ABSTRACT
Purpose
To provide a comprehensive review on secondary IOL implantation in children who have undergone primary surgery at an early age and are aphakic aiming at answering common dilemmas among pediatric ophthalmologists.
Method of literature review
A systematic literature search was done using keywords like secondary intraocular implantation, congenital cataractand surgical aphakia. Various novel case reports, retrospective case studies and review articles covering different aspects of secondary IOL implantation were searched and reviewed using PubMed and Google scholar journal search engines.
Results
This article highlights various aspects of secondary IOL implantation like the appropriate timing should be when the child is entering preschool, with the proper technique being in bag fixation is the most preferred method with least associated complications and the IOL type should be decided based on the fixation site.
Conclusion
Secondary IOL implantation can accomplish good and stable long-term outcomes in children. It is the most accepted mode of optical correction once the appropriate age is achieved.
INTRODUCTION
Secondary IOL implantation is considered in children who previously were operated for congenital cataract extraction usually after 2 years of age when these children become intolerant to aphakic correction.1 There are numerous modalities of optical corrections available like contact lenses, spectacles, and intraocular lens implantation. Early visual rehabilitation of these children along with appropriate amblyopia management can help to improve their visual acuity and quality of life.Citation2,Citation3 When children and their parents are unwilling to accept glasses or contact lenses for optical correction, secondary IOL implantation can be considered. But for children who are less than 2 years of age, this can be a little challenging as one needs to consider age-appropriate under-correction, refractive outcomes considering constant eyeball growth. The initial hypermetropia after under-correction is thought to be more amblyogenic by some surgeons.Citation4,Citation5
The other dilemma which is faced is concerning the site of IOL implantation. The assessment of capsular support or IOL power calculation in very young children could be difficult in an office setup. The presence or absence of capsular support will determine the IOL fixation site and IOL type or design. In a study by Serafino et al., many unresolved issues concerning secondary IOL implantation were attempted to be addressed.Citation5 The scope of this article is to provide a comprehensive review of all aspects related to secondary IOL implantation in children like appropriate age, timing, indications, contraindications, the most preferred site of IOL fixation along with other sites, preferred IOL formulae calculation, appropriate selection of IOL material/designs and finally common complications of the procedure.
INDICATIONS FOR SECONDARY IOL IMPLANTATION
Optical correction is a critical component of visual rehabilitation in children with aphakia. Primary IOL implantation in children less than two years of age remains controversial. The resultant aphakia from the primary surgery needs optical correction for normal visual development. Aphakia can be corrected using aphakic glasses or contact lenses (CL). Aphakic glasses are preferred in children with bilateral aphakia. CL is another very acceptable option for aphakia correction, especially in presence of unilateral aphakia. Since the early 1950s CL has been used for optical correction in children. High plus power CLs are easily available for aphakic correction these days.Citation6
There are a few pros and cons of each of these methods. Aphakic glasses result in the prismatic distortion of images, visual field constriction, retinal disparity, heavy weight and it is cosmetically, psychologically debilitating for children and their caretakers.Citation7
Aphakic CLs are more socially and cosmetically acceptable, it is a better choice for unilateral aphakia. These provide a better field of vision and there is less image-size disparity. However, there are complications associated with their use like difficult insertion, non-compliance of both parents and patients, corneal complications like keratitis, frequency of lens loss that adds to the costin addition to psychological stress.Citation8−Citation9
The IOL implantation reduces the dependency on external optical devices and provides constant refractive correction. Hence, the common indications of secondary IOL implantation are as follows:
Non-compliance to spectacles or contact lenses
Parental needs and cosmesis
Unilateral cases
Difficult to handle contact lenses
Unable to renew spectacles/ CL due to poor socioeconomic status or its unavailability in remote places
PRE-OPERATIVE EVALUATION
A detailed workup is necessary before deciding on secondary IOL implantation. Visual acuity, slit-lamp biomicroscopy, a thorough examination of the sulcus, the extent of capsular support, presence of synechiae, shape, and size of the pupil, vitreous strand in the anterior chamber, central corneal thickness, keratometry, axial length, intraocular pressure, dilated fundus examination, and gonioscopy must be included in the clinical workup.[] When the sulcus examination becomes difficult clinically, UBM provides information on the positioning of the ciliary sulcus and its surrounding tissue pre-operatively which will help the surgeon to view the anatomy carefully before planning secondary IOL implantation especially suture fixated IOL implantation.Citation12 Post-surgery, the position of IOL and the capsular bag can be assessed accurately by looking at their interface plane on UBM.Citation13
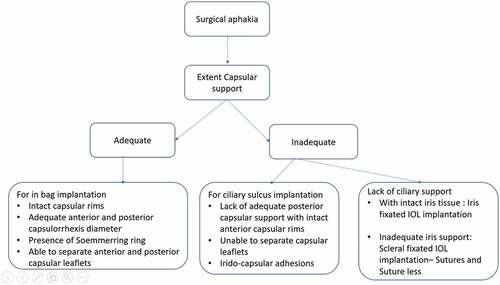
Figure 1. Schematic representation of pre-operative assessment (A-C).
The presence of capsular support and its extent helps us to decide the site of IOL fixation. On routine slit-lamp examination, the patient is asked to look into extreme gazes while keeping the slit lamp stable or one can even look through the peripheral iridectomy to determine the presence of any capsular support. When there are peripheral synechiae there are adhesions between the iris and capsule which indicate the presence of some capsular support. In young children, clinical examination becomes difficult so one can look for a capsule under an operating microscope while examining under anesthesia. Before going ahead with the procedure another dilemma faced by an ophthalmologist is whether to implant the emmetropic powered IOL or under corrected IOL.Citation11Given the myopic shift, many consider under-correction during IOL implantation in children. Another school of thought here is keeping a small under-correction or an initial emmetropia as hypermetropia is considered to be amblyogenic. To compensate for this myopic shift later IOL exchange can be performed in these cases.Citation14
The most popular guidelines for under correction were given by Dahan et al and Enyedi et al.Citation12,Citation13 It was Sachdeva et al. who validated guidelines for under correction.Citation15 The results were consistent with those of Enyedi et al. and it was concluded that children undercorrected using guidelines by Enyedi et al may achieve an acceptable refractive error at 7 years of age.Citation15
Dahan et al proposed under correction based on age, IOL power which is 20% less than the emmetropic IOL power for children <2 years of age and 10% for > 2 years should be considered.Citation12 Whereas, Enyedi et al proposed a rule of seven (7- age in years = amount of under correction).Citation13 In another approach by Chen et al. children between 2–4 years of age are to be undercorrected by 1.25 D less than the fellow eye.Citation16,Citation17
The most preferred method for biometry in older children is with the help of an optical biometer which is IOL Master 500 (Carl Zeiss). Another optical biometer that provides better resolution than the IOL master will be Lenstar LS 900.Citation15,Citation16,Citation18,These methods are contact-free so are preferred over the contact method. For young uncooperative children, it is preferable to perform biometry under general anesthesia using handheld keratometers (Nidek KM, 500) and axial length is calculated by contact A-scan (OcuScan Rxp, Alcon). In presence of disparity between the eyes, it is always better to repeat the readings by another surgeon.Citation18 Pediatric ophthalmologists must measure the parameters of the eyes carefully and predict eye growth as much as possible to implant the IOL which is best suited for each patient at the time of surgery.
APPROPRIATE AGE FOR SECONDARY IOL IMPLANTATION
Deciding the appropriate age for secondary IOL implantation has always been a controversy.Citation1,Citation3,Citation4,Citation10 This question remains unanswered as there are many different views on this.Citation11 In a study by Serafino et al where Delphi process was used to find areas of consensus and also disagreement among pediatric ophthalmologists. Many unanswered queries with regards to secondary IOL implantation were put forward to eminent pediatric ophthalmologists around the world and it was thought that some of the questions which don’t have consensus could be possible areas of research. However, it was concluded that secondary IOL implantation in children can be performed around the age of 4–8 years in patients who can tolerate aphakic glasses or CL well whereas for those who do not tolerate any external mode of optical correction one can consider the procedure at any age even if the child is less than 1 year of age.Citation5
Shenoy et al reviewed visual outcomes of secondary IOL implantation in children and it was seen that the mean age of the surgery and duration between the primary and secondary procedures were less as compared to other published literature. The average age of patients who underwent secondary IOL implantation with good outcome was 6.08±3.75 years.Citation18 The post-operative complications in terms of secondary membrane, rise of intraocular pressure, post-operative inflammation were reported to be less common. The bilateral aphakia patients showed improvement in visual acuity more than unilateral cases. These sulcus fixated IOLs had reasonably good outcomes. In this study the absolute prediction error (PE) was slightly higher as compared to other studies, there was no difference in absolute PE between unilateral and bilateral cases. The absolute PE was better when IOL Master was used as compared to contact biometry.Citation18
It was Trivedi et al who concluded secondary IOL implantations have successful outcomes when performed in children of more than 2 years of age. The two peaks for the procedure noted in this study were between 2–4 years of age and 12–14 years of age. When the presence of capsular support was doubtful scleral tunnel was preferred over corneal incisions. For children less than 6 months of age who underwent cataract surgery the success rate of secondary IOL implantation was explained due to the potential space which was maintained by the proliferating lens equatorial cells between the anterior and posterior capsular leaflets which accounted for more In-the bag IOL implantation. The next common method of fixation used was ciliary sulcus fixation of foldable and PMMA IOLs.Citation3
Secondary IOL implantation is usually advised or performed before the child enters preschool. However, there has been a debate against early placement of IOL like in children less than or of 2 years of age. Prediction error will be high as the eye still grows if the IOL is implanted in this age group. Placing an IOL in young children with age appropriate under correction is always advocated and preferred. There are multiple published literature which have shown different visual and refractive outcomes in different age groups pertaining to secondary IOL implantation []
Table 1. Appropriate age for secondary IOL implantation.
VARIOUS SITES FOR IOL IMPLANTATION
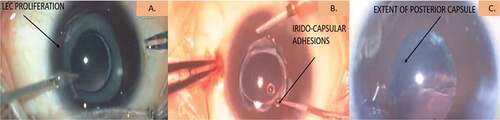
The next important aspect to think about is the appropriate site for IOL fixation which differs case wise.[] Most of the children who have undergone cataract extraction at a very early age have undergone primary posterior capsulotomy with anterior vitrectomy. The most ideal method is in the bag fixation of IOL. However, at times in-bag implantation may not be possible due to lack of standardization of primary surgery. The site of implantation will depend upon presence or absence of adequate capsular support, size of capsulorhexis opening, fusion of anterior and posterior capsular edge, amount of lens epithelial cells proliferation and presence or absence of intact ciliary sulcus.[]
Figure 2. Suitable sites of IOL implantation.
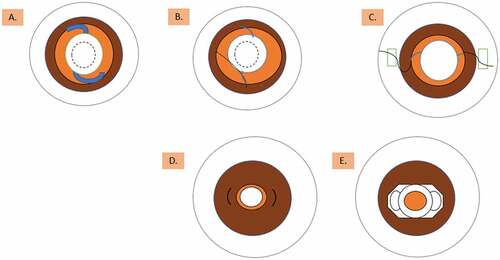
Table 2. Overview of different sites of secondary IOL implantation.
In the Bag Fixation of IOLs
The most ideal and preferred method for all the surgeons is in bag IOL fixation. When cataract surgery is performed during early infancy, even after complete cortical clean up the lens epithelial cells migrate to the equator and proliferate to form a dense Soemmerring ring which occupies a potential space in the bag and prevents capsular fusion.Citation3 It has been seen that this ring is less dense in children who undergo surgery at a later age leading to capsular fusion making in bag IOL placement difficult.
There are studies which showed in bag placements of IOLs were much more successful in children who were operated at a younger age due to maintenance of this potential space.Citation24 According to Serafino et al the ophthalmologists after being a part of the Delphi process concluded that in presence of capsular support an attempt to open the bag and placing the IOL in the bag should always be considered, this was also mentioned by Shenoy et al in his study.Citation5,Citation18
Trivedi et al also concluded the most desirable site of IOL fixation is the reopened capsular bag as the rate of complications associated is extremely low.Citation3 In-bag implantation showed more favorable outcomes than ciliary fixated implantation in a study by Wood et al.Citation22
The process of in bag fixation starts with creating two side ports or paracentesis using astraight microvitreoretinal blade (20 G, Model no. BR 1048, Aurolab, Madurai, India) followed by inflation of the anterior chamber with ophthalmic viscosurgical devices (OVDs). The synechiael adhesion between the iris and capsular rim is removed using an OVD or an iris repositor. In presence of capsular adhesion one can initiate a new capsulorhexis with the help of pediatric microrhexis forceps (23 G, Model no. IG- 3984, Indo-German, Mumbai, India) and vitreoretinal scissors (23 G, Model no. IG-4361, Indo-German, Mumbai, India). The remaining capsular bag is opened up and inflated with OVD, this even helps to clean up the Soemmerring ring along with cortical matter with irrigation and aspiration cannula. The potential space between the previously adhered capsule is created, if needed limited anterior vitrectomy is performed before placing foldable single piece acrylic IOL with the help of an injector carefully in the reopened capsule. The viscoelastic is then washed, wound closure is done with 10–0 nylon sutures (15 centimeters, black monofilament non-absorbable surgical suture, Aurolab, Madurai, India) followed by intracameral antibiotic injection.[]
This has a very low rate of complications; visual axis opacification is usually seen in patients with in bag fixation of IOL along with optic capture.Citation3
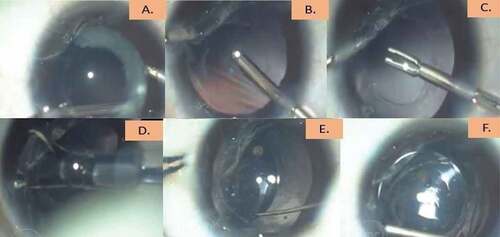
Figure 3. Initial step of opening the capsular bag (A-L).
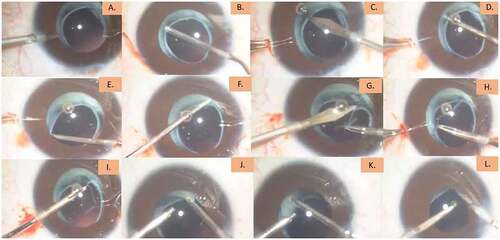
Figure 4. Procedure for in capsular bag fixation of IOL (A-F).
Ciliary Sulcus Fixation of IOLs
Ciliary fixated implantation is relatively a safer option and second most preferred choice. Presence of sulcus can be determined by clinical examination or by performing a UBM and it can be compared with that of a fellow eye.Citation12 Safety profile of this method of fixation was studied by Shenoy et al. It was seen due to lack of standardization of primary surgery the bag implantation was impossible and more than 80% of patients underwent sulcus fixation of IOL with a good visual and refractive outcome with IOL power calculated using SRK II formula.Citation18
Possible complications associated are optic capture, IOL decentrations, pigment dispersion and ciliary body erosion. However, the post-operative complications in terms of secondary membrane, rise of intraocular pressure, post-operative inflammation were reported to be less common by Shenoy et al.Citation18 Trivedi et al also reported less VAO formation with ciliary sulcus IOL implantation but however, it was seen with foldable lenses showed more decentration as compared to PMMA when placed in sulcus if axial length was more than 23 mm especially in male patients.Citation3 The long-term effect of this method was studied by Zhao et al, where it was seen that IOL malposition and crowding of the anterior segment was more and there was higher incidence of secondary glaucoma. However, it was noted that long-term visual outcome was comparable to the capsular fixation of IOLs.Citation24
Here, the initial step will be same as mentioned above, i.e. to create two side ports or paracentesis using straight microvitreoretinal blade (20 G, Model no. BR 1048, Aurolab, Madurai, India) followed by inflation of the anterior chamber with ophthalmic viscosurgical devices (OVDs). This technique is relatively easier. A scleral tunnel incision for placing PMMA (Polymethacrylate) IOL or a clear corneal tunnel incision for placing three-piece acrylic foldable IOLs is created. After injecting OVDs in the anterior chamber using micro- vitreoretinal blade (20 G, Model no. BR 1048, Aurolab, Madurai, India) the capsular bag is attempted to open wherever it is possible, if this fails careful IOL placement in sulcus is achieved with adequate anterior vitrectomy and if Soemmerring ring is present its removal is attempted.[] According to rule of 9 always remember to subtract 1.5 D for 28.5 D, 1 D for 17.5 D-28 D and 0.5 D for 9.5 D-17.0 D when fixation is switched from bag to sulcus implantation. For IOL powers to be less than 9 D no subtraction is required.Citation25
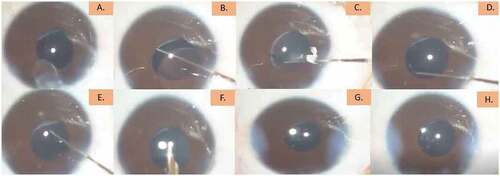
Figure 5. Procedure for ciliary sulcus fixation of IOL (A-H).
Iris Fixated IOL Implantation
Iris claw lenses can be considered as an alternative when capsular support is not adequate for in the bag or ciliary sulcus fixation. Serafino et al stated that iris-claw lenses can be considered as an effective method for secondary IOL implantation in absence of adequate support but never when adequate capsular support is present.Citation5
The aphakic artisan IOL is a peripheral iris bridge supported lens. This has a central oval anterior vault with two fixing haptics to claw the iris tissue. This is known for its excellent stability and is more cosmetically acceptable. However, this also has few disadvantages like acquiring surgical expertise and also a large limbal or scleral incision is to be constructed. Initially, these lenses were developed for anterior chamber enclavation which was associated with unfavorable outcomes in terms of endothelial damage. Siddiqui et al documented endothelial loss of 17% with iris- claw IOL fixation in the anterior chamber in children aged 8 to 15 years during a short follow up period of 12 months.Citation26 In another retrospective study with a follow-up period of up to 15 years, Sminia et al have shown that the endothelial cell count might decrease down to 1400 cells/mm2 in some eye, if the iris-claw IOL is located in the anterior chamber.Citation27,Citation28
These lenses now are used for posterior fixation with good refractive outcome and also less risk of endothelial loss as it maintains good distance from corneal endothelium. Iris-claw IOL is a suitable technique to correct aphakia in children with low complication rates.Citation29 The outcome of retro-pupillary fixation was studied retrospectively by Gonnermann et al who stated no endothelial cell loss was noticed over a period of 3 years with this technique. According to Clearly et al endothelial cell loss with iris claw lenses in aphakic children was similar to that of adult which ranges from 1.5% −10% over three years.Citation30,Citation31
For anterior enclavation, pupil has to constricted prior to IOL implantation. A corneoscleral tunnel is created along with two paracentesis at 3 o’clock and 9 o’clock, OVDs is used to fill the anterior chamber making the iris to lie flat. The Artisan IOL is inserted in a vertical position at the 12 o’clock position and is rotated to the desired position (haptics being at 3 o’clock and 9 o’clock positions) using the Artisan lens manipulator. The first enclavation must be performed with the nondominant hand. The enclavation needle is inserted through one of the paracenteses to stabilize the IOL. The implantation forceps are then inserted through the tunnel to firmly grasp the lens at the optic edge, the other hand is used to create a knuckle of iris tissue using the enclavation needle. A significant fold of iris tissue is then delivered to haptic slot to ensure proper enclavation. After the first enclavation the instruments are transferred to the opposite hand and the fixation steps are repeated. The IOL has to be centered all the time and each iris bridge has to be adequate. Lastly, small peripheral Iridectomy is created followed by OVDs removal and wound closure.Citation29
For retro pupillary fixation, the pupil is not constricted at the beginning of procedure. The IOL is inserted with the convex side down and held behind the pupil with the IOL implantation forceps through the corneoscleral tunnel. As the lens is being placed behind the pupil, pupil is constricted using a miotic agent. A fine spatula is inserted through a paracentesis to exert gentle pressure on the slotted center of the lens haptic for the enclavation. The same maneuver is repeated on the other side.Citation29
The complications commonly seen are IOL decentrations, iritis and also endothelial loss.Citation26–31
Scleral Fixated IOLs
As other alternative scleral fixated IOLs have shown to improve best corrected visual acuities in pediatric aphakia mainly seen post congenital or traumatic cataract extraction and lensectomy. Kumar et al concluded with appropriate amblyopia treatment in patients who underwent scleral fixation for aphakia achieved comparable best corrected visual acuity.Citation32
These IOLs present with different set of perioperative and postoperative complications. The procedure is technically challenging, presents risks of vitreous hemorrhage, chronic uveitis, scleral thinning, cystoid macular edema, endophthalmitis, retinal detachment, glaucoma, IOL tilting and dislocation, exposure and breakage of anchoring suture through the conjunctiva.Citation33 The long-term stability of the procedure as well as complications are yet to be studied.
Glued IOLs
Glued intra-scleral fixation technique has been introduced recently. This involves implanting of PCIOL in cases with deficient posterior capsular support using a fibrin sealant. The haptics of PCIOL are inserted into scleral pockets and the scleral flaps are sealed with a glue. This technique can be used in children with no capsular support post primary cataract extraction, traumatic cataracts and ectopia lentis.Citation33 This technique has a long learning curve and requires a lot of expertise.
The small-incision, sutureless, transconjunctival scleral fixation technique first described by Yamane et al in absence of capsular support by creating small-gauge sclerotomies and a small clear corneal incision. This resulted in faster visual recovery and a low risk of postoperative hypotony. The technique involves externalizing the haptics of the IOL using a double needle technique, and then using cautery to form a mushroom-shaped tip at the end of each haptic. Each haptic is threaded into the lumen of 30-gauge needle introduced through transscleral tunnels made 180 degrees apart. The haptics are threaded using micro-forceps and introduced through the paracentesis adjacent to the plane of the scleral tunnels. As the needles are externalized, the haptics are drawn out through the transscleral tunnel. After cautery, gentle manipulation is used to depress the haptics back into the scleral tunnels and achieve centration of the lens.
Post -operative complications like IOL decentration and suture related were seen to be less with this technique.Citation34 According to Kumar et al, the pediatric patients is their study who underwent this procedure did not show any post-operative strabismus, retinal detachment, IOL dislocation, endophthalmitis or glaucoma but with regular occlusion therapy good visual outcome was achieved.Citation33
Anterior Chamber IOLs
This is not a preferred choice in pediatric aphakia, not many studies have been done to study long-term effect of this technique. The only indication for ACIOL implantation is absence of posterior capsular support and irido-capsular adhesions which makes PCIOL implantation difficult. This technique is associated with series of complications like endothelial loss, iritis, hyphema, secondary glaucoma, cystoid macular edema and at times IOL decentration. According to Turner et al, the children who underwent ACIOL implantation had a higher rate of reoperationswhich was agreed by Epley et al who also demonstrated high rates of complications and very unsatisfactory outcomes. This technique is easier to perform as other techniques have a longer learning curves.Citation19,Citation35
APPROPRIATE IOL DESIGN
Implantation of an adult size IOL in very young children can be problematic. In order to identify the size of pediatric capsular bag and lens, autopsied eyes were examined by Bluestein et al from age 1 day to 16 years and it was found that the most rapid growth of the globe, lens and the capsular bag took place from birth to 2 years of age.Citation36 The IOLs available these days are slightly over sized but can fit into capsular bags of children in first two years of age.[] There can be numerous consequences if a large IOL is placed in a small capsular bag like problematic IOL haptic dialing, zonular stress due to oval stretching of the bag, decentrations, posterior capsular folds with opacification, risk of bag- sulcus asymmetric fixations.Citation37
Table 3. Common IOL designs available.
COMMON COMPLICATIONS
Visual Axis Opacification
VAO or secondary membrane opacification is one of the most common complications seen in cases where posterior capsule is left intact even after placing a hydrophobic intraocular lens. In infants despite performing posterior capsulotomy with anterior vitrectomy and IOL implantation VAO can be one of the common problems. It is seen with younger age group there are more chances of developing VAO. The IOL design like square haptics prevents lens epithelial cell migration and proliferation.Citation38 The average rate of VAO in children older than 2 years is around 5.1% and for children less than two years it is around 8.1% to 80%. This needs secondary intervention as the visual acuity will be affected and chances of developing amblyopia will be high.Citation39–43
Capsular Fibrosis and Posterior Synechia
May lead to shift of the ciliary process to the pupil center, which causes difficulty to secondary IOL implantation in children.
Post-operative Inflammation
Inflammation will be high in the setting of iris claw lenses or anterior chamber IOL implantation and even in presence of irido-capsular adhesions which needs to be released. The in bag IOL implantation shows least post-operative inflammation and corneal edema.43
Transient spike of intraocular pressure or secondary glaucoma
This could be due to retained viscoelastic, inflammation and also in presence of already existing aphakic glaucoma it better to give these children anti-glaucoma medications. Shenoy et al and Vanderveen et al concluded approximately of 4% incidence of glaucoma with sulcus fixated secondary IOLs which was less compared to others.Citation41
Cystoid Macular Edema
CME is seen in setting of significant post-operative inflammation which is likely to develop affecting l visual outcome.
IOL Decentration/ Dislocations
Decentrations have been seen with iris-claw lenses, mono-focal foldable acrylic IOLs when placed in sulcus or are fixed to sclera, in presence of increased white to white diameter and increased axial lengths > 23 mm.Citation3 The three-piece foldable IOL, PMMA lenses show much more promising outcomes when placed in sulcus.
Sight Threatening Complications
Endophthalmitis, retinal detachments, glaucoma and sympathetic ophthalmia in children with significant uveitis are few sight- threatening complications.
VISUAL OUTCOMES
Secondary IOL implantation is a safe and effective method for aphakic correction in children above 2 years of age but in less than 2 years the external optical aphakic correction should be preferred over IOL implantation considering the biometry and also constant refractive status change. However, studies by Koch et al and Shenoy et al have shown successful outcomes in children less than 30 months and less than 2 years respectively who underwent secondary IOL implantation.Citation18,Citation20
The overall safety and visual outcomes in surgically aphakic children undergoing secondary intraocular lens (IOL) implantation were evaluated by Shenoy et al where it was concluded with their retrospective study that secondary sulcus IOL implantation in children is a relatively safe procedure and leads to favorable visual postoperative outcomes. The improvement in BCVA in the bilateral secondary IOL group is significantly higher compared with the unilateral secondary IOL but both the groups showed improvement.Citation18 According to Woods et al the final visual acuity achieved at final follow-up for bilateral secondary IOL group was better than the unilateral group.Citation24 Another study which supports this procedure was by Trivedi et al who stated that foldable IOLs in bag is the most favored procedure with good stability.Citation3
CONCLUSION
Placing an IOL is the most acceptable and preferred method of aphakia correction when other traditional practices become unsuccessful. This is extremely important in treating amblyopia and encouraging normal visual development. Due to constant growth of eyeball in children and their unstable refractive status giving spectacle free lives to children is a bit challenging. To summarize, secondary IOL implantation can be performed in children of more than 2 years of age, in presence of adequate capsular support keeping age appropriate under correction in mind in bag fixation of IOL gives the best result followed by ciliary sulcus fixated IOLs. There are other sites where an IOL can be implanted based on the capsular support.[]
Supplemental Material
Download MS Word (12.6 KB)Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplementary Material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/08820538.2022.2116288
Additional information
Funding
References
- Wilson Jr ME, Englert JA, Greenwald MJ. In-the-bag secondary intraocular lens implantation in children. JAAPOS. Dec 1, 1999;3(6):350–355.
- Baradaran-Rafii A, Shirzadeh E, Eslani M, Akbari M. Optical correction of aphakia in children. J Ophthalmol Vis. Jan 2014;9(1):71.
- Trivedi RH, Wilson Jr ME, Facciani J. Secondary intraocular lens implantation for paediatric aphakia. JAAPOS. Aug 1, 2005;9(4):346–352. doi:10.1016/j.jaapos.2005.02.010.
- Shenoy BH, Mittal V, Gupta A, Sachdeva V, Kekunnaya R. Complications and visual outcomes after secondary intraocular lens implantation in children. Am J Ophthalmol. Apr 1, 2015;159(4):720–726. doi:10.1016/j.ajo.2015.01.002.
- Serafino M, Trivedi RH, Levin AV, et al. Use of the Delphi process in paediatric cataract management. Br J Ophthalmol. May 1, 2016;100(5):611–615. doi:10.1136/bjophthalmol-2015-307287.
- Sato T, Saito N. Contact lenses for babies and children. Contacto Dec 1959;3:419–424.
- Dabezies Jr OH. Defects of vision through aphakic spectacle lenses. Ophthalmol. Mar 1, 1979;86(3):352–379. doi:10.1016/S0161-6420(79)35503-8.
- Lambert SR, Buckley EG. Drews-Botsch C.A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: grating acuity and adverse events at age 1 year. Arch Ophthalmol. 2010;128:810–818.
- Amaya LG, Speedwell L, Taylor D. Contact lenses for infant aphakia. Br J Ophthalmol. Mar 1, 1990;74(3):150–154. doi:10.1136/bjo.74.3.150.
- Al Shamrani M, Al Turkmani S. Update of intraocular lens implantation in children. Saudi J Ophthalmol. Jul 1, 2012;26(3):271–275. doi:10.1016/j.sjopt.2012.05.005.
- Medsinge A, Nischal KK. Paediatric cataract: challenges and future directions. Clin Ophthalmol Auck NZ. 2015;9:77.
- Oh J, Shin HH, Kim JH, Kim HM, Song JS. Direct measurement of the ciliary sulcus diameter by 35-megahertz ultrasound bio-microscopy. Ophthalmol. Sep 1, 2007;114(9):1685–1688. doi:10.1016/j.ophtha.2006.12.018.
- Ishikawa H, Schuman JS. Anterior segment imaging: ultrasound bio microscopy. Ophthalmolol Clin NA. 2004 Mar;17(1):7. doi:10.1016/j.ohc.2003.12.001.
- Chen KP. Intraocular lens implantation in paediatric patients. In: Tasman W, Jaeger EA, eds. Duane’s Clin Ophthalmol. Vol. 6. Philadelphia: Lippincott-Raven. 1995:1–18.
- Sachdeva V, Katukuri S, Kekunnaya R, Fernandes M, Ali MH. Validation of guidelines for under correction of intraocular lens power in children. Am J Ophthalmol. Feb 1, 2017;174:17–22.
- Dahan E, Drusedau M. Choice of lens and dioptric power in paediatric pseudophakia. J Cataract Refract Surg. 1997;23:618–623. doi:10.1016/S0886-3350(97)80043-0.
- Enyedi LB, Peterseim MW, Freeman SF, Buckley EG. Refractive changes after paediatric intraocular lens implantation. Am J Ophthalmol. 1998;126(6):772–781. doi:10.1016/S0002-9394(98)00247-5.
- Shenoy BH, Mittal V, Gupta A, Sachdeva V, Kekunnaya R. Refractive outcomes and prediction error following secondary intraocular lens implantation in children: a decade- long analysis. Br J Ophthalmol.2013;97(12):1516–1519.
- Epley KD, Shainberg MJ, Lueder GT, Tychsen L. Paediatric secondary lens implantation in the absence of capsular support. JAAPOS. Oct 1, 2001;5(5):301–306. doi:10.1067/mpa.2001.117567.
- Abrar NA, Ashfaque M, Motaz B. Primary and secondary intraocular lens implantation in congenital cataract surgery: a retrospective comparative study of the visual outcomes. J Ophthalmol Clin Res. 2017.
- Koch CR, Kara-Junior N, Serra A, Morales M. Long-term results of secondary intraocular lens implantation in children under 30 months of age. Eye. 2018 Dec;32(12):1858–1863. doi:10.1038/s41433-018-0191-3.
- Wood KS, Tadros D, Trivedi RH, Wilson ME. Secondary intraocular lens implantation following infantile cataract surgery: intraoperative indications, postoperative outcomes. Eye. 2016 Sep;30(9):1182–1186. doi:10.1038/eye.2016.131.
- Rong X, Ji Y, Fang Y, Jiang Y, Lu Y. Long-term visual outcomes of secondary intraocular lens implantation in children with congenital cataracts. PloS one. Jul 31, 2015;10(7):e0134864. doi:10.1371/journal.pone.0134864.
- Zhao YE, Gong XH, Zhu XN, et al. Long- term outcomes of ciliary sulcus versus capsular bag fixation of intraocular lenses in children: an ultrasound bio-microscopy study. PloS one. Mar 16, 2017;12(3):e0172979. doi:10.1371/journal.pone.0172979.
- Mehta R, Aref AA. Intraocular lens implantation in the ciliary sulcus: challenges and risks. Clin Ophthalmolol. 2019;13:231. (Auckland, NZ)
- Siddiqui SN, Khan A. Visual outcome and changes in corneal endothelial cell density following aphakic iris-fixated intraocular lens implantation in paediatric eyes with subluxated lenses. JAAPOS. May 1, 2013;50(3):178–182.
- Sminia ML, Odenthal MT, Prick LJ, Mourits MP, Völker-Dieben HJ. Long-term follow-up of the corneal endothelium after aphakic iris-fixated IOL implantation for bilateral cataract in children. J Cataract Refract Surg. May 1, 2011;37(5):866–872. doi:10.1016/j.jcrs.2010.07.040.
- Rijneveld WJ, Beekhuis WH, Hassman EF, Dellaert MM, Geerards AJ. Iris claw lens: anterior and posterior iris surface fixation in the absence of capsular support during penetrating keratoplasty. J Cataract Refract Surg. Jan 1, 1994;10(1):14–19. doi:10.3928/1081-597X-19940101-04.
- Brandner M, Thaler-Saliba S, Plainer S, Vidic B, El-Shabrawi Y, Ardjomand N. Retropupillary fixation of iris-claw intraocular lens for aphakic eyes in children. PLoS One. Jun 25, 2015;10(6):e0126614. doi:10.1371/journal.pone.0126614.
- Gonnermann J, Amiri S, Klamann M, et al. Endothelial cell loss after retropupillary iris-claw intraocular lens implantation. Klinische Monatsbl. Jul 3, 2014;231(8):784–787.
- Cleary C, Lanigan B, O’Keeffe M. Artisan iris-claw lenses for the correction of aphakia in children following lensectomy for ectopia lentis. Br J Ophthalmol. Mar 1, 2012;96(3):419–421. doi:10.1136/bjophthalmol-2011-300579.
- Kumar M, Arora R, Sanga L, Sota LD. Scleral-fixated intraocular lens implantation in unilateral aphakic children. Ophthalmology. Nov 1, 1999;106(11):2184–2189. doi:10.1016/S0161-6420(99)90503-1.
- Kumar DA, Agarwal A, Agarwal A, Prakash G, Jacob S. Glued intraocular lens implantation for eyes with defective capsules: a retrospective analysis of anatomical and functional outcome. Saudi J Ophthalmol. Jul 1, 2011;25(3):245–254. doi:10.1016/j.sjopt.2011.04.001.
- Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmol. Aug 1, 2017;124(8):1136–1142. doi:10.1016/j.ophtha.2017.03.036.
- Turner RP, Owen L, Davidson J, Trivedi R, Wilson ME. Long-term outcomes of anterior chamber intraocular lens placement in a paediatric cohort. Pediatric Transplantation. 2015 Aug 1;19(4):e66. JAAPOS. doi:10.1111/petr.12447.
- Bluestein EC, Wilson ME, Wang XH, Rust PF, Apple DJ. Dimensions of the paediatric crystalline lens: implications for intraocular lenses in children. JAAPOS. 1996;33:18–20.
- Pandey SK, Werner L, Wilson Jr ME, Izak AM, Apple DJ. Capsulorhexis ovaling and capsular bag stretch after rigid and foldable intraocular lens implantation: experimental study in paediatric human eyes. J Cataract Refract Surg. Oct 1, 2004;30(10):2183–2191. doi:10.1016/j.jcrs.2004.02.079.
- Kohen T, Fabian E, Gerl R, Hunold W, Hutz W, Strobel J. Optic edge design as long-term factor for posterior capsular opacification rates. Ophthalmol. 2008;115:1308–1314. doi:10.1016/j.ophtha.2008.01.002.
- Chang DF. “Single versus three-piece acrylic IOLs. Br J Ophthalmol. 2004;88:727–728. doi:10.1136/bjo.2004.040063.
- Khan AO, AlGaeed A. Paediatric secondary intraocular lens estimation from the aphakic refraction alone: comparison with a standard biometric technique. Br J Ophthalmol. Dec 1, 2006;90(12):1458–1460. doi:10.1136/bjo.2006.100834.
- Vasavada AR, Trivedi RH, Nath VC. Visual axis opacification after AcrySof intraocular lens implantation in children. J Cataract Refract Surg. 2004;30:1073–1081. doi:10.1016/j.jcrs.2003.08.020.
- Nihalani BR, Vanderveen DK. Secondary intraocular lens implantation after paediatric aphakia. JAAPOS. Oct 1, 2011;15(5):435–440. doi:10.1016/j.jaapos.2011.05.019.
- Trivedi RH, Wilson ME, Bartholomew LR, Lal G, Peterseim MM. Opacification of the visual axis after cataract surgery and single acrylic intraocular lens implantation in the first year of life. JAAPOS. 2004;8:156–164.