Scientific and technical advancements provided a deeper insight into the cellular and molecular processes of the host immunity and its clinical significance in various aspects of human health, including organ transplantation. Improved surgical and medical management, along with immunosuppressive drugs, allowed big leaps in clinical organ transplantation. However, preexisting antibodies, either as blood group isoagglutinins or through allosensitization, remain a major roadblock for successful and sustainable organ transplantation. This special issue of International Reviews of Immunology discusses the antibodies produced by the recipient against antigens on the graft known as donor-specific antibodies, (DSAs) after transplantation and its overall outcome in case of the intestine and liver transplant. Additionally, this issue also discusses the challenges linked with the more recent assays for DSAs.
The development of HLA antibodies (allosensitization) can occur following exposure to foreign HLA through pregnancy and blood transfusion, but it may also be triggered by HLA‐unrelated immune stimuli such as Hepatitis B vaccine or tuberculin skin test. More relevant to the discussion, organ transplant recipients can also produce antibodies against the HLA epitopes of the graft (donor-specific HLA antibodies, DSAs) after transplantation. The presence of DSAs against human leukocyte antigen (HLA) is strongly associated with an increased risk of rejection and graft loss, particularly if the antibodies were raised after transplantation (de-novo DSAs). The HLA antibody testing has become a critical part of both pre‐transplant recipient assessment as well as pre and post‐transplant management because it can trigger several innate and subsequently adaptive immune responses. Furthermore, increasing evidence confirms that DSA are mechanistically relevant to the development of microvascular alterations, which are the hallmark of chronic rejection. However, antibody effector functions are dependent on several factors, including antibody concentration, antigen availability, and antibody isotype/subclass, making a definitive risk assessment difficult. The first review article of this issue is an attempt to discuss different immunoassays by Kofoeld-Nielsen and Moeller, particularly solid phase immunoassays and the pros and cons associated with this assay.
Much of the information available on anti-HLA antibody response after organ transplantation as well as the clinical significance of circulating HLA antibodies have been obtained from kidney allograft recipients and has been the topic of countless reports and reviews. However, the impact of DSAs following the transplantation of other abdominal organs is less extensively studied and seems to differ from kidney transplantation. It has been observed that the existence of preformed DSAs is of little concern during liver transplantation and that HLA antibodies (particularly Class I antibodies) are cleared within hours from liver graft reperfusion. The exact mechanisms remain unknown but several mechanisms including the adsorption of preexisting recipient antibodies or HLA-I soluble antigen production. These initially empirical findings have led to the uneventful performance of numerous combined liver-kidney transplants in the presence of a positive crossmatch. However, more recent data confirm that de-novo DSA are associated with liver graft failure. Similarly, almost 20% of a large cohort of intestinal graft recipients developed de-novo DSAs, and a significant association between DSAs and the severity of rejection episodes was found in intestinal graft recipients suggesting that DSAs may work synergistically with cell-mediated mechanisms. Herein, Wozniak and Venick review the emerging field of DSAs after liver and intestinal transplantation and provide all the essential information as well as a set of recommendations for the HLA antibody screening in this patient population. This review raises the awareness of immunologists and clinicians on the significance and impact of DSAs on the early and late results of liver and intestinal transplantation.
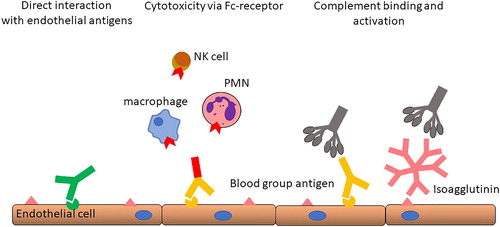
In spite of biological and immunological differences between the simpler anti-A and anti-B antibodies and the much more heterogenous anti-HLA antibodies, several significant similarities exist both regarding the mechanisms of injury and the management of allograft sensitized recipients or recipients of ABO-incompatible grafts (). The effect of preexisting antibodies is immediate and may cause acute or hyperacute graft loss in the immediate period after the transplant through immunological reactions such as complement-mediated endothelial injury and thrombosis. Consequently, antibody removal is needed and the suppression of B‐cell response immediately after transplantation is essential to achieve accommodation. Selective removal of isoagglutinins is possible and its titers are easy to quantify. In this issue, Skogsberg and Bennet summarize the current knowledge and protocols and review the results following ABO-incompatible liver transplantation. As outlined in their contribution, several clinical strategies are available, safely allowing both emergency or elective liver transplantation in circumstances when suitable, blood-group compatible donors are lacking ().
These reviews may benefit the broad readers such as clinician and researchers working in transplantation immunobiology and its interfaces.
References
- Koefoed-Nielsen P, Møller BK. Donor-specific anti-HLA antibodies by solid phase immunoassays: advantages and technical concerns. Int Rev Immunol 2019;38(3):95–105. doi:10.1080/08830185.2018.1525367
- Wozniak L, Venick R. Donor-specific antibodies following liver and intestinal transplantation: clinical significance, pathogenesis and recommendations. Int Rev Immunol 2019;38(3):106–117. doi:10.1080/08830185.2019.1630404
- Dahlgren US, Bennet W. ABO-incompatible liver transplantation - a review of the historical background and results. Int Rev Immunol 2019;38(3):118–128. doi:10.1080/08830185.2019.1601720