed in the ceiling for fixation with the other eye. Jiang et al., went a step further by fixing five fluorescent papers as ceiling targets to standardize the measurements for the different examinations of all quadrants (12, 3, 6 and 9 o’ clock positions).Citation22 A good scan would include the scleral spur, the angle and the ciliary body.Citation17,Citation22
A study evaluating CBL using spectral domain ASOCT did not take the four clock hours mentioned above but chose the superotemporal (ST), inferotemporal (IT), superonasal (SN) and inferonasal (IN) quadrants and did so by making the participants fixate at a light that was moved from one of the quadrants stated above, to the next quadrant.Citation7
Accommodation, a confounding factor, was relaxed by asking the subjects to fixate on a given point on the ceiling, with authors even going to the extent of correcting the refractive error of the other eye with appropriate contact lens.Citation8 Muftuoglu et al, in their study, relaxed accommodation with the aid of cyclopentolate 1% and performed the examination after 40 mins.Citation14 To minimise intra and inter-observer variation, authors have appointed only one observer, who is usually a trained individual involved in performing ocular ultrasonographies for a long period of time.Citation4,Citation9,Citation10,Citation14,Citation20,Citation23,Citation24 The technique of employing two blinded observers to analyze images was also applied by some authors.Citation7,Citation8,Citation12,Citation17,Citation22,Citation25 Another method, was by averaging 3 measurements for each quadrant, all performed by two independent examiners.Citation7 Some authors however, did not mention the number of observers.Citation18,Citation19,Citation26,Citation27 In , we have summarized the interclass correlation coefficient (ICC) and kappa values from these studies.
Table 1. Table showing interclass correlation coefficient, percentage agreement and κ value used by various authors.
Illumination of the Examination Room
In , we have listed the various illuminance employed by different authors. Normal luminance of a room is approximately around 150–200 lux.Citation28 Therefore it would be ideal to perform UBM procedures in luminance of less than 150 lux.
Table 2. Table showing the illuminance used by various authors.
Ciliary Body Parameters
There is considerable disparity in the definition and quantification of ciliary body parameters in the multitude of studies that have been reviewed. The various parameters and the methods of measurement are in . An important landmark, the scleral spur is located by delineating the part where the radiolucent cornea integrates with the radio-opaque sclera.
Table 3. Table showing the different ciliary body parameters, with their definitions according to various authors.
Ciliary Body Thickness (CBT) and Ciliary Body Length (CBL)
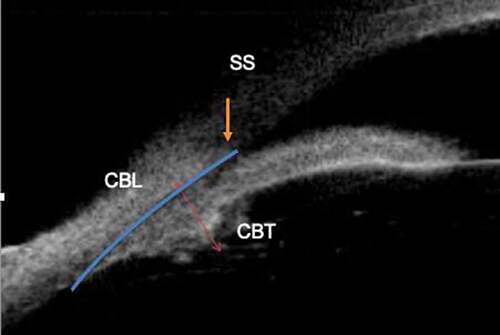
As seen from and , most authors measured CBT as the perpendicular distance from the inner sclera to the apex of the ciliary body,Citation9,Citation12,Citation17,Citation21,Citation22 whereas Muftuoglu et al.Citation14 measured it as the distance from the sclera to the tip of the ciliary process, the difference between the two being that Muftuoglu et al. had an additional measurement of the ciliary process. CBT1, CBT2 and CBT3 are the perpendicular distances measured from points 1 mm, 2 mm and 3 mm posterior to the scleral spur whereas Marchini et al.Citation19 took these distances as 1500 microns, 2000 microns and 2500 microns from the scleral spur, these measurements being important during accommodation. These 500 microns differences may be a source of error while conducting various accommodation studies and have to be standardized.
CBL in UBM
CBL has been taken as a section of the arc passing through the scleral spur and the posterior end of the ciliary body by Okamoto et al.Citation8 ( and ).
CBL in ASOCT
Lincke et al.Citation7 measured CBL as a straight line distance from the scleral spur and the posterior end of the ciliary body ( and ). CBL is shorter by 2 mm by this method. The most probable reason for this could be that Lincke et al.Citation7 used the iridocorneal angle as the starting point of their measurement which is more posterior to the scleral spur, as used by Okamoto et al.Citation8 It can also be attributed to the poor visibility in OCT beyond a certain point, which may have led the authors to exclude the pars plana while measuring the CBL. Further comparative studies are required to quell this debate and exactly determine CBL and other ciliary body parameters and decide the appropriate method, be it UBM or ASOCT, to accurately estimate these parameters.
CBL and CBT are more in the superior quadrant as compared to the inferior quadrant of the eye. Okamoto et al have attributed this finding to the differential growth of the eyeball, during the period of development, growing from top to bottom, a fact which is supported by the evidence of colobomas being presently inferiorly ().Citation8 Considering the significantly longer CBL and CBT superiorly, it would be imperative to stress on the fact that anti-vascular endothelial growth factor (anti-VEGFs) are safer when injected superiorly. As much as a difference of 0.77 mm in mean CBL was seen between short axial length (AL) and long AL. Therefore, scleral tunnels for vitreo-retinal surgery should be made taking into account CBL and the fastest most accessible indirect method to estimate this would be AL.
Table 4. Ciliary body thickness (CBT) and ciliary body length (CBL) in normal individuals.
Ethnicity also defines CBT, with Caucasians having thicker ciliary body as compared to Chinese.Citation24 Thicker ciliary body was also seen in longer AL,Citation24 thicker iris,Citation10 increased CBL,Citation10 thicker lens,Citation4 and deeper anterior chamber (AC).Citation10 The greater the CBL the deeper the AC,Citation8 the longer the AL.Citation7 CBT and CBL are also positively correlated with age ().Citation7,Citation9
Table 5. Trabecular ciliary process distance (TPCD), Trabecular ciliary angle (TCA) and Scleral ciliary process angle (SCPA).
Table 6. Significant results related to CBT and CBL of normal subjects.
Ciliary Muscle Parameters and Accommodation
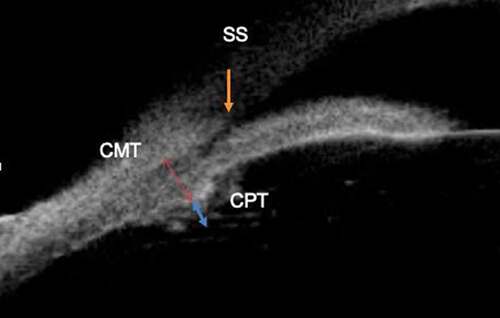
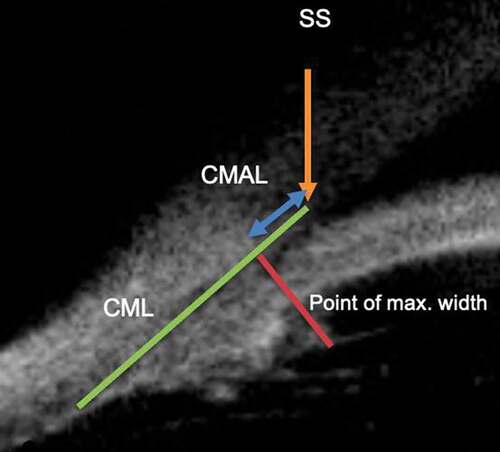
Ciliary muscle thickness (CMT) as seen in and has been mainly defined as the thickness of the ciliary body excluding the ciliary processes.Citation13,Citation23 It is an important measure for accommodation studies, and has been defined and measured differently by various authors, Muftuoglu et al.Citation14 and Safwat et al.Citation26 measured it from the base of the ciliary process to the sclera.
Ciliary Muscle Parameters on ASOCT
Sheppard et al.Citation13 specified CMT at various points (CM25, CM50, CM75), as the width of the muscle determined at points that fell 25%, 50% and 75% of the total length posterior to the scleral spur ( and ). These points have been selected because of already existing data on the anterior shifting that occurs during accommodation.Citation29 CM2 is measured from a point 2 mm from the scleral spur. CM2 being taken as it has been shown in previous workCitation30 to have a negative correlation with refraction in children. Ciliary muscle length (CML) and Ciliary muscle anterior length (CMAL) have only been defined by Sheppard et al.Citation13 in their ASOCT study of accommodation with CML being measured from the scleral spur to the posterior visible limit and CMAL as the length being measured from the point of maximum width of the ciliary body to the scleral spur ( and ). Sheppard et al.Citation13 with their findings of a decrease in anterior length of the ciliary muscle and an increase in CM25 thickness, concluded that during accommodation, there is an anterior and inward shift of the ciliary muscle.Citation31,Citation32 This was further substantiated in children as well,Citation23,Citation33,Citation34 validating that the contraction of the anterior circular fibres of the ciliary muscle are responsible for accommodation. Studies have shown also that ciliary muscle width is more during childhood as compared to adults.Citation35
Figure 3. Figure depicting ciliary muscle thickness at the levels of CM25, CM50 and CM75, as the width of the muscle determined at points that fell 25%, 50% and 75% of the total length posterior to the scleral spur. SS:scleral spur.
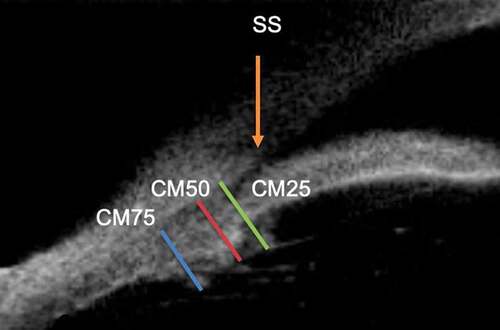
Figure 4. Figure depicting ciliary muscle length (CML) and ciliary muscle anterior length (CMAL). SS: scleral spur.
Studies related to accommodation have used near targets (Maltese cross) in ASOCT, at an angle of 40°, to enable imaging of the ciliary body. For accommodation, a stimulus vergence level of −4D and −8D were used and for distance −0.19D with the help of a mirror to make it into a distant target.Citation13 The variation in the parameters of the ciliary body between nasal and temporal aspects in terms of length, width and accommodative response could have an impact on future research on accommodating intraocular lenses and may be related to the physiology of convergence.Citation36
Plateau Iris and PACG
PACG forms a major chunk of the total cases in glaucoma in the Asian region.Citation37 Post laser peripheral iridectomy (LPI) (the standard of care), the persistence of raised IOP and advancing glaucoma still plagues most ophthalmology clinics substantiating the fact that pupillary block isn’t the sole mechanism for PACG. Non-pupillary block mechanisms are not as uncommon as previously thought.Citation38,Citation39 Plateau iris syndrome (PIS) accounting as one of the non-pupillary block mechanisms, exhibits a deep anterior chamber centrally with the presence of anteriorly located ciliary processes pushing the peripheral iris forward leading to narrowing of the angle recess.Citation40 PIS is diagnosed post iridotomy, whereas plateau iris configuration is diagnosed pre iridotomy.Citation41 There are however, conflicting reports about central anterior chamber depth (ACD) and plateau iris, with some claiming that the ACD is more shallow in these cases rather than in pupillary block or normal subjects.Citation42,Citation43 The presence of a large ciliary body and anteriorly placed ciliary processes are said to be the two properties of plateau iris (non-pupillary block) mechanisms for angle closure.Citation44 With the advent of the UBM it has made the diagnosis of plateau iris syndrome (PIS) more objective, also showcasing the anteriorly positioned ciliary processes and absent ciliary sulcus.Citation5 Initially thought to be a rare entity, PIS is being increasingly diagnosed, with cases being as high as 66.66%Citation3 or 32.4% of the angle closure glaucomas.Citation5 In fact, Kumar et al., noted that PIS diagnosed on UBM were not diagnosed clinically on gonioscopy.Citation5 Verma et al. have studied the prevalence of plateau iris in the 3 distinct subgroups of PACG that they had classified based on ASOCT findings.Citation45 Classifying a case as plateau iris was based on the presence of all the following characteristics in at least 2 quadrants; “(a) The ciliary process was anteriorly directed, supporting the peripheral iris so that it was parallel to the trabecular meshwork; (b) The iris root had a steep rise from its point of insertion, followed by a downward angulation from the corneo-scleral wall: (c) An absent ciliary sulcus: (d) Irido-angle contact (above the level of the scleral spur) in the same quadrant.”Citation45 The proportion of plateau iris in all the 3 distinct subgroups of PACG was found to be similar. PIS has also been seen in primary angle closure patients post LPI, consolidating the fact that it may be one of the probable causes of progression in PACG, in a large number of patients.Citation46 Prospective longitudinal studies are therefore required to follow up and understand the importance and implication of PIS and PACG.
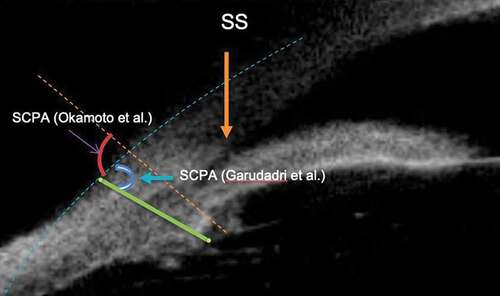
Parameters (in the form of angles and distances), help to measure the proximity of the ciliary body and its processes to the trabecular meshwork, angle of the anterior chamber and related structures. These parameters aid us in the better understanding of non-pupillary block mechanisms in PACG. Scleral ciliary process angle (SCPA) as defined by Okamoto et al.Citation8 and Marchini et al.Citation19 is the angle between the axis of the ciliary process and a line tangential to the sclera whereas Garudadri et al.Citation3 have defined it as the angle between two lines, one being a line joining the sclera and a ciliary process and the other going through the plane of iris to the sclera ( and ). Both being a measure of the proximity of the ciliary process to the sclera and how anteriorly rotated they are.
Figure 5. Figure depicting scleral ciliary process angle (SCPA) as described by Okamoto et al.Citation8 and Garudadri et al.Citation3 SS: scleral spur.
Another angle, Iris ciliary angle (ICA) has been defined by Chen et al.Citation12 as the angle between the posterior iris surface and the anterior surface of the ciliary body and Trabecular ciliary angle (TCA) as the angle measured by the scleral spur as the apex and the corneal endothelium and the anterior surface of the ciliary body as the arms.Citation12,Citation24 The more acute the angle in both, the more anteriorly angulated the processes are ( and ).
Figure 6. Figure depicting scleral ciliary process angle (SCPA), Trabecular ciliary angle (TCA), Iris ciliary angle (ICA), Trabecular ciliary process distance (TCPD) and Iris ciliary process distance (ICPD). SS: scleral spur.
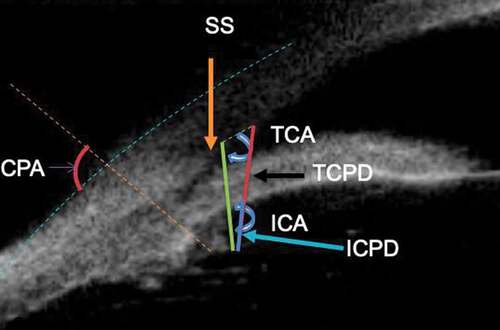
Trabecular ciliary process distance (TCPD) is the “length of the line extending from the corneal endothelium 500 µm from the scleral spur perpendicularly to the line passing through the innermost point of the ciliary body and parallel to the iris”,Citation12,Citation20,Citation21,Citation24 or “vertical Distance of a ciliary process to the tangent drawn from 500 microns anterior to the scleral spur.”Citation3 ( and ). Both essentially mean the distance of the trabecular meshwork from the ciliary process. Iris Ciliary Process Distance (ICPD), is the distance measured “from the posterior surface of the iris 500 microns anterior to the sclera spur toward the ciliary process” signifying a measure of the distance of the iris to a ciliary process.Citation21 Both TCPD and ICPD are supposed to give an estimation of the proximity of the ciliary processes to the trabecular meshwork or the iris, the latter representing the ciliary sulcus ( and ). Closer proximity and absent ciliary sulcus being linked to the pathogenesis of PACG or PIS.
Ciliary body position is another factor being studied in the pathogenesis of PACG. A study done in primary angle closure suspects (PACS) labelled ciliary body position as neutral or anteriorly positioned based on the direction of the axis of the ciliary body, from a pre-existing set of UBM images. The ciliary body was found to be anteriorly positioned in almost three-fourths of the cases.Citation22
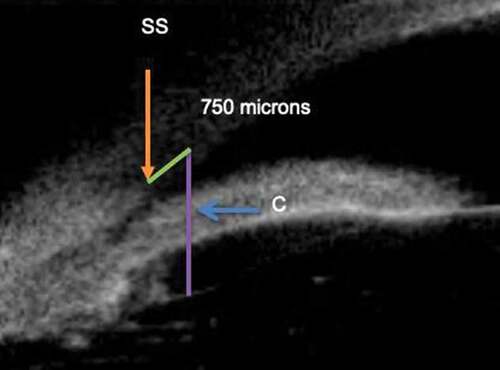
Sakata et al.Citation20 preferred to use the term “long ciliary process with no ciliary sulcus”, and not “anterior positioning of the ciliary processes”, as used by previous authors. They drew a line perpendicular to the plane of the iris and this line passed through a point 750 µm anterior to the scleral spur at the corneal endothelium (). A long ciliary process was defined as one whose length crossed this line, and the ciliary sulcus was said to be absent if the ciliary processes were opposed to the peripheral iris at this same location.Citation20 In their study, long ciliary process with absence of ciliary sulcus was seen not only in the appositional closure group but in the control group (32%) as well. With this, they came to a conclusion that long ciliary process associated with no ciliary sulcus is not the only factor for non-pupillary block mechanism as it is seen in cases with open angles as well. Additional factors like anterior positioning of the ciliary processes, ACD, AOD500 and TPCD play an important role.Citation20
Figure 7. Figure depicting the concept of long ciliary process. A line was drawn (line C) perpendicular to the plane of the iris and this line passed through a point 750 µm anterior to the scleral spur at the corneal endothelium. A long ciliary process was defined as one whose length crossed this line, and the ciliary sulcus was said to be absent if the ciliary processes were opposed to the peripheral iris at this same location. SS: scleral spur.
Garudadri et al.,Citation3 also had similar findings of the presence of anteriorly placed ciliary processes in open angles and posteriorly placed ciliary processes in narrow angles. Likewise, Jiang et al.Citation22 also found that eyes with open angles, possessed anteriorly placed ciliary bodies which were larger in size. Apart from the mechanisms stated above, Pavlin et al.,Citation47 described yet another mechanism, wherein the thinner atrophied ciliary body seen with age and in eyes with narrow angles, is the actual cause of anteriorly rotated ciliary processes. Sequentially, this brings about loosening of the zonules and with it an increase in the thickness of the lens with consequent shallow anterior chamber.Citation37 Ku et al. have however, stated that patients with larger CB have a higher likelihood of angle closure than small CB.Citation17 Further studies are required in this regard to accept or refute these findings and assumptions ().
Table 7. Significant results related to angle closure.
A lot of work still remains to ascertain the definite mechanisms behind PIS, not forgetting the fact that there is no proper quantification of how much anterior the position of the ciliary processes defines PIS and it is still subjective. Treatment options for this entity vary from laser iridoplastyCitation40,Citation48 to topical pilocarpine.Citation49,Citation50 We are yet to reach an accord on the number of quadrants of PIS features on UBM that are required for diagnosis. There is still no randomized controlled trial for the appropriate treatment for PIS and no fixed UBM characteristics for its proper diagnosis.
TSCPC and UBM
Safwat et al,Citation26 in their study wanted to highlight the changes in ciliary body parameters, especially in the ciliary processes, after TSCPC. Mean length of ciliary processes per field (MLCPPF) was defined as “the sum of heights of ciliary processes (measured from the tip to the base of the ciliary process in microns) per field divided by number of ciliary processes in the same field” and the mean width of ciliary processes per field (MWCPPF) as “the sum of widths of ciliary processes per field divided by number of ciliary processes per the same field”.Citation26 It was found that ciliary process length and width was positively correlated with IOP at 3 months of post TSCPC, signifying that the drop in IOP post TSCPC is proportional to the reduction in size of the ciliary processes. From their study, the main take away points were; the utility of the UBM to monitor the ciliary body and processes alterations post TSCPC, to titrate re-treatment by aiding in identification of segments which have already been treated and those segments which may have been missed previously.Citation26
Malignant Glaucoma
Being able to predict this vicious and blinding complication, would be a godsend for any ocular surgeon. As the ciliary body has been implicated as the predominant offender (anterior rotation), needless to say, its imaging by UBM in the pre-operative phase would help in prognosticating cases and in planning the surgery accordingly. One such study, examined patients who had developed malignant glaucoma post-surgery, and who already had a pre-operative UBM done.Citation15 For patients who had not undergone a pre-operative UBM, a scan of the other eye was taken into consideration. It was noted that 85% of the eyes had a plateau iris configuration pre-operatively and before the development of malignant glaucoma. The other 15% had narrow angles with a shallow anterior chamber.Citation15 Other short case series have also reported the presence of plateau iris configuration in patients as a risk factor of malignant glaucoma.Citation51,Citation52 Prata et al.,Citation15 have however mentioned a major drawback in their study; the retrospective nature and selection bias. This is so because the possibility of only patients with narrow angles undergoing UBM pre-operatively would be disproportionately higher. Wang et al.Citation53 collected retrospective data of PACG patients and compared it to patients who had developed malignant glaucoma. The CBT, TPCA and ACD were significantly lesser in the malignant glaucoma group as compared to PACG without malignant glaucoma.Citation53 In another study however, CBT was shown to be increased in malignant glaucoma as compared to PACG and normal subjects. A randomized controlled trial would be required to provide us with adequate and reliable risk factors for predicting malignant glaucoma.
Aniridia
Okamoto et al.Citation27 in their study of adult aniridia patients demonstrated that along with iris hypoplasia, there is significant ciliary body hypoplasia also, when compared with normal controls. The SCPA was also significantly narrower in aniridia patients, denoting that the ciliary processes were more anteriorly rotated in these patients. This would make them exhibit shallower anterior chambers with an increased risk of malignant glaucoma. Many theories on the mechanism of glaucoma in aniridia have been put forth,Citation54,Citation55 which include angle dysgenesis and/or angle closure by iris stroma strands. Okamoto et al.Citation27 have suggested that hypoplasia of the ciliary body, could be another factor for the development of glaucoma, with uveoscleral outflow having a part to play. Future studies on UBM are required to consolidate this.
Congenital Glaucoma
As compared to the non-glaucomatous myopic eyes, which have a larger CBT, eyes with congenital glaucoma have been shown to have significantly thinner CBTs, with a uniquely thin, ill-defined and “rarefied” ciliary body, most probably owing to the stretching of the coats of the eye ().Citation16,Citation56 Another atypical finding, was the emergence of a few ciliary processes directly from the posterior surface of the iris. This finding should caution one when making an iridectomy as it may lead to ciliary body injury and/or prolapse of vitreous.Citation16
Ciliary Body in DME
It has been noted, that like the macula, the ciliary body possesses VEGF receptors and it undergoes inflammatory changes in many pathological processes.Citation57,Citation58 It would be only reasonable to speculate that an inflammation of the retina and macula would be followed by inflammation of the ciliary body and its consequent thickening and increase in size. Post vitrectomy, macular oedema improves leading to a reduction in the central macular thickness and it has been shown to lead to an improvement of the ciliary body thickness as well.Citation10 Changes in the ciliary body accompanying diabetic macular oedema may help to establish the link between glaucoma and diabetes. Future studies may help in determining this correlation.
Effect of Topical Medications on Ciliary Body
UBM has been able to demonstrate the changes in the ciliary body after instillation of topical medications in the eye. Topical pilocarpine has been shown to increase the CBT significantly, the mechanism being ciliary body muscle constriction and topical cyclopentolate decreased the CBT significantly by an opposing mechanism of relaxing the ciliary body muscle.Citation18 Topical Latanoprost has been shown to decrease the CBT 4 hours after instillationCitation18 and to increase the CBT 1 week later, with the mechanism either being relaxation or extracellular matrix remodeling of the ciliary body.Citation19
ICL and Ciliary Body
Excessive vault post ICL implantation, an increased risk for angle closure glaucoma, has been on the rise, being approximately 0.4%-11.1%,Citation59 even though, all possible preventive measures have been taken including meticulous measurements of white to white (WTW), ACD and STS. This has led some to believe that there must be some other hidden anatomic factors responsible for this incidence, possibly parameters related to the ciliary body.Citation60 Chen et al.,Citation12 in their study, looked into ciliary body factors, like ICA, TCA, TCPD, CBT max and CP length. CP length as measured by Chen et al.Citation12 is “the distance from the innermost point of the ciliary body to the intersection point of the iris and ciliary body”. This parameter, correlated with Iris ciliary angle (ICA), and showed that a more anteriorly located ciliary body was usually associated with long ciliary processes. ICA (an indicator of ciliary sulcus), and STS seem to be important determinants of the ciliary sulcus.Citation12,Citation61 The conclusion of their study was that eyes that had a more anteriorly positioned ciliary body, had a higher risk of increased vault after implantation of ICL.Citation12 Risk of post ICL increased vault seems to be related to the discrepancy between WTW and STS. They argued that absence of ciliary sulcus with anteriorly positioned ciliary process may inhibit unfolding of the ICL haptic leading to an excessive vault. Further studies looking at the position of the ICL haptic in relation to the ciliary body need to be conducted.
Ciliary Body Masses
Benign lesions of the ciliary body include reactive hyperplasia, congenital masses, Fuch’s adenoma.Citation62–64 Acquired adenomas of the ciliary body epithelium (ACE) have been classified into adenomas of the pigmented ciliary body epithelium (APCE) and adenomas of the pigmented ciliary epithelium (ANPCE).Citation65,Citation66 Others include uveal melanocytoma, adenomatous hyperplasia, medulloepithelioma, leiomyoma, lymphoma, schwannoma and glioneuroma.Citation67–69 Malignant tumours include adenocarcinoma and melanomas.Citation70 The UBM is helpful in differentiating a few of these masses and in monitoring them over a period of time. ANPCE usually has medium echogenicity, while APCE, melanocytoma has high echogenicity with a characteristic posterior shadowing.Citation47 Melanomas however have low to medium echogenicity with metastatic lesions having a variable echogenicity.Citation71 Benign lesions have a regular internal structure, melanoma usually has acoustic hollowness with possible lacunae in between and metastatic lesions have irregular internal structure.Citation71 Based on UBM findings, authors have recently been able to coin the term “ring lymphoma of the ciliary body”, due to the tendency of the ciliary body lymphoma to grow 360 degrees circumferentially. With this in mind, ring melanomas have also been described, wherein there is an involvement of six or more clock hours, not necessarily a 360 degree involvement.Citation72 Differentiating the two on UBM is as described above, with regards to echogenicity and internal structure. The few challenges though, are that it is quite a problematic task to acquire images in the same quadrant, zone and in the exact same orientation during follow up.
DRAWBACKS
We are still not able to ascertain pupil size by UBM and this is still a major setback in analysis and comparison of parameters. Localization of the scleral spur on UBM is another major factor for creeping of errors in measurements. Refining this would lead to more proper and accurate findings. Poorer resolution of the UBM images as compared to OCT images may be a source of error while determining parameters. While acquiring scans, the possibility of a few misoriented scans is always there, and this will remain a source of error. Any measurement involving the ciliary processes has an intrinsic fallacy, because each process will vary in size and orientation at that particular point in time, which brings to the fore another ingrained error in imaging of the ciliary body. Dynamic changes will always occur in the ciliary body and iris during accommodation or with changes in illumination. Ethnicity remains a big confounder, wherein, environmental influences seem to play no role. This was shown by He et al., where American Chinese and Mainland Chinese subjects had comparable UBM parameters. The Chinese were found to have thinner CBT1 as compared to Caucasians and it had a negative correlation with age, possibly due to muscle atrophy with increasing age. An important hypothesis made by the authors was that a thinner ciliary body would not be securely attached to the scleral spur, therefore leading to anterior positioning of the ciliary processes,Citation24 with a thicker and anteriorly positioned lens adding to the issue, more so in Chinese females. This could help to explain the increased incidence of non-pupillary block glaucoma in Chinese females.Citation24 Other confounding factors would be age, physical stature and background illumination during examination.
FUTURE PROSPECTS
UBM is preferred over the OCT because of its ability to image structures behind the thick pigmented irisCitation9 but a lot of lacunae of knowledge still exists in this field and standardization of measurements has to be performed. Consensus has to be reached on defining all the parameters universally, to facilitate standardized measurements. Future studies will hopefully be able to shed some light on the role of the ciliary body in all of the ocular disorders mentioned in this review and many more other disorders.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Duke-Elder S, Wyber KC. The Anatomy of the Visual System, Duke-Elder S ed. London: Henry Kimpton; 1961.
- Pavlin C J, Harasiewicz K, Sherar M D and Foster F Stuart. (1991). Clinical Use of Ultrasound Biomicroscopy. Ophthalmology, 98(3), 287–295. 10.1016/S0161-6420(91)32298-X
- Garudadri CS, Chelerkar V, Nutheti R. An ultrasound biomicroscopic study of the anterior segment in Indian eyes with primary angle-closure glaucoma. J Glaucoma. 2002 Dec;11(6):502–507. doi:10.1097/00061198-200212000-00009.
- Gohdo T, Tsumura T, Iijima H, Kashiwagi K, Tsukahara S. Ultrasound biomicroscopic study of ciliary body thickness in eyes with narrow angles. Am J Ophthalmol. 2000 Mar;129(3):342–346. doi:10.1016/S0002-9394(99)00353-0.
- Kumar RS, Tantisevi V, Wong MH, et al. Plateau iris in Asian subjects with primary angle closure glaucoma. Arch Ophthalmol. Oct 2009;127(10):1269–1272. doi:10.1001/archophthalmol.2009.241.
- Wang Z, Huang J, Lin J, Liang X, Cai X, Ge J. Quantitative measurements of the ciliary body in eyes with malignant glaucoma after trabeculectomy using ultrasound biomicroscopy. Ophthalmology. 2014 Apr;121(4):862–869. doi:10.1016/j.ophtha.2013.10.035.
- Lincke J-B, Keller S, Amaral J, Zinkernagel MS, Schuerch K. Ciliary body length revisited by anterior segment optical coherence tomography: implications for safe access to the pars plana for intravitreal injections. Graefes Arch Clin Exp Ophthalmol. 2021 Jun;259(6):1435–1441. doi:10.1007/s00417-020-04967-3.
- Okamoto Y, Okamoto F, Nakano S, Oshika T. Morphometric assessment of normal human ciliary body using ultrasound biomicroscopy. Graefes Arch Clin Exp Ophthalmol. 2017 Dec;255(12):2437–2442. doi:10.1007/s00417-017-3809-4.
- Garcia JPS, Spielberg L, Finger PT. High-frequency ultrasound measurements of the normal ciliary body and iris. Ophthalmic Surg Lasers Imaging. 2011 Aug;42(4):321–327. doi:10.3928/15428877-20110603-03.
- Kim C, Yu HG. Changes in ciliary body thickness in patients with diabetic macular edema after vitrectomy. Retina. 2012 Jul;32(7):1316–1323. doi:10.1097/IAE.0b013e318236e81d.
- Marianelli BF, Mendes TS, de Almeida Manzano RP, Garcia PN, Teixeira IC. Observational study of intraocular lens tilt in sutureless intrascleral fixation versus standard transscleral suture fixation determined by ultrasound biomicroscopy. Int J Retina Vitreous. 2019;5(1):33. doi:10.1186/s40942-019-0182-y.
- Chen Q, Tan W, Lei X, et al. Clinical prediction of excessive vault after implantable collamer lens implantation using ciliary body morphology. J Refract Surg. Jun 1 2020;36(6):380–387. doi:10.3928/1081597X-20200513-02.
- Sheppard AL, Davies LN. In vivo analysis of ciliary muscle morphologic changes with accommodation and axial ametropia. Invest Ophthalmol Vis Sci. 2010 Dec;51(12):6882–6889. doi:10.1167/iovs.10-5787.
- Muftuoglu O, Hosal BM, Zilelioglu G. Ciliary body thickness in unilateral high axial myopia. Eye (Lond). 2009 May;23(5):1176–1181. doi:10.1038/eye.2008.178.
- Prata TS, Dorairaj S, De Moraes CGV, et al. Is preoperative ciliary body and iris anatomical configuration a predictor of malignant glaucoma development? Clin Exp Ophthalmol. Aug 2013;41(6):541–545. doi:10.1111/ceo.12057.
- Gupta V, Jha R, Srinivasan G, Dada T, Sihota R. Ultrasound biomicroscopic characteristics of the anterior segment in primary congenital glaucoma. J AAPOS. 2007 Dec;11(6):546–550. doi:10.1016/j.jaapos.2007.06.014.
- Ku JY, Nongpiur ME, Park J, et al. Qualitative evaluation of the iris and ciliary body by ultrasound biomicroscopy in subjects with angle closure. J Glaucoma. Dec 2014;23(9):583–588. doi:10.1097/IJG.0b013e318285fede.
- Mishima HK, Shoge K, Takamatsu M, Kiuchi Y, Tanaka J. Ultrasound biomicroscopic study of ciliary body thickness after topical application of pharmacologic agents. Am J Ophthalmol. 1996 Mar;121(3):319–321. doi:10.1016/S0002-9394(14)70282-X.
- Marchini G, Toscano A, Tosi R, Marraffa M, Bonomi L. Ultrasound biomicroscopy study of ciliary body and its influence on anterior chamber angle width. Acta Ophthalmol Scand Suppl. 1997;(224):27–28.
- Sakata LM, Sakata K, Susanna R, et al. Long ciliary processes with no ciliary sulcus and appositional angle closure assessed by ultrasound biomicroscopy. J Glaucoma. Oct 2006;15(5):371–379. doi:10.1097/01.ijg.0000212251.72207.19.
- Liu W, Qin L, Xu C, et al. Transscleral cyclophotocoagulation followed by cataract surgery: a novel protocol to treat refractory acute primary angle closure. BMC Ophthalmol. May 29 2020;20(1):209. doi:10.1186/s12886-020-01483-0.
- Jiang Y, He M, Huang W, Huang Q, Zhang J, Foster PJ. Qualitative assessment of ultrasound biomicroscopic images using standard photographs: the liwan eye study. Invest Ophthalmol Vis Sci. 2010 Apr;51(4):2035–2042. doi:10.1167/iovs.09-4145.
- Mohamed Farouk M, Naito T, Shinomiya K, Mitamura Y. Observation of ciliary body changes during accommodation using anterior OCT. J Med Invest. 2018;65(1.2):60–63. doi:10.2152/jmi.65.60.
- He N, Wu L, Qi M, et al. Comparison of ciliary body anatomy between American caucasians and ethnic Chinese using ultrasound biomicroscopy. Curr Eye Res. 2016;41(4):485–491. doi:10.3109/02713683.2015.1024869.
- Oliveira C, Tello C, Liebmann JM, Ritch R. Ciliary body thickness increases with increasing axial myopia. Am J Ophthalmol. 2005 Aug;140(2):324–325. doi:10.1016/j.ajo.2005.01.047.
- Safwat AMM, Hammouda LM, El-Zembely HI, Omar IAN. Evaluation of ciliary body by ultrasound bio-microscopy after trans-scleral diode cyclo-photocoagulation in refractory glaucoma. Eur J Ophthalmol. 2020 Nov;30(6):1335–1341. doi:10.1177/1120672119899904.
- Okamoto F, Nakano S, Okamoto C, Hommura S, Oshika T. Ultrasound biomicroscopic findings in aniridia. Am J Ophthalmol. 2004 May;137(5):858–862. doi:10.1016/j.ajo.2003.12.014.
- Adams C. Ergonomic lighting levels by room for residential spaces 1206643 . 2021.
- Ma J, Chen X. Dynamic changes of configuration and position of human ciliary body during accommodation. Zhonghua Yan Ke Za Zhi. Sep 2004;40(9):590–596.
- Bailey MD, Sinnott LT, Mutti DO. Ciliary body thickness and refractive error in children. Invest Ophthalmol Vis Sci. 2008 Oct;49(10):4353–4360. doi:10.1167/iovs.08-2008.
- Croft MA, Glasser A, Kaufman PL. Accommodation and presbyopia. Int Ophthalmol Clin. 2001;41(2):33–46. doi:10.1097/00004397-200104000-00005.
- Charman WN. The eye in focus: accommodation and presbyopia. Clin Exp Optom. 2008 May;91(3):207–225. doi:10.1111/j.1444-0938.2008.00256.x.
- Lewis HA, Kao C-Y, Sinnott LT, Bailey MD. Changes in ciliary muscle thickness during accommodation in children. Optom Vis Sci. 2012 May;89(5):727–737. doi:10.1097/OPX.0b013e318253de7e.
- Kano K, Kuwayama Y, Mizoue S, et al. Observation of physiological change in the human ciliary body using an ultrasound biomicroscope during accommodation. Nippon Ganka Gakkai Zasshi. Apr 1999;103(4):297–300.
- Schultz KE, Sinnott LT, Mutti DO, Bailey MD. Accommodative fluctuations, lens tension, and ciliary body thickness in children. Optom Vis Sci. 2009 Jun;86(6):677–684. doi:10.1097/OPX.0b013e3181a7b3ce.
- Glasser A, Croft MA, Brumback L, Kaufman PL. Ultrasound biomicroscopy of the aging rhesus monkey ciliary region. Optom Vis Sci. 2001 Jun;78(6):417–424. doi:10.1097/00006324-200106000-00014.
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006 Mar;90(3):262–267. doi:10.1136/bjo.2005.081224.
- Wang N, Wu H, Fan Z. Primary angle closure glaucoma in Chinese and Western populations. Chin Med J (Engl). Nov 2002;115(11):1706–1715.
- Nonaka A, Kondo T, Kikuchi M, et al. Cataract surgery for residual angle closure after peripheral laser iridotomy. Ophthalmology. Jun 2005;112(6):974–979. doi:10.1016/j.ophtha.2004.12.042.
- Ritch R, Tham CCY, Lam DSC. Long-term success of argon laser peripheral iridoplasty in the management of plateau iris syndrome. Ophthalmology. 2004 Jan;111(1):104–108. doi:10.1016/j.ophtha.2003.05.001.
- Wand M, Grant WM, Simmons RJ, Hutchinson BT. Plateau iris syndrome. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. Feb 1977;83(1):122–130.
- Mansoori T, Sarvepally VK, Balakrishna N. Plateau iris in primary angle closure glaucoma: an ultrasound biomicroscopy study. J Glaucoma. 2016 Feb;25(2):e82–86. doi:10.1097/IJG.0000000000000263.
- Mandell MA, Pavlin CJ, Weisbrod DJ, Simpson ER. Anterior chamber depth in plateau iris syndrome and pupillary block as measured by ultrasound biomicroscopy. Am J Ophthalmol. 2003 Nov;136(5):900–903. doi:10.1016/S0002-9394(03)00578-6.
- Congdon NG, Youlin Q, Quigley H, et al. Biometry and primary angle-closure glaucoma among Chinese, white, and black populations. Ophthalmology. Sep 1997;104(9):1489–1495. doi:10.1016/S0161-6420(97)30112-2.
- Verma S, Nongpiur ME, Oo HH, et al. Plateau iris distribution across anterior segment optical coherence tomography defined subgroups of subjects with primary angle closure glaucoma. Invest Ophthalmol Vis Sci. Oct 1 2017;58(12):5093–5097. doi:10.1167/iovs.17-22364.
- Kumar RS, Baskaran M, Chew PTK, et al. Prevalence of plateau iris in primary angle closure suspects an ultrasound biomicroscopy study. Ophthalmology. Mar 2008;115(3):430–434. doi:10.1016/j.ophtha.2007.07.026.
- Pavlin CJ, Harasiewicz K, Sherar MD, Foster FS. Clinical use of ultrasound biomicroscopy. Ophthalmology. 1991 Mar;98(3):287–295. doi:10.1016/S0161-6420(91)32298-X.
- Romito N, Bluwol E, Graber M, Le Pape C, Lachkar Y. Argon laser iridoplasty for plateau iris syndrome: long-term outcomes of 48 eyes. J Glaucoma. 2019 Sep;28(9):767–771. doi:10.1097/IJG.0000000000001313.
- Pavlin CJ, Foster FS. Plateau iris syndrome: changes in angle opening associated with dark, light, and pilocarpine administration. Am J Ophthalmol. 1999 Sep;128(3):288–291. doi:10.1016/S0002-9394(99)00149-X.
- Feraru C, Bâlha A, Aursulesei V, Filip A, Pantalon A. Plateau iris - therapeutic options and functional results after treatment. Rom J Ophthalmol. 2017 Jun;61(2):117–122. doi:10.22336/rjo.2017.22.
- Schroeder W, Fischer K, Erdmann I, Guthoff R. Ultrasound biomicroscopy and therapy of malignant glaucoma. Klin Monbl Augenheilkd. 1999 Jul;215(1):19–27. doi:10.1055/s-2008-1034664.
- Ueda J, Sawaguchi S, Kanazawa S, et al. Plateau iris configuration as a risk factor for malignant glaucoma. Nippon Ganka Gakkai Zasshi. Sep 1997;101(9):723–729.
- Wang M, Tan Q, Jiang H, et al. Clinical analysis of malignant glaucoma after glaucoma surgery. Zhong Nan Da Xue Xue Bao Yi Xue Ban. May 2015;40(5):543–548. doi:10.11817/j.1672-7347.2015.05.015.
- Grant WM, Walton DS. Progressive changes in the angle in congenital aniridia, with development of glaucoma. Trans Am Ophthalmol Soc. 1974;72:207–228.
- Margo CE. Congenital aniridia: a histopathologic study of the anterior segment in children. J Pediatr Ophthalmol Strabismus. 1983 Oct;20(5):192–198. doi:10.3928/0191-3913-19830901-06.
- Wang N, Ouyang J. The real-time observation of anterior segment of primary congenital glaucoma. Yan Ke Xue Bao. Jun 1998;14(2):83–86.
- Gilbert RE, Vranes D, Berka JL, et al. Vascular endothelial growth factor and its receptors in control and diabetic rat eyes. Lab Invest. Aug 1998;78(8):1017–1027.
- Peizeng Y, Qianli M, Xiangkun H, Hongyan Z, Li W, Kijlstra A. Longitudinal study of anterior segment inflammation by ultrasound biomicroscopy in patients with acute anterior uveitis. Acta Ophthalmol. 2009 Mar;87(2):211–215. doi:10.1111/j.1755-3768.2008.01194.x.
- Kojima T, Yokoyama S, Ito M, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. Apr 2012;153(4):632–7, 637.e1. doi:10.1016/j.ajo.2011.06.031.
- Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol. 2016;10:1059–1077. doi:10.2147/OPTH.S111620.
- Lee D-H, Choi S-H, Chung E-S, Chung T-Y. Correlation between preoperative biometry and posterior chamber phakic visian implantable collamer lens vaulting. Ophthalmology. 2012 Feb;119(2):272–277. doi:10.1016/j.ophtha.2011.07.047.
- Ishigooka H, Yamabe H, Kobashi Y, Nagata M. Clinical and pathological status of mesectodermal leiomyoma of the ciliary body. A case report and review of the literature. Graefes Arch Clin Exp Ophthalmol. 1989;227(2):101–105. doi:10.1007/BF02169778.
- Taban M, Sears JE, Singh AD. Ciliary body naevus. Eye (Lond). 2007 Dec;21(12):1528–1530. doi:10.1038/sj.eye.6702622.
- Goto H, Yamakawa N, Tsubota K, Umazume K, Usui Y. Clinicopathologic analysis of 32 ciliary body tumors. Jpn J Ophthalmol. 2021 Mar;65(2):237–249. doi:10.1007/s10384-021-00814-y.
- Pita-Ortiz IY, Padilla-García E, Ramirez-Estudillo A, Graue-Moreno G. Not every pigmented tumour is melanoma: adenoma of the ciliary body pigment epithelium. Arch Soc Esp Oftalmol (Engl Ed). 2020 Sep;95(9):463–466. doi:10.1016/j.oftal.2020.03.009.
- Chen Z, Fang X. Adenoma of nonpigmented epithelium in ciliary body: literature review and case report. J Zhejiang Univ Sci B. 2007 Sep;8(9):612–615. doi:10.1631/jzus.2007.B0612.
- Alkatan HM, Al-Dahmash SA, Aljaedi H. A case of ciliary body mesectodermal leiomyoma with rapid growth and loss of vision necessitating enucleation. Ann Med Surg (Lond). Dec 2020;60:651–653. doi:10.1016/j.amsu.2020.11.067.
- Esmaili DD, Mukai S, Jakobiec FA, Kim IK, Gragoudas ES. Ocular melanocytoma. Int Ophthalmol Clin. 2009;49(1):165–175. doi:10.1097/IIO.0b013e31819248d7.
- Kaliki S, Shields CL, Eagle RC, et al. Ciliary body medulloepithelioma: analysis of 41 cases. Ophthalmology. Dec 2013;120(12):2552–2559. doi:10.1016/j.ophtha.2013.05.015.
- Lee T, Semenova E, Proia AD, Materin MA. A case of high-risk ciliary body melanoma arising in an eye following resection of an iridociliary melanocytoma. Retin Cases Brief Rep. Jun 24, 2021;Publish Ahead of Print. doi:10.1097/ICB.0000000000001178.
- Méndez-Martínez S, Santiago Varela M, Blanco-Teijeiro MJ, Piñeiro-Ces A. Diagnosis and long-term monitoring of adenomas of the ciliary body epithelium by ultrasound biomicroscopy. Eur J Ophthalmol. 2021 Jul;31(4):2032–2041. doi:10.1177/1120672120952645.
- Demirci H, Shields CL, Shields JA, Honavar SG, Eagle RC. Ring melanoma of the ciliary body: report on twenty-three patients. Retina. 2002;Dec 22(6):698–706. quiz 852–3 doi:10.1097/00006982-200212000-00003.