Abstract
Creation of arteriovenous fistula (AVF) may lead to left ventricle hypertrophy and predispose for development or worsening of heart failure. It was postulated to reduce access blood flow if exceeded 2 L/min or cardiac index was higher than 3.0 L/min/m2. Numbers of techniques decreasing flow were described. The major disadvantage was the complexity of procedure and necessity of intraoperative flow measurement needed to establish desired flow. The technique of dilator-assisted banding with no endovascular catheterization is presented. After blunt dissection non absorbable thread was placed around vessel and tied over the dilator. Then the dilator was gently removed and blood flow was confirmed by palpation. We performed 12 banding procedures. Mean brachial blood flows were 3733.2 ± 826.2 mL/min preoperatively and 1461.2 ± 337.7 mL/min after surgery. Mean flow reduction was 2272.2 ± 726.9 mL/min. The external dilator-assisted banding is a feasible method for vascular access flow reduction without necessity of endovascular catheterization.
Introduction
Creation of arteriovenous fistula (AVF) increases cardiac output and may predispose for development or worsening of heart failure. Moreover, it may lead to left ventricle hypertrophy and pulmonary hypertension.Citation1 Although high flow rates (>1500 mL/min) were found in 19.1% of 820 incident hemodialysis patients, there were no associations with increased risk of death.Citation2 Evaluation for symptoms of excessive blood flow is recommended.Citation3 It was postulated to reduce access blood flow if exceeded 2 L/min or cardiac index was higher than 3.0 L/min/m2, and after solving anemia, over hydration and hypertension.Citation3,Citation4 Among various options for vascular access flow restriction,Citation3–8 there are methods allowing for standardized inflow decrease.Citation9,Citation10 The aim of the study is to present the utility of external dilator-assisted banding (EDAB) with no endovascular catheterization.
Materials and methods
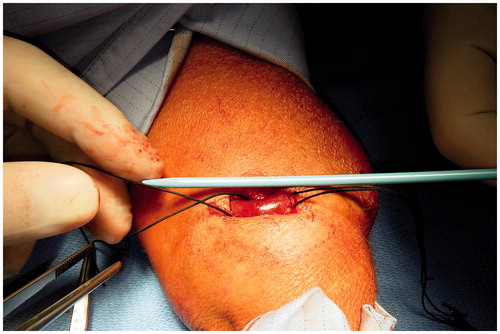
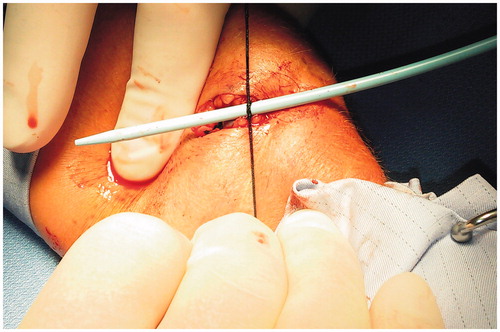
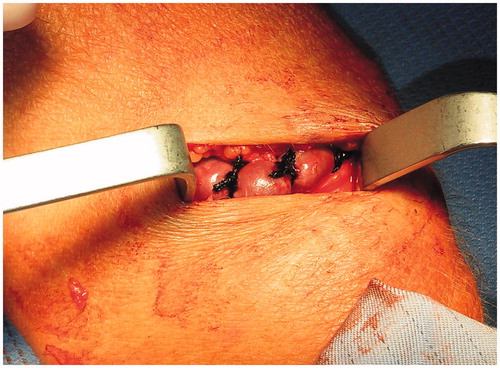
The clinical data of patients who underwent restriction of AVF flow in 2015 were retrospectively reviewed. All patients underwent Doppler ultrasound evaluation before and after procedure. Diameters of upper extremity arteries were measured. Brachial artery blood flow was assessed before and after surgery on the arm with AVF. The study group included 12 patients, 7 women and 5 men. They were 30–77 years old, mean 54 ± 12.7 years. Three patients were hemodialyzed, eight were after kidney transplantation, and a last woman was waiting for dialysis initiation. AVFs were functioning 3–32 years, mean 10.6 ± 8.2 years. In four patients signs of heart failure were present. All patients had cardiac hypertrophy on echocardiography. No signs of distal ischemia were found. An informed consent was taken from all patients before surgery. All procedures were done in local anesthesia with 1% solution of lidocaine. Skin was incised above the vessel chosen for banding. For upper arm AVFs the procedure was conducted on the vein just distal to anastomosis. For forearm AVFs banding was performed on the radial artery just proximal to anastomosis. Non absorbable thread around artery or vein, respectively, was placed after blunt dissection. Then vascular dilator was placed along exposed vessel (). We used 10-French dilator (diameter of 3.3 mm) for vein banding of each high flow upper-arm AVF and forearm AVF (artery banding) in case of end-to-end radial artery-cephalic vein anastomosis. If the side-to-end radial-cephalic AVF was found 8-French dilator (diameter of 2.7 mm) was used for narrowing of feeding artery. Sutures were tied over the dilator until the thrill disappeared (). Two or three ligatures were placed within 1 cm distance. Dilator was gently removed and blood flow was confirmed by palpation (). Afterwards, the wound was sutured and dressed.
Results
Preoperative brachial artery diameters ranged from 7.1 to 12.7 mm. Radial artery diameters for distal AVFs were 4.7–7.7 mm. Mean brachial blood flows were 3733.2 ± 826.2 mL/min preoperatively (ranged from 2774 to 5118 mL/min) and 1461.2 ± 337.7 mL/min after surgery (from 950 to 2003 mL/min). Mean flow reduction after EDAB was 2272.2 ± 726.9 mL/min (from 1648 to 3262 mL/min). Within one to 10 months of follow up no AVF thrombosis was recorded. The detailed results are given in .
Table 1. Vascular access data in studied patients.
Discussion
High-flow fistula can be asymptomatic or result in high output cardiac failure, pulmonary hypertension and distal hypoperfusion ischemic syndrome. Paradoxically, dialysis through hyper functional access could be inadequate due to high cardiopulmonary recirculation.Citation8 Presence of AVF is well tolerated by majority of patients, but its effect on cardiovascular system cannot be omitted.Citation1 Also in the analyzed group, AVFs were well tolerated and signs of cardiac failure were mild. Recently, the idea of reduction of peripheral resistance by AVF was used to treat uncontrolled hypertension.Citation11 Moreover, creation of AVF is thought to slower progression of chronic kidney disease.Citation12 Even after kidney transplantation with suboptimal, impaired graft function most physicians prefer AVF blood flow reduction as a safer option rather than fistula ligation.Citation13
Numbers of techniques decreasing flow were described. The reduction of flow is based on increase of resistance at level of anastomosis or venous outflow.Citation4 For distal hyper flow AVFs proximal radial artery ligationCitation6 could be effective intervention. Of course, it is appropriate only for side-to-end anastomosed fistulas.Citation14 Reduction of flow could be achieved with spindle-like narrowing suture near the anastomosis. Intraoperative flow measurement was needed to establish desired flow. PTFE strip was placed around narrowed segment to prevent vein dilatation and flow increase.Citation5 Other technique was T-banding, that avoids anastomotic aneurisms.Citation15 Revision using distal inflow (RUDI) was another procedure used for treatment of high-flow AVF.Citation6 Two methods of guided flow reduction procedures were presented previously. In MILLER procedure (minimally invasive limited ligation endoluminal-assisted revision), an intraluminal balloon was used as a sizing dowel. Initial banding was successful in 94% of patients with high-flow access. In this group of patients primary band patency at 6 months was 86%. The band size ranged from 2.5 to 6 mm for AVFs. The most common (in 57% of patients) first band size was 4 mm. It is noteworthy, that the highest risk of complication for MILLER technique was found in grafts and the lowest thrombotic event rate was for forearm fistulas.Citation9 In dilator-assisted banding (DAB) over-the-wire vascular dilators of known diameters were used as guides.Citation10 Although, the methods are quite simple, they both have the same disadvantage, necessity of vessel puncture and device insertion. For MILLER technique also radiology suite is needed. The method we propose is very easy and reproducible, it allows for precise banding without necessity of vessel assessing. Moreover, fluoroscopic guidance is not required. We suppose that EDAB is especially useful for reduction of flow in long standing distal AVFs originating from radial artery. Placing ligature on radial artery should reduce the risk of aneurysmal dilatation of anastomotic area. Moreover, banding close to anastomosis should avoid recurrence of high flow due to development of collaterals. The obvious limitation of the observation is small number of patients and short follow up. The long term outcome and risk of thrombosis cannot be predicted, but flows exceeding 1 L/min found in majority of our patients should be enough for avoidance of access thrombosis. Moreover, due to small number of patients and short observation we cannot conclude on impact of AVF banding on cardiac function. Satisfactory results of MILLER technique and simplicity of our method should be encouraging for broader use of EDAB. The technique is an easy and feasible method for vascular access flow reduction.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Alkhouli M, Sandhu P, Boobes K, Hatahet K, Raza F, Boobes Y. Cardiac complications of arteriovenous fistulas in patients with end-stage renal disease. Nefrologia. 2015;35:234–245.
- Al-Ghonaim M, Manns BJ, Hirsch DJ, Gao Z, Tonelli M, Alberta Kidney Disease Network. Relation between access blood flow and mortality in chronic hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:387–391.
- Kukita K, Ohira S, Amano I, et al. 2011 update Japanese society for dialysis therapy guidelines of vascular access construction and repair for chronic hemodialysis. Ther Apher Dial. 2015;19:1–39.
- Basile C, Lomonte C. When and how should an arterio-venous access be modified because of a high blood flow rate? Semin Dial. 2011;24:396–398.
- Zanow J, Petzold K, Petzold M, Krueger U, Scholz H. Flow reduction in high-flow arteriovenous access using intraoperative flow monitoring. J Vasc Surg. 2006;44:1273–1278.
- Chemla ES, Morsy M, Anderson L, Whitemore A. Inflow reduction by distalization of anastomosis treats efficiently high-inflow high cardiac output vascular access for hemodialysis. Semin Dial. 2007;20:68–72.
- Padberg FT Jr, Calligaro KD, Sidawy AN. Complications of arteriovenous hemodialysis access: Recognition and management. J Vasc Surg. 2008;48:55S–80S.
- Sequeira A, Tan TW. Complications of a high-flow access and its management. Semin Dial. 2015;28:533–543.
- Miller GA, Goel N, Friedman A, et al. The MILLER banding procedure is an effective method for treating dialysis-associated steal syndrome. Kidney Int. 2010;77:359–366.
- Wang S, Almehmi A, Packer J. Dilator-assisted banding for managing complications associated with excessive hemodialysis access flow. Semin Dial. 2013;26:100–105.
- Lobo MD, Sobotka PA, Stanton A, et al. Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): A randomised controlled trial. Lancet. 2015;385:1634–1641.
- Golper TA, Hartle PM, Bian A. Arteriovenous fistula creation may slow estimated glomerular filtration rate trajectory. Nephrol Dial Transplant. 2015;30: 2014–2018.
- Yaffe HC, Greenstein SM. Should functioning AV fistulas be ligated after renal transplantation? J Vasc Access. 2012;13:405–408.
- Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van Laere O, Raynaud A. Proximal radial artery ligation (PRAL) for reduction of flow in autogenous radial cephalic accesses for haemodialysis. Eur J Vasc Endovasc Surg. 2010;40:94–99.
- Schneider CG, Gawad KA, Strate T, Pfalzer B, Izbicki JR. T-banding: A technique for flow reduction of a hyperfunctioning arteriovenous fistula. J Vasc Surg. 2006;43:402–405.