Abstract
Background: Strategies used to teach nephrology to medical students are not well studied. This study assesses the published literature on medical student education in nephrology.
Methods: A review of the published literature on nephrology education for medical students was conducted on two major online search engines (PubMed and ERIC). In addition, references of the manuscripts discovered in these searches were reviewed. The empirical studies were categorized by subject within nephrology and research design.
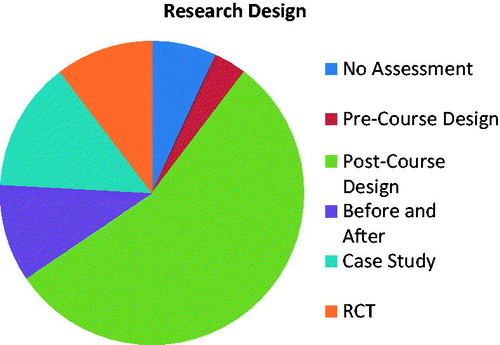
Results: We found 26 original studies in which a method of teaching nephrology to medical students was described. The studies dated from 1977 to 2015. The focus of these nephrology teaching experiences was as follows: anatomy (6.5%), physiology (22.6%), pathophysiology (29.0%), pathology (6.5%), treatment (25.8%), and general nephrology (9.7%). The studies were also categorized into various types of research design. 6.9% had either no assessment of the educational experience or had a description too vague to categorize it; 3.4% involved a survey about the existing educational approach before a curriculum change was implemented; 55.2% used surveys or tests after an educational course was carried out; 10.3% sought feedback from students before and after the educational experience; 13.8% were case studies; and 10.3% included a randomized controlled trial. The randomized controlled trials involved teaching techniques focused on the pathophysiology of renal disease.
Conclusions: Rigor was lacking in most empirical studies on medical student education in nephrology. Well-designed randomized controlled studies are needed to accurately assess the effectiveness of the educational techniques introduced into medical school curricula.
Introduction
Over the last decade, there have been several publications documenting a decline in the number of United States medical graduates pursuing nephrology fellowships.Citation1–6 This concerning finding is magnified by the reality that an aging population and rising incidence of such chronic diseases as diabetes mellitus and hypertension continue to increase the demand for specialists, including nephrologists.
Recent studies suggest that experiences in medical school – both positive and negative – can influence a medical trainee’s decision to pursue nephrology. Limited medical student exposure to clinical nephrology,Citation7 confusing methods of teaching complex material,Citation7 a dearth of nephrology courses taught by nephrologists,Citation2 and the widespread view of nephrology as a highly specialized field focused on rare and severe diseasesCitation8 may contribute to apathy toward a career in nephrology. Conversely, effective teaching and role models may explain the finding of a studyCitation6 that over 20% of nephrology fellows first became interested in the field during medical school.
These studies suggest that medical school is an important time for medical trainees to become interested or disinterested in nephrology, and therefore that it would be an appropriate target of intervention.Citation7 Yet little is known about existing approaches to teaching nephrology to medical students. In this article, we review the strategies being employed to teach different topics of nephrology to medical students and the extent to which those methods have been successful.
Methods
We conducted a review of the English published literature on nephrology education of medical students using two major online academic search engines, PubMed and Education Resources Information Center (ERIC). This study was deemed exempt by the Institutional Review Board at Northwell Health. After our search, we were assisted by a librarian who conducted an additional review. Together, we used the following keywords in our searches: “medical students,” “nephrology,” “education,” “kidney,” and “teaching.” We also reviewed references of the papers discovered in these searches. Exclusion criteria were abstracts, articles that focused on nephrology education of trainees other than medical students (e.g. internal medicine residents, nephrology fellows, or college physiology students), and articles providing commentary on medical school education of nephrology without an accompanying empirical study. We did not limit the review by the year of publication or geography.
We categorized the empirical studies by subject within nephrology based on the primary focus of the teaching method: anatomy, physiology, pathophysiology, pathology, treatment, and general nephrology. We then recorded the research design of each study using a list (see ) adapted from Beckman and Cook.Citation9 Questionnaires, evaluations, and feedback are grouped under the umbrella term “surveys.” Finally, for studies that included an assessment of the teaching method, we noted factors that appeared to contribute to the success of the educational experience.
Table 1. Types of study designs for research of medical education.
Results
We identified 26 publications in which an original method of teaching nephrology to medical students was described (see ). The publications dated from 1977 to 2015. Three studies utilized two different educational research designs. Five studies covered two different subject materials.
Table 2. 26 Publications describing medical student education of nephrology.
There were many (more than 25) publications that were discovered in the original search but were excluded in our study because they focused on the education of learners other than medical students, lacked an empirical trial, were published as abstracts, or were not written in English.
depicts the breakdown of studies by subject material. portrays the breakdown of studies by research design.
Figure 1. Subject material: anatomy (6.5%), physiology (22.6%), pathophysiology (29.0%), pathology (6.5%), treatment (25.8%), and general nephrology (9.7%).
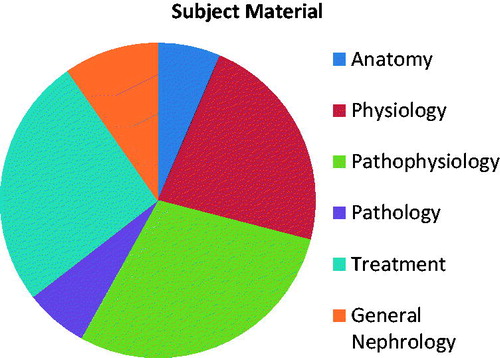
Figure 2. Research design: 6.9% had either no assessment of the educational experience or had a description too vague to categorize it; 3.4% involved a survey about the existing educational approach before a curriculum change was implemented; 55.2% used surveys or tests after a practice was carried out; 10.3% sought feedback from students before and after the educational experience; 13.8% were case studies; and 10.3% included a randomized controlled trial. There were no ethnographic studies.
Medical student assessment
Each of the studies categorized above aimed to assess the success of an innovational approach to teaching nephrology to medical students. There were four major threads that ran through the publications.
First, several studies support the notion that interactive teaching of nephrology is crucial to the engagement and therefore learning of medical students. For example, Brands and SchumacherCitation10 found that students appreciated small group problem-solving sessions and worksheet exercises. Dietz and StevensonCitation11 engaged students with clicker questions designed to facilitate active learning. These authors also used group exercises and faculty-led class-wide discussions, and they reduced time spent in traditional lectures. ElzubeirCitation12 championed problem-based learning as an effective method to allow students to develop new skills while building on prior knowledge. Shafi et al.Citation13 claimed that “integrated learning is the need of the hour” and used “large-group interactive sessions, small group learning, problem-based learning, practical, and self-directed learning” to maximize efforts to fulfill that need.
Second, many authors considered the value of technology in educating their students. In 1993, Rabushka et al.Citation14 advocated for the use of an interactive computer program to teach medical students to evaluate and manage renal masses. Leong et al.Citation15 offered computer cases to fill gaps in students’ clinical experiences during their clerkships. Brands and SchumacherCitation10 used patient simulations to teach renal physiology, and Kalinski et al.Citation16 presented 3D visualizations of renal pathological specimens to improve education in renal pathology. Telemedicine was advanced by Bramstedt et al.,Citation17 in which medical students who conducted interviews via Skype with dialysis patients had improved understanding of the psychosocial burdens of dialysis and increased empathy toward patients.
Third, there were studies that highlighted the importance of clinical relevance in effective education of nephrology. Harrison-BernardCitation18 began sessions with “hooks” that situated basic science topics within a clinical context in order to maintain student interest. Ali and LewingtonCitation19 called for a more clinically relevant training in acute kidney injury, and Dietz and StevensonCitation11 found success in using clinical cases to engage students in a more active learning process. However, Shafi et al.Citation13 reported that the overemphasis of clinical relevance in their renal module was perceived as a negative by students.
Finally, a number of authors encouraged the use of concept maps to teach pathogenesis of disease. Preiss et al.Citation20 found that students who used concept graphics were better able to organize and remember their newly acquired knowledge. Students in a study by Ho et al.Citation21 performed better on their quizzes after using pathogenesis maps, and they reported enjoying the exercises because they felt encouraged to do more self-directed learning. McLaughlin and MandinCitation22 connected students’ use of ‘schemes’ – internal representations of knowledge – and success on a concept sorting task to improved scores on questions relating to metabolic alkalosis. Novak et al.Citation23 was a follow-up study that raised the idea that diagnostic schemes help to build long-term knowledge.
Educational study design
Two studies had no structured assessment of the educational approach that was introduced to students. Schwartz and RauchCitation24 developed a 38-page course study guide that covered the major topics in pediatric nephrology and organized a weekly seminar with staff to emphasize major points and allow students to ask questions. The authors merely reported that “…their [the students’] comments have been complimentary,” so the extent to which the study met its goals of providing organization to the students’ study time and ensuring standardization of the students’ learning cannot be adequately gauged. Similarly, Harrison-BernardCitation18 described a method of teaching the renal renin-angiotensin system to first year medical students without an assessment of that method.
Several studies used surveys with qualitative and quantitative components in order to examine student preference of teaching technique or assess the extent to which those techniques contributed to improved knowledge. In some of these studies, surveys were distributed before the new technique was presented (“pre-course designs”); others circulated surveys after the new technique was presented (“post-course designs”); and still others disseminated surveys both before and after the technique was introduced (“before and after studies”). In the quantitative sections, respondents were typically asked to rate certain features of the teaching method on a scale, and their ratings were then averaged. In the qualitative parts, respondents provided feedback about the teaching experience and answered questions about changes in their perceived understanding of a topic in nephrology after the teaching experience. Most publications incorporated both quantitative and qualitative assessment. For example, in order to determine the effectiveness of its problem-based learning curriculum during the renal system block in first year of medical school, ElzubeirCitation12 used Likert-type rating scales to measure the extent to which students found the problems relevant, stimulating, and educational. There was also an opportunity for students to comment on aspects of the problem-based learning that they appreciated or would like to see changed. However, without a control group, even surveys that compared students’ impressions before and after an educational experience are unable to reliably assess the impact of the intervention.
Furthermore, many of these publications are missing details regarding the surveys used to assess the outcomes of their teaching method. Schwab and Knox,Citation25 for instance, described a laboratory experiment in which students administered diuretics to anesthetized dogs in an effort to improve their understanding of the physiology of diuretics. The authors concluded that the experience was effective but provided only the following evidence: “Of the students responding to our questionnaire, 72% felt this laboratory was a good to excellent learning experience.” Similarly, after describing the use of an interactive computer program to teach the evaluation and management of renal masses, Rabushka et al.Citation14 simply stated that the “comments and suggestions” they received from residents, staff, and medical students indicated that they “enjoy the interactive nature of the program and the hypermedia environment.” Without specific information about the nature of the surveys, it is difficult both to assess the extent to which the educational methods made a difference in students’ learning and to apply the approach to other trainee groups.
In some studies, the authors administered tests to assess student knowledge of subjects related to the kidney and to evaluate the effectiveness of the educational approach introduced to the students. For example, Arger et al.Citation26 described a pilot sonography course aiming to teach students anatomy of the aorta and right kidney through experience with ultrasound technology. The authors gave students an identical test in the first and final weeks of the course with questions that focused on the “clinical diagnostic sonography of the aorta and kidney” and concluded based on these tests that exposure to sonography improved student comprehension of the relevant anatomy. Lack of control group again limits the internal validity of these studies.
There were four case studies in which the knowledge of students was assessed through observing the skills they demonstrated during a clinically-related task. Wimmers et al.Citation27 showed that if the patient’s history and physical findings were not provided in a case (i.e. only lab data was present), intermediate recall (at the level of advanced medical students) was equivalent to expert recall (at the level of nephrology attendings). However, when asked to think aloud and elaborate on how the presented lab data related to the patient’s problem, experts outperformed intermediates. McLaughlin and MandinCitation22 and McLaughlin et al.Citation28 evaluated the teaching of different clinical presentations (metabolic alkalosis in the former study; hyponatremia, hyperkalemia, metabolic acidosis, and metabolic alkalosis in the latter study) to first year medical students. The authors found the use of concept schemes to be an effective way of learning about patients with such presentations. Specifically, McLaughlin et al.Citation28 reported an “independent association between expert-type concepts in knowledge structure and diagnostic success” as well as “between the use of diagnostic schemes by preceptors and the number of expert-type concepts in knowledge structure in students.” Lastly, Kiesewetter et al.Citation29 instructed students to think aloud about three cases related to renal disease (hematuria due to glomerulonephritis, symptoms of acute renal failure and depression, and hypertensive crisis due to renal artery stenosis) and found that in 56% of cases, students employed cognitive actions that used “higher level reasoning,” which the authors believed may have improved the students’ diagnostic capabilities. Although lessons can be learned from the observations made in these studies, there were limited numbers of participants, and many relied on cognitive reasoning that was expressed verbally with no ability to account for any connections made that were not explicitly shared with the data collectors.
There were only three randomized controlled trials in the 26 publications. They all involved teaching techniques focused on the pathophysiology of renal disease. In Preiss et al.,Citation20 second year medical students who had volunteered to be part of the study were randomly divided into two groups. Each group was provided with a text that summarized 13 pathological conditions in nephrology. The experimental group was also given color photocopies of graphic summaries of those 13 pathological conditions and an accompanying glossary. Both groups were given 30 min to study. Then both groups were given a short quiz with four “memorization questions” (which tested the memorization of a single fact associated with one pathology) and five “correlation questions” (which tested the ability to correlate “two or more causally related facts of a characteristic of a given pathology”). Grades were significantly higher in the experimental group for the correlation questions, but no difference was observed for the memorization questions. The grader of the quizzes was not involved in the study and was blinded to the group identity of the students. The authors concluded that concept graphics aid students’ understanding of complex subjects, possibly through the representation of patterns unique to distinct pathologies.
In the second randomized controlled trial, Leong et al.Citation15 had medical students read two articles, and complete either a paper case or a computer case on low back pain associated with kidney stones. Though randomly assigned to each of these interventions, the medical students were again a self-selected group of students who had volunteered to test the computer cases. The authors found no statistical significance among the groups in learning preferences, but the students rated the computer case highest on a 10-point scale in response to the question, “Do you think the case study was helpful?” (8.0 for the computer case vs. 7.4 for the paper case and 6.5 for the articles). There was also no significant difference on the post-test administered to the students in this study. The authors commented that “students reported enjoying the computer format” and that “this educational method proved at least as effective as the others tested.”
Finally, Ho et al.Citation21 is a crossover study in which medical students were randomized to receive either access to online pathogenesis concept maps related to acute kidney injury and chronic kidney disease or links to sections of the existing pathology textbook (Robbins Basic Pathology) that covered the same concepts. In the subsequent block on hepatic disease, the groups crossed over in their access to concept maps on alcoholic liver disease and complications of cirrhosis; both groups then received access to concept maps in the final block on pancreatic disease. An online assessment that was given to both groups at the end of each block showed a significantly higher quiz score in the group that received access to the concept maps on questions related to the pathogenesis of renal disease. This difference between the two groups was seen also on the assessments on hepatic disease, and there was no difference between the groups on any of the questions in the assessment on pancreatic disease. The authors argued that their results demonstrate the effectiveness of concept maps in teaching students about disease processes.
Discussion
To our knowledge, this study marks the first analysis of published empirical studies designed to teach nephrology to medical students. Our research reveals that rigor is lacking in research on medical student education in nephrology.
Overall, only three published studies in the literature used a study design with randomization and a control group. These studies point toward the usefulness of concept maps and computer cases in helping medical students learn about the pathophysiology of renal disease. Still, the success of these approaches was gauged mainly by student report and tests taken immediately after a course, so the long-term impact of these educational approaches remains unknown. Most importantly, the results of these studies cannot attest to improved patient outcomes as a result of the employed educational methods.
Our findings support the conclusion of a recent review,Citation30 in which the authors noted a paucity of high quality medical education research in nephrology as compared to other areas of medicine. We encourage the use of carefully designed randomized controlled trials (seeCitation31) as have been conducted in other areas of medical education. In cardiology, for instance, there are several randomized controlled studies that assess medical students’ learning of cardiac auscultation,Citation32–34 electrocardiogram interpretation,Citation35–37 and cardiac ultrasound exams.Citation38,Citation39 Similarly, in pulmonary medicine and critical care, randomized controlled trials exist to evaluate the value of ultrasound on learning the clinical exam,Citation40 the effectiveness of counseling techniques on smoking cessation,Citation41,Citation42 and the impact of simulation-based training on managing dyspneaCitation43 and septic shock.Citation44 Other studies randomized medical students to different educational modalities to determine how students most effectively learn to use proper pressurized metered dose inhalersCitation45 and to recognize agonal breathing as a sign of cardiac arrest.Citation46 As a final example, randomized controlled studies in gastroenterology have assisted in ascertaining the effects of various educational experiences, including: 3D visualizations on learning of liver anatomy,Citation47,Citation48 role-playing and simulations in the learning of digital rectal exam,Citation49 and abdominal ultrasound training in learning the physical examination of the abdomen.Citation50 Further studies assess the value of computer-aided learning on student understanding of the anatomy and physiology of the liver and biliary tree,Citation51 as well as the influence of peer teaching on students’ knowledge acquisition and retention in a gastroenterology/hematology course.Citation52
More rigorous studies are needed in the field of nephrology to reliably assess the effectiveness of the educational techniques used for teaching the subject to medical students. Though a complete training of nephrologists to conduct such studies is beyond the scope of this article, we offer the following recommendations on improving the rigor of nephrology education studies based on our experience in undergraduate medical education:
Clinicians should be trained via certificate courses and degree programs to conduct education research. Examples include the medical education research training at the Association of American Medical CollegesCitation53 and Harvard Macy Institute.Citation54
A general three-step method, as recently outlined in an article on this subject,Citation30 is to (a) refine and clearly articulate the study question; (b) identify the design and methods for the qualitative or quantitative study; and (c) select outcomes and outcome methods (see #3).
Trials should measure changes in patient-centered outcomes in addition to changes in student knowledge. The results of such studies will provide a more significant contribution to the field of nephrology. They are also more likely to garner funding from sources that focus on patient care.
In conclusion, rigor is lacking in the design of studies on medical student education of nephrology. Well-designed randomized controlled studies are needed to accurately assess the effectiveness of the educational techniques introduced into medical school curricula.
Acknowledgements
We would like to thank Leanna Stager, Scholarly Publications Librarian at the Hofstra Northwell School of Medicine, who assisted the authors in the literature review. Sarah D. Bayefsky is a senior medical student at the Hofstra Northwell School of Medicine. Dr. Hitesh H. Shah serves on the American Society of Nephrology (ASN) Workforce and Training Program Director Executive Committees. Dr. Kenar D. Jhaveri serves on the ASN Education Committee.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Adams ND. Attracting more residents into nephrology. Clin J Am Soc Nephrol. 2012;7:1382–1384.
- Hoenig MP, Shapiro E, Hladik GA. Lessons learned from the ASN renal educator listserv and survey. Clin J Am Soc Nephrol. 2013;8:1054–1060.
- Jhaveri KD, Sparks MA, Shah HH, et al. Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis. 2013;61:540–546.
- Parker MG, Ibrahim T, Shaffer R, Rosner MH, Molitoris BA. The future nephrology workforce: Will there be one? Clin J Am Soc Nephrol. 2011;6:1501–1506.
- Parker MG, Pivert KA, Ibrahim T, Molitoris BA. Recruiting the next generation of nephrologists. Adv Chronic Kidney Dis. 2013;20:326–335.
- Shah HH, Jhaveri KD, Sparks MA, Mattana J. Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol. 2012;7:1513–1520.
- Patel AB, Balzer MS. On becoming a nephrologist: Medical students' ideas to enhance interest in a career in nephrology. Am J Kidney Dis. 2013;62:450–452.
- Piccoli GB, Burdese M, Bergamo D, et al. Teaching technology with technology: Computer assisted lessons in the medical school – The first Italian experience in nephrology and dialysis. Int J Artif Organs. 2002;25:860–866.
- Beckman TJ, Cook DA. Developing scholarly projects in education: A primer for medical teachers. Med Teach. 2007;29:210–218.
- Brands MW, Schumacher L. Active learning strategies to teach renal-cardiovascular integration with high student-to-teacher ratios. Adv Physiol Educ. 2009;33:282–285.
- Dietz JR, Stevenson FT. Active learning in a large medical classroom setting for teaching renal physiology. Adv Physiol Educ. 2011;35:456–459.
- Elzubeir MA. Teaching of the renal system in an integrated, problem-based curriculum. Saudi J Kidney Dis Transpl. 2012;23:93–98.
- Shafi R, Quadri KHM, Ahmed W, Mahmud SN, Iqbal M. Experience with a theme-based integrated renal module for a second-year MBBS class. Adv Physiol Educ. 2010;34:15–19.
- Rabushka LS, Fishman EK, Goldman SM, Hennessey JG, Nixon MS. Development of a computer-assisted instructional tool for evaluation and treatment of renal masses. An experiment in hypermedia. Invest Radiol. 1993;28:169–174.
- Leong SL, Baldwin CD, Adelman AM. Integrating web-based computer cases into a required clerkship: Development and evaluation. Acad Med. 2003;78:295–301.
- Kalinski T, Zwönitzer R, Jonczyk-Weber T, Hofmann H, Bernarding J, Roessner A. Improvements in education in pathology: Virtual 3D specimens. Pathol Res Pract. 2009;205:811–814.
- Bramstedt KA, Prang M, Dave S, et al. Telemedicine as an ethics teaching tool for medical students within the nephrology curriculum. Prog Transplant. 2014;24:294–297.
- Harrison-Bernard LM. The renal renin-angiotensin system. Adv Physiol Educ. 2009;33:270–274.
- Ali MN, Lewington AJP. Do medical trainees receive adequate training in the management of acute kidney injury? Renal Failure. 2011;33:669–671.
- Preiss B, Black R, Caron C, Shapcott D. Graphic summaries of expert knowledge for the medical curriculum: An experiment in second-year nephrology. Methods Inf Med. 1992;31:303–309.
- Ho V, Kumar RK, Velan G. Online testable concept maps: Benefits for learning about the pathogenesis of disease. Med Educ. 2014;48:687–697.
- McLaughlin K, Mandin H. Using concept sorting to study learning processes and outcomes. Acad Med. 2002;77:831–836.
- Novak K, Mandin H, Wilcox E, McLaughlin K. Using a conceptual framework during learning attendees the loss of expert-type knowledge structure. BMC Med Educ. 2006;6.
- Schwartz MW, Rauch JS. A structured curriculum for an undergraduate elective clerkship in pediatric nephrology. J Med Educ. 1977;52:857–858.
- Schwab TR, Knox FG. Laboratory experience for understanding the physiological basis of diuretic therapy. Am J Physiol. 1991;260:S10–S13.
- Arger PH, Schultz SM, Sehgal CM, Cary TW, Aronchick J. Teaching medical students diagnostic sonography. J Ultrasound Med. 2005;24:1365–1369.
- Wimmers PF, Schmidt HG, Verkoeijen PPJL, Van De Wiel MWJ. Inducing expertise effects in clinical case recall. Med Educ 2005;39:949–957.
- McLaughlin K, Coderre S, Mortis G, Mandin H. Expert-type knowledge structure in medical students is associated with increased odds of diagnostic success. Teach Learn Med. 2007;19:35–41.
- Kiesewetter J, Ebersbach R, Görlitz A, Holzer M, Fischer MR, Schmidmaier R. Cognitive problem solving patterns of medical students correlate with success in diagnostic case solutions. PLoS One. 2013;8:e71486.
- Jhaveri KD, Perazella MA. Nephrologists as educators: Clarifying roles, seizing opportunities. Clin J Am Soc Nephrol. 2016;11(1):176–189.
- Cook DA. Randomized controlled trials and meta-analysis in medical education: What role do they play? Med Teach. 2012;34:468–473.
- Mesquita CT, Reis JC, Simões LS, et al. Digital stethoscope as an innovative tool on the teaching of auscultatory skills. Arq Bras Cardiol. 2013;100:187–189.
- Sverdrup Ø, Jensen T, Solheim S, et al. Training auscultatory skills: Computer simulated heart sounds or additional bedside training? A randomized trial on third-year medical students. BMC Med Educ. 2010;10:3.
- Høyte H, Jensen T, Gjesdal K. Cardiac auscultation training of medical students: a comparison of electronic sensor-based and acoustic stethoscopes. BMC Med Educ. 2005;5:14.
- Mahler SA, Wolcott CJ, Swoboda TK, et al. Techniques for teaching electrocardiogram interpretation: self-directed learning is less effective than a workshop or lecture. Med Educ. 2011;45:347–353.
- Rolskov Bojsen S, Räder SB, Holst AG, et al. The acquisition and retention of ECG interpretation skills after a standardized web-based ECG tutorial-a randomised study. BMC Med Educ. 2015;15:36.
- Blissett S, Cavalcanti R, Sibbald M. ECG rhythm analysis with expert and learner-generated schemas in novice learners. Adv Health Sci Educ Theory Pract. 2015;20:915–933.
- Russell PM, Mallin M, Youngquist ST, et al. First “glass” education: telementored cardiac ultrasonography using Google Glass- a pilot study. Acad Emerg Med. 2014;21:1297–1299.
- Griksaitis MJ, Sawdon MA, Finn GM. Ultrasound and cadaveric prosections as methods for teaching cardiac anatomy: A comparative study. Anat Sci Educ. 2012;5:20–26.
- Fodor D, Badea R, Poanta L, et al. The use of ultrasonography in learning clinical examination - a pilot study involving third year medical students. Med Ultrason. 2012;14:177–181.
- Hayes RB, Geller A, Churchill L, et al. Teaching tobacco dependence treatment and counseling skills during medical school: rationale and design of the Medical Students helping patients Quit tobacco (MSQuit) group randomized controlled trial. Contemp Clin Trials. 2014;37:284–293.
- Stolz D, Langewitz W, Meyer A, et al. Enhanced didactic methods of smoking cessation training for medical students-a randomized study. Nicotine Tob Res. 2012;14:224–228.
- Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–157.
- Hänsel M, Winkelmann AM, Hardt F, et al. Impact of simulator training and crew resource management training on final-year medical students' performance in sepsis resuscitation: a randomized trial. Minerva Anestesiol. 2012;78:901–909.
- Dominelli GS, Dominelli PB, Rathgeber SL, et al. Effect of different single-session educational modalities on improving medical students' ability to demonstrate proper pressurized metered dose inhaler technique. J Asthma. 2012;49:434–439.
- Perkins GD, Walker G, Christensen K, et al. Teaching recognition of agonal breathing improves accuracy of diagnosing cardiac arrest. Resuscitation. 2006;70:432–437.
- Beermann J, Tetzlaff R, Bruckner T, et al. Three-dimensional visualisation improves understanding of surgical liver anatomy. Med Educ. 2010;44:936–940.
- Müller-Stich BP, Löb N, Wald D, et al. Regular three-dimensional presentations improve in the identification of surgical liver anatomy - a randomized study. BMC Med Educ. 2013;13:131.
- Popadiuk C, Pottle M, Curran V. Teaching digital rectal examinations to medical students: An evaluation study of teaching methods. Acad Med. 2002;77:1140–1146.
- Butter J, Grant TH, Egan M, et al. Does ultrasound training boost Year 1 medical student competence and confidence when learning abdominal examination? Med Educ. 2007;41:843–848.
- Devitt P, Palmer E. Computer-aided learning: An overvalued educational resource? Med Educ. 1999;33:136–139.
- Peets AD, Coderre S, Wright B, et al. Involvement in teaching improves learning in medical students: a randomized cross-over study. BMC Med Educ. 2009;9:55.
- Association of American Medical Colleges. Medical Education Research Certificate (MERC) Program. Available at: https://www.aamc.org/members/gea/merc. Accessed March 18, 2016.
- Harvard Macy Institute. Available at: http://www.harvardmacy.org. Accessed March 18, 2016.
- Bernstein RA, McKegney FP, Weaver LA. The dialysis exercise: A clinical simulation for preclinical medical students. J Med Educ. 1980;55:958–960.
- Lio PA, Martin SA, Seifter JL. A medical team format for tutorial groups and cases. Acad Med. 2001;76:527–528.
- McLaughlin K, Coderre S, Woloschuk W, Lim T, Muruve D, Mandin H. The influence of objectives, learning experiences and examination blueprint on medical students' examination preparation. BMC Med Educ. 2005;5:39.
- Nambudiri VE, Newman LR, Haynes HA, Schur P, Vleugels RA. Creation of a novel, interdisciplinary, multisite clerkship: Understanding lupus. Acad Med. 2014;89:404–409.
- Bijol V, Byrne-Dugan CJ, Hoenig MP. Medical student web-based formative assessment tool for renal pathology. Med Educ Online. 2015;20:26765.
