ABSTRACT
Purpose
To systematically review surgical procedure, safety and efficacy of Gonioscopy-Assisted Transluminal Trabeculotomy (GATT).
Methods
A review of literature was done to analyze all suitable articles from two different databases.
Results
GATT is effective in reducing intraocular pressure and mean number of medications from baseline. It is associated with minimal complications when compared to ab-externo procedures. It has shorter learning curve and can be performed as primary surgical procedure in moderate-to-severe case of open-angle glaucomas.
Conclusion
GATT is a minimally invasive surgical procedure for the management of primary and secondary open-angle glaucoma in both adults and children. The advantages of GATT are ab-interno approach, access to open entire natural drainage system, good safety profile and efficacy comparable to trabeculectomy. It can be performed with both illuminated micro-catheter and suture, out of which suture GATT is cost-effective, which is a boon to developing nations.
INTRODUCTION
About 111 million individuals by 2040 are expected to become irreversibly blind due to chronic optic neuropathy caused by glaucoma.Citation1 The final goal of all various glaucoma treatment strategies is to prevent disease progression by lowering intraocular pressure, which is the only modifiable risk factor.Citation2 Trabeculectomy, though gold-standard procedure, has its own complications such as hypotony, wound leak, induced astigmatism, bleb-related infections and choroidal detachment.Citation3 Contrary to the conventional filtration surgeries, angle-based procedure, like goniotomy, is a blebless surgical procedure to decrease the intraocular pressure by increasing the aqueous humour outflow through Schlemm’s canal and collector channels. Angle-based surgery which is associated with less complications can be done for open-angle glaucoma (OAG) as primary procedure. Limited opening of Schlemm’s canal by conventional ab-externo trabeculotomy with metal trabeculotome is less effective in reducing IOP. 360-degree trabeculotomy can be achieved by either suture or illuminated micro-catheter-assisted ab-externo circumferential trabeculotomy (AECT). Although AECT was more effective than metal trabeculotomy in reducing IOP,Citation4 it still needed conjunctival incision and scleral flap to identify and enter the Schlemm’s canal. Therefore, if need for further filtration surgery in future arises, it is not possible because of scarring of conjunctiva.Citation5
A new ab-interno, sutureless trabeculotomy referred to as gonioscopy-assisted transluminal trabeculotomy (GATT) was first developed by Grover and colleagues at the Glaucoma Associates of Texas in 2014 to conquer the demerits of AECT.Citation6 Direct visualization and good view of Schlemm’s canal to insert suture or micro-catheter under direct gonioscopy is needed to perform all steps of GATT within anterior chamber. It is important to note that the approach is via clear corneal wounds only without involving conjunctiva and sclera, therefore making it a conjunctival-sparing procedure with minimal tissue handling with promising results in clinical practice. The use of suture to achieve 360-degree trabeculotomy makes it a cost-effective treatment modality for situations with poor resources.Citation4,Citation5
This review article will comprehensively summarize the indications, procedure, postoperative management, follow-up, efficacy of GATT and its current relevance in developing nations.
METHOD OF LITERATURE RESEARCH
Articles were reviewed from two databases, PubMed and Libgen, using keywords GATT, gonioscopy assisted transluminal trabeculotomy and open angle glaucoma. Forty-two abstracts were reviewed and finally sixteen articles were included.
INDICATIONS
GATT like any other angle-based glaucoma surgery needs good visualization of the angle structures. Being a circumferential procedure, it is indicated in OAG.
Primary open-angle glaucoma (POAG)
Secondary open-angle glaucoma (SOAG)
Pseudoexfoliative glaucoma
Pigmentary glaucoma
Uveitic glaucoma
Steroid-induced glaucoma
Post-VR surgery glaucoma
(3) Juvenile open-angle glaucoma
(4) Primary congenital glaucoma
GATT procedure can also be tried in angle-closure glaucoma patients where the appositional angle closure has been relieved after a peripheral iridotomy.
SURGICAL TECHNIQUE
Surgical technique was first described by Davinder S. Grover and his colleagues at Glaucoma Associates of Texas in 2014. The surgical procedure is same for both micro-catheter-based GATT or suture-based GATT using prolene suture.
The head of a patient is turned away from the surgeon and eyepiece of microscope is tilted toward the surgeon by approximately 30–45 degrees so that nasal angle is clearly visible and approachable. The nasal angle is visualized with Swan Jacob gonioprism (). A 23-gauge needle or micro-vitrectomy (MVR) blade paracentesis should be placed nasally either superiorly or inferiorly with tangential orientation (). A tangential entry helps to access the nasal angle more easily as compared to a horizontal stab entry. This initially created paracentesis is used for introduction of suture or micro-catheter into the anterior chamber. Anterior chamber is filled with high-density viscoelastic (sodium hyaluronate) through this site. A 2.2-mm keratome is used to create temporal clear corneal incision (). Avoid limbal vessels while making incisions as the bleeding may encroach the surgical field and can hamper the visualization. In nasal angle, 2-mm goniotomy is made with microsurgical blade through the temporal incision (). Through the initial nasal paracentesis made by MVR blade, a micro-catheter or 5-0 prolene suture is inserted into anterior chamber with the tip placed in the nasal angle (). The tip of suture or micro-catheter in nasal angle is grasped with Microsurgical forceps (23 gauge Grieshaber forceps) which is inserted into anterior chamber from temporal clear corneal incision. The distal end of suture or micro-catheter enters Schlemm’s canal through goniotomy which was made in nasal angle (). The Grieshaber forceps is used to advance the catheter or suture through 360 degrees of Schlemm’s canal (). The path of progression of the micro-catheter through Schelmm’s canal is indicated by illuminated tip. After passing 360 degrees around the Schlemm’s canal, the distal tip of catheter or suture is seen coming out of initial goniotomy incision. It is externalized from the temporal incision to achieve 180-degree trabeculotomy (). Thereafter, the proximal tip of the catheter or prolene suture is pulled into anterior chamber, thus completing a 360-degree trabeculotomy (). Hyphema due to reflux of blood from Schlemm’s canal and viscoelastic is cleared from anterior chamber. One fourth of anterior chamber is filled with viscoelastic to reduce bleeding from the canal at the end of the procedure. Watertight closure of wounds should be done before patching the eye.
Figure 2. Inferonasal or superonasal paracentesis with MVR blade which is used for the introduction of 5-0 prolene suture (note the tangential entry of the MVR blade angulated towards the nasal angle).
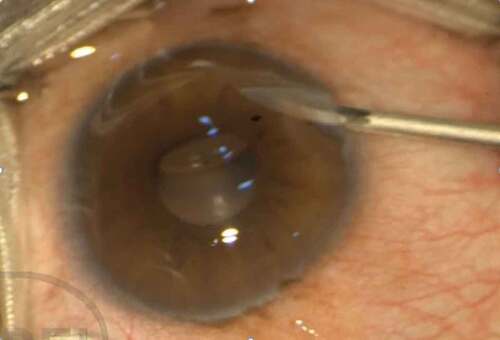
Figure 3. Temporal clear corneal incision with keratome which is used for making goniotomy and for advancement of suture with forceps.
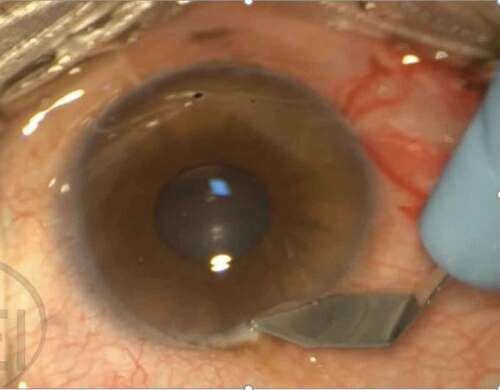
Figure 4. Goniotomy incision is made using MVR blade in the nasal angle (shown using black arrow in the picture). Note the prolene suture on the right side of the image that has already been introduced into the anterior chamber.

Figure 5. Suture is grasped using micro-retinal forceps and introduced into Schlemm’s canal and advancing it 360 degrees.

Figure 6. Proximal end of the suture that has traversed 360 degrees of the Schlemm’s canal is retrieved and exteriorized.

In some cases, when the suture or micro-catheter stops 180–270 degrees and cannot be passed circumferentially in one direction, a limited trabeculotomy can be created. A additional 23-gauge needle incision is created and procedure is repeated in the opposite direction to complete 360 trabeculotomy.
For the cases in which cataract surgery has to be performed along with this procedure, GATT can be performed first, followed by cataract surgery or vice versa. Phacoemulsification can be done with extension of the initiallycreated temporal paracentesis. Epstein et al. reported that angle surgery can be done before or after cataract extraction and the surgical order is usually at the surgeon’s discretion.Citation7
The navigation of micro-catheter tip circumferentially through Schlemm’s canal can be visualized as it is illuminated, therefore offers an additional advantage over suture GATT. Any deviation into sulcus or suprachoroidal space can be immediately identified as catheter is visualized by surgeon throughout procedure. Furthermore, a cutting down the canal or pressure application at different sites of Schlemm’s canal is done by surgeon if catheter halts halfway through Schlemm’s canal or if it enters a collector channel.Citation8
Technique of thermal modification of suture was developed by Grover et al. in 2016. To pass entire circumference of Schlemm’s canal, 4-0 nylon suture clear monofilament or 6-0 polypropylene suture is trimmed to appropriate length. Suture tip is blunted into rounded end with a heating source. Low-temperature cautery with an ophthalmic fine tip can be alternatively used. Within the anterior chamber, modified 5-0 prolene suture is passed through Schlemm’s canal in anti-clockwise direction with the help of Grieshaber forceps. The pathway of progression of the suture can be appreciated with help of Swan Jacob gonioprism. Rest of the procedure is similar as with illuminated micro-catheter.Citation7 It can be performed in primary angle-closure glaucoma too if angle is sufficiently visualized and there is no synechial closure of angle.Citation9
The site of sclerostomy should be evaluated by gonioscopy prior to performing GATT on eye with a prior trabeculectomy. The catheter or suture freely passes all around Schlemm’s canal without any hindrance if the sclerostomy is located in front of canal. Anterior chamber entry or stoppage of suture or catheter occurs if canal is involved by sclerostomy. Then entire 360 circumference of Schlemm’s canal can be accessed by cutting down canal to recover the suture or micro-catheter.
Tube entry site relative to location of Schlemm’s canal should be evaluated by gonioscopy prior to performing GATT in eyes with a prior glaucoma drainage implant. No further additional measures are to be taken if canal was not involved by tube. Suture or micro-catheter stops at tube insertion site if tube involves the canal. In this situation, distal end of suture or micro-catheter can be recovered by cutting down the canal and it is passed in the clockwise direction to access entire circumference of Schlemm’s canal.Citation10,Citation11
EPISCLERAL VENOUS FLUID WAVE
Episcleral venous fluid wave (EFW) is defined as fluid surge of balanced salt solution into the conjunctival and episcleral venous system after 360 cleavage of trabecular meshwork. The anatomical patency of trabecular outflow into episcleral and conjunctival collector channels is indicated by this surge of fluid intraoperatively. Structural patency confirmed by fluid wave need not indicate physiological functioning of trabecular outflow.Citation12
POSTOPERATIVE CARE AND FOLLOW-UP
After surgery, the usual postoperative regimen consists of topical antibiotics and topical steroids. However, the duration and strength of topical steroid use is usually at the surgeon’s discretion. Topical steroids are gradually tapered to control inflammation and to prevent steroid response.Citation6 Pilocarpine 2% is used in the early postoperative period to prevent formation of peripheral anterior synechiae. Postoperative head end elevation position is advised to reduce postoperative hyphema.
COMPLICATIONS
Hyphema is the most common complication seen in almost all cases. The next most common complications of GATT are hypotony and rise of IOP transiently. Vision-threatening complications such as Cystoid macular edema, Choroidal folds, Vitreous hemorrhage, Peripheral anterior synechiae and Descemet’s membrane detachmentCitation5 are less commonly seen.
The hyphema usually occurs due to reflux of blood into anterior chamber due to reversal of pressure gradient between the anterior chamber and the Schlemm channel. Hyphema indicates complete trabecular meshwork removal. Success of procedure is confirmed by this complication.Citation13
Management of Hyphema - Hyphema usually resolves with medical management with topical steroids and cycloplegics over 1–2 weeks.
Other rare complications reported are transient myopia secondary to supraciliary effusion causing visual impairmentCitation14 and pan-scleritis in patients with uveitic glaucoma.Citation15
CONTRAINDICATIONS
Absolute contraindications include bleeding diathesis, inability to stop anticoagulants, subluxated IOL, difficulty in identifying the trabecular meshwork in iridogoniodysgenesis or developmental anomaly, synechial angle closure or severe endothelial decompensation. Procedure is relatively contraindicated in patients with previous corneal transplantation and who are unable to maintain propped-up position for the initial few weeks after procedure .Citation6
ADVANTAGES
Being a conjunctiva-sparing procedure is the biggest advantage of angle-based surgeries. GATT procedure also shares the same advantage.
Advantage over other angle-based surgeries such as trabectome and goniotomy by Kahook Dual Blade (KDB) is that they can treat only 90–110 degrees of angle but GATT can be used 360 or whole circumference of angle.
Suture GATT using prolene suture is highly cost-effective as against catheter-based GATT procedure.
EFFICACY
Guo et al. reported a significant decrease in IOP and mean number of antiglaucoma medications from the baseline after GATT when compared to before the surgery. In this review article, 85% achieved success surgically and 20% underwent reoperation. Rarely, vision-threatening adverse events are observed, whereas 36% has hyphema.Citation4
Wang et al. showed that the mean decrease in IOP in patient with JOAG who underwent GATT was 37.2% at end of 1 year and 47.9% at end of 18 months. The mean reduction in number of antiglaucoma medication (AGM) was 3 at end of 1 year and 3.3 at end of 18 months.Citation11
Grover et al. reported that the mean decrease in IOP from baseline was 30% at end of 6 months and 39.8 at end of 1 year.Citation6 Kamran Rahmatnejad et al. showed that the GATT success rate was 63%.Citation5
Quan et al. reported that mean IOP improved from 32.7 ± 5.1 mm Hg to 13.6 ± 1.8 mm Hg with a reduction (4.8 ± 0.9 to 1.6 ± 1.4) medications after a mean follow-up duration of 8.6 months when GATT was performed in patients with secondary OAG following VR surgery.Citation16
All these studies show good results in short term, but long-term results are to be seen further with regard to trabecular meshwork scarring.
OUR EXPERIENCE
Though in initial stages and with a short follow-up of 6 months, our experience with GATT procedure has been overwhelming. We have performed GATT procedure in 30 eyes with OAG, both primary and secondary. The IOP reduction seen is ~30% from pre-operative values and has been in accordance with the published literature. The need for anti-glaucoma medications (AGM) has been greatly reduced from an average preoperative three medications to one (AGM) in the postoperative follow-up. The most common complication experienced has been transient hyphema which could be medically managed. The short-term results appear promising and GATT procedure definitely has a role as an IOP-reducing procedure in OAG, though long-term follow up in our population needs to be evaluated.
CONCLUSION
GATT is a newer surgical procedure in the management of primary and secondary OAG which is minimally invasive and is suitable for both adults and children. GATT decreases IOP by increasing the aqueous outflow through Schlemm’s canal and collector channels. The advantages of GATT are ab-interno approach, access to open entire natural drainage system, good safety profile and efficacy comparable to trabeculectomy. It can be performed with both illuminated micro-catheter and suture out of which suture GATT is cost-effective which is a boon to developing nations.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
Additional information
Funding
REFERENCES
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013.
- Salimi A, Nithianandan H, Al Farsi H, Harasymowycz P, Saheb H. Gonioscopy-assisted transluminal trabeculotomy in younger to middle-aged adults: one-year outcomes. Ophthalmology Glaucoma. 2021;4(2):162–172. doi:10.1016/j.ogla.2020.08.014.
- Faria BM, Daga FB, Rebouças-Santos V, Araujo, R B, Matos Neto, C, Jacobina, J S, and Faria , M A, et al. Gonioscopy-assisted transluminal trabeculotomy (GATT) outcomes in eyes with open-angle glaucoma resistant to maximum treatment. ArquivosBrasileiros de Oftalmologia 84 6 587–93 doi:10.5935/0004-2749.20210083 . 2021. 34320113
- Guo CY, Qi XH, Qi JM. Systematic review and meta-analysis of treating open angle glaucoma with gonioscopy-assisted transluminal trabeculotomy. Int J Ophthalmol. 2020;13(2):317. doi:10.18240/ijo.2020.02.17.
- Rahmatnejad K, Pruzan NL, Amanullah S, et al. Surgical outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in patients with open-angle glaucoma. J Glaucoma. 2017;26(12):1137–1143. doi:10.1097/IJG.0000000000000802.
- Grover DS, Godfrey DG, Smith O, Feuer WJ, De Oca IM, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology. 2014;121(4):855–861. doi:10.1016/j.ophtha.2013.11.001.
- Epstein RS, Scott AT, Capitena Young CE, et al. Optimum time for angle visualization during ab interno glaucoma surgery: before or after phacoemulsification. J Cataract Refract Surg. 2019;45(5):615–619. doi:10.1016/j.jcrs.2019.01.012. PMID: 31030776.
- Grover DS, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy (GATT): thermal suture modification with a dye-stained rounded tip. J Glaucoma. 2016;25(6):501–504. doi:10.1097/IJG.0000000000000325.
- Sharkawi E, Artes P H, Lindegger D Josef, Dari, M Laura, Wardani, M EI, Pasquier, J, and Guarnieri, A, et al. Gonioscopy-assisted transluminal trabeculotomy in primary angle-closure glaucoma. Graefes Arch Clin Exp Ophthalmol 259 10 . 2021;3019–26 doi:10.1007/s00417-021-05244-7. 34155560
- Grover DS, Godfrey DG, Smith O, Shi W, Feuer WJ, Fellman RL. Outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyes with prior incisional glaucoma surgery. J Glaucoma. 2017;26(1):41–45. doi:10.1097/IJG.0000000000000564.
- Wang Y, Wang H, Han Y, et al. Outcomes of gonioscopy-assisted transluminal trabeculotomy in juvenile-onset primary open-angle glaucoma. Eye. 2021;35(10):2848–2854. doi:10.1038/s41433-020-01320-0.
- Fellman RL, Grover DS. Episcleral venous fluid wave: intraoperative evidence for patency of the conventional outflow system. J Glaucoma. 2014;23(6):347–350. doi:10.1097/IJG.0b013e31827a06d8.
- Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma. 2018;27(10):849–855. doi:10.1097/IJG.0000000000001019.
- Aktas Z, Ucgul AY, Segawa A. Transient myopia secondary to supraciliary effusion: unusual complication after an uneventful prolene gonioscopy-assisted transluminal trabeculotomy. J Glaucoma. 2020;29(7):e60–3. doi:10.1097/IJG.0000000000001531.
- Aktas Z, Bektas C, Hasanreisoglu M. Panscleritis as an unusual complication of gonioscopy-assisted transluminal trabeculotomy. J Glaucoma. 2019;28(2):e21–3. doi:10.1097/IJG.0000000000001100.
- Quan AV, Yannuzzi N, Chen J, Wang YE, Townsend J, Chang TC. Gonioscopy-Assisted transluminal trabeculotomy (GATT) in patients with secondary open angle glaucoma following vitreoretinal surgery. J Glaucoma. 2020;29(4):e23. doi:10.1097/IJG.0000000000001461.


