Abstract
Purpose: Mortality is a major problem in renal transplant patients, and appropriate preoperative evaluation is very important. We retrospectively reviewed the left ventricle ejection fraction (LVEF) of renal transplant patients.
Material and methods: The clinical records of 1763 patients who had preoperative LVEF results and who underwent renal transplantation at Akdeniz University Faculty of Medicine during the years 2004–2014 were studied. The LVEF limit was set at 55%. LVEF, age, gender, diabetes mellitus, hypertension, type of dialysis were assessed by linear multiple regression analysis on survival.
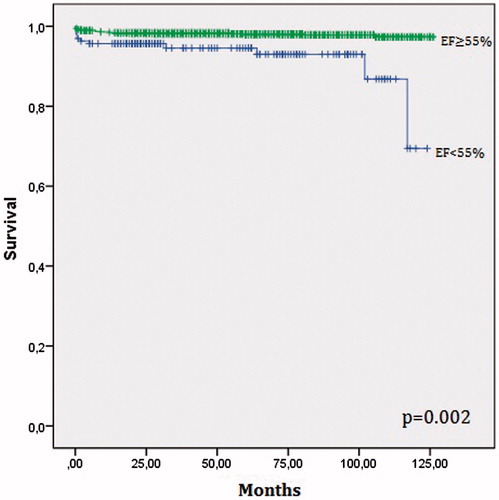
Results: There were a total of 1763 renal transplant patients. Those with LVEF of <55% were identified as having left ventricular dysfunction. The mean LVEF was 59.4 ± 9.1 in the 43 patients who died after renal transplantation, while it was 62.6 ± 7.4 in the survivors (p = 0.02). The mortality rate in the LVEF < 55% group was 6.8% (11/162 patients), while mortality in the LVEF ≥ 55% group was 2% (32/1601 patients, p < 0.001). LVEF was found to be the most powerful variable on survival by the linear multiple regression analysis, R2 = 0.05, p < 0.001.
Conclusion: LVEF may predict mortality in renal transplant patients. LVEF is known to be lower in patients with high cardiac mortality, who may require greater modifications of the postoperative risks.
Keywords:
Introduction
Transplantation is the standard of therapy for end-stage renal disease (ESRD) patients. Renal transplants are more cost-effectiveness than dialysis.Citation1 The most important challenge is improving long-term outcomes, and the selection of recipients and donors is critical. The preoperative evaluation of the recipient is very important, as it is donor suitability, because patient and organ losses cause societal and economic damage. Evaluation of the recipient patient, identification of high-risk patients, and modification of preoperative care is of vital importance. Cardiovascular mortality is a major problem in cardiac surgery, as well as in non-cardiac surgery; left ventricular systolic and diastolic dysfunction are the most common cardiovascular abnormalities, associated with increased morbidity and mortality in patients with ESRD.Citation2 Due to renal anemia, systemic hypertension, volume overload, and the presence of an arteriovenous fistula with high flow rate, the LV systolic and diastolic diameters, wall thickness, and cardiac output are increased and left ventricle ejection fraction (LVEF) is indirectly decreased.Citation3 LVEF is measured by echocardiography, which is an easy, highly reproducible, cheap, and noninvasive method. Therefore, appropriate arrangements for preoperative evaluation should be made to achieve the best clinical outcomes.
LVEF is a good predictor of cardiovascular mortality. The present study aims to investigate the relationship between postoperative mortality and LVEF in renal transplant patients.
Material and methods
Study population
Medical records regarding clinical transplantations were examined retrospectively at the Akdeniz University Faculty of Medicine. We analyzed the data of patients who underwent renal transplantation during the years 2004–2014, with regard to LVEF and post-transplant mortality. The records of 2009 renal transplant patients were analyzed, and 1763 of these patients with recorded EFs were enrolled the study; echocardiographic data and causes of death were examined in detail. The patients were divided into two groups depending on preoperative LVEF (<55% or ≥55%).
Statistical analysis
All analyses were conducted using SPSS version 19.0 for Windows (SPSS Inc., Chicago, IL). Quantitative variables were expressed as mean ± SD or median (minimum–maximum) and qualitative variables were expressed as percentages (%). All measurements were evaluated with the Kolmogorov–Smirnov test for normality. Comparison of parametric values between the two groups was performed with the Mann–Whitney U test or Student’s t-test. Categorical variables were compared by the likelihood-ratio χCitation2 test or Fisher’s exact test. p < 0.05 was considered statistically significant. The effect of the degree of LVEF on the survival of transplant patients was investigated using a log rank test. The Kaplan–Meier survival estimates were calculated. The associations between survival (dependent variable) and independent variables were analyzed using linear multivariable regression analysis Multivariate models were adjusted for age, gender, diabetes mellitus (DM), types of dialysis, hypertension, and LVEF. All variables were continuous. A 5% Type I error level was used to inter-statistical significance.
Results
We analyzed the data of patients who underwent renal transplantation between the years 2004 and 2014. LVEF and post-transplant mortality were analyzed using the data of 2009 patients, and 1763 patients with recorded LVEFs were enrolled the study. General characteristics of study population were showed . Pre-transplant renal replacement therapy was also evaluated (). The relationships between mortality and LVEF were evaluated statistically. First, the LVEF values of patients who died were compared to those of the survivors using the t-test, which showed that LVEF values were lower in the patients who died. The mean LVEF was 59.4 ± 9.1 in the 43 patients who died after renal transplantation, while it was 62.6 ± 7.4 in the survivors (p = 0.02). LVEF was categorized into two groups, above and below the level of 55%. An LVEF value of <55% was considered to be low, while an LVEF value of >55% was considered to be normal. In the analysis, LVEFs of <55% in 162 patients were detected. LVEFs were >55% in 1601 patients. The mortality rate in the LVEF <55% group was 6.8% (11/162 patients), while mortality in the LVEF ≥55% group was 2% (32/1601 patients, p < 0.001).
Table 1. General characteristics of study population.
Table 2. Types of dialysis before kidney transplantation.
Second, a survival analysis was also assessed with the Kaplan–Meier method, and the median survival time was 114.1 months in patients with LVEF of <55% and 123.5 months in patients with EF of ≥55% (p = 0.002, confidence interval 95%). Patients with low LVEF had significantly higher mortality. Moreover LVEF, age, gender, DM, hypertension, type of dialysis were assessed by linear multiple regression analysis on survival. Hemodialysis, diabetes mellitus and hypertension were found to be statistically insignificant effect on survival with stepwise model. LVEF was found to be the most powerful variable on survival by the linear multiple regression analysis. Age, peritoneal dialysis, and male gender were found to reduce survival ().
Table 3. Linear multivariable regression analysis of survival in renal transplant patients.
The exact cause of death could not be determined in some patients; therefore, all-cause mortality was used as a parameter. As a result, both methods revealed that as LVEF decreases, mortality increases.
Discussion
The primary finding of this study of a large population of ESRD patients was that preoperative LVEF was a strong predictor of survival during long-term follow-up after renal transplantation, so preoperative evaluation is important in non-cardiac surgeries such as renal transplantation. Knowing the risks and modifying them is crucial in order to achieve good clinical results in the perioperative stage. The most important problem in renal transplantation is loss of a recipient with a functional kidney. Cardiovascular diseases are quite common in ESRD patients, with vessel atherosclerosis and left ventricular hypertrophy having been shown in postmortem studies of ESRD patients.Citation4
Cardiovascular disorders are the leading cause of death after renal transplantation in the early and late phases. The main causes of death are infection and postoperative deterioration of preexisting cardiovascular disease in the early phase. The reasons for cardiovascular disease deaths include cardiac infarction, stroke, and therapy-refractory cardiac insufficiency, which are emphasized in the later phase after renal transplantation.Citation5 In the first-year post-renal transplantation, 40–50% of deaths are due to cardiovascular disease. The Patient Outcomes in Renal Transplantation (PORT) study, which included 23,000 patients, was analyzed retrospectively, and cardiovascular death was found to be 7% in the five-year period after renal transplantation.Citation4 In our study, the conventional cardiac risk factors, such as diabetes mellitus and hypertension, were present in approximately 25% of the patients (n = 440). Additionally, immunosuppressive therapy may also be an extra risk factor for cardiovascular disease. Calcineurin inhibitors and corticosteroids increase blood pressure, and in addition to corticosteroids, calcineurin inhibitors and mTOR (mammalian target of rapamycin) inhibitors are associated with dyslipidemia.Citation6,Citation7 Standard risk scores like Framingham Risk Score, underestimate cardiovascular risk even new factors such as uric acid and high-sensitivity C-reactive protein were added the in transplant recipients.Citation8–10 There is a need for predictors for long-term prognosis. Although there is evidence that LVEF is an indicator of the outcome of patients undergoing cardiac surgery,Citation11 the role of LVEF in non-cardiac surgery is less clear.Citation12 In addition, the definition of reduced LVEF is controversial. Although the traditionally accepted cutoff value in LV systolic dysfunction is an LVEF of <50%,Citation13 we compared the LVEFs of patients who died and those who survived and the LVEFs of the patients who died were 59% ± 9.1%. This value was significantly lower than in the surviving patients. Therefore, we used a threshold of 55%. Although groups are not homogenous group in terms of risk factors, LVEF was found to be the most powerful variable on survival by linear multiple regression analysis. In our study, a low LVEF was found to be associated with increased mortality. In addition, length of hospital stay was found significantly shorter in patients with higher LVEF. Our study is the first article describing the effect of LVEF after renal transplantation. To our knowledge, there are no clinical data yet about the cutoff value for LVEF in renal transplant candidates. We found that survival was reduced in patient with LVEF <55% after the renal transplantation ().
The use of cardioprotective therapy to improve the clinical results in ESRD patients has been demonstratedCitation14 and the decreasing death rates from cardiovascular disease have been shown to be due to primary and secondary preventions, increased cardiovascular screening, and interventions according to the registry data.Citation15–17
Study limitations
This study has several limitations. It was a retrospective review of data, and its accuracy depended on the availability of information within the medical records. This was not a randomized trial, we can only speculate on the ideal cutoff for referring patients for renal transplantation. Information on the cause of death was not available in some patients, therefore all-cause mortality was used as a parameter than cause-specific death.
Conclusion
In ESRD patients undergoing renal transplantation, LVEF provides important prognostic information beyond the standard risk factors, and LVEF may predict mortality. Patients with low LVEF have higher cardiac mortality and may require more modifications of the periprocedural risks. Strategies to minimize the risk of post-transplant death should include continuous support of renal transplant recipients in terms of early and subsequent cardiovascular training. There is a need for predictors of mortality in renal transplant patients. Clarification and verification of cardiovascular disease predictors with prospective studies will be useful for clinicians in the future.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hagenmeyer EG, Haussler B, Hempel E, et al. Resource use and treatment costs after kidney transplantation: Impact of demographic factors, comorbidities, and complications. Transplantation. 2004;77:1545–1549.
- Hsiao SH, Huang WC, Sy CL, Lin SK, Lee TY, Liu CP. Doppler tissue imaging and color M-mode flow propagation velocity: Are they really preload independent? J Am Soc Echocardiogr. 2005;18:1277–1284.
- Arjona Barrionuevo JD, Gonzáles Vargas-Machuca MF, Gómez Pulido F, Gil Sacaluga L, Gentil Govantes MA, Martínez-Martínez A. Transthoracic echocardiographic findings in patients with chronic kidney disease awaiting kidney transplantation. Transplant Proc. 2010;42:3123–3125.
- Israni AK, Snyder JJ, Skeans MA, Peng Y, et al. Predicting coronary heart disease after kidney transplantation: Patient Outcomes in Renal Transplantation (PORT) study. Am J Transplant. 2010;10:338–353.
- Qiu J, Cai J, Terasaki PL. Death with a functioning graft in kidney transplant recipients. Clin Transpl. 2004;18:379–386.
- Weiner DE, Carpenter MA, Levey AS, et al. Kidney function and risk of cardiovascular disease and mortality in kidney transplant recipients: The FAVORIT trial. Am J Transplant. 2012;12:2437–2445.
- Svensson M, Jardine A, Fellstrom B, Holdaas H. Prevention of cardiovascular disease after renal transplantation. Curr Opin Organ Transplant. 2012;17:393–400.
- Soveri I, Holme I, Holdaas H, Budde K, Jardine AG, Fellström B. A cardiovascular risk calculator for renal transplant recipients. Transplantation. 2012;94:57–62.
- Silver SA, Huang M, Nash MM, Prasad GV. Framingham risk score and novel cardiovascular risk factors underpredict major adverse cardiac events in kidney transplant recipients. Transplantation. 2011;92:183–189.
- Pita-Fernandez S, Pertega-Diaz S, Valdes-Canedo F, et al. Incidence of cardiovascular events after kidney transplantation and cardiovascular risk scores: Study protocol. BMC Cardiovasc Disord. 2011;11:2.
- Kennedy JW, Kaiser GC, Fisher LD, et al. Clinical and angiographic predictors of operative mortality from the collaborative study in coronary artery surgery (CASS). Circulation. 1981;63:793–802.
- Dahl JS, Eleid MF, Michelena HI, et al. Effect of left ventricular ejection fraction on postoperative outcome in patients with severe aortic stenosis undergoing aortic valve replacement. Circ Cardiovasc Imaging. 2015;8:2917–2926.
- Lang RM, Bierig M, Devereux RB, et al. Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463.
- Pilmore HL, Skeans MA, Snyder JJ, Israni AK, Kasiske BL. Cardiovascular disease medications after renal transplantation: Results from the patient outcomes in renal transplantation study. Transplantation. 2011;91:542–551.
- Pilmore H, Dent H, Chang S, McDonald SP, Chadban SJ. Reduction in cardiovascular death after kidney transplantation. Transplantation. 2010;89:851–857.
- Lentine KL, Villines TC, Xiao H, et al. Cardioprotective medication use after acute myocardial infarction in kidney transplant recipients. Transplantation. 2011;91:1120–1126.
- Cross NB, Webster AC, Masson P, O’Connell PJ, Craig JC. Antihypertensives for kidney transplant recipients: Systematic review and meta-analysis of randomized controlled trials. Transplantation. 2009;88:7–18.