Abstract
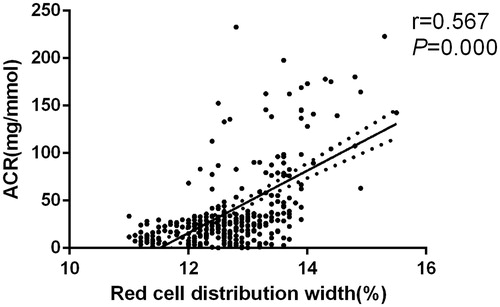
Previous studies found that red cell distribution width was related to adverse cardiovascular events. However, few studies reported the relationship between red cell distribution width and early-stage renal injury in pregnant women with gestational diabetes mellitus. Using a cross-sectional design, 334 pregnant women with gestational diabetes mellitus were enrolled according to the criterion of inclusion and exclusion. Demographic and clinical examination data were collected. Depended on the urine albumin, study population were divided into case group (n = 118) and control group (n = 216). Compared with control group, the case group tend to be higher red cell distribution width level (13.6 ± 0.9 vs.12.5 ± 0.6, p < 0.001). The red cell distribution width was positively associated with albuminuria creatinine ratio (r = 0.567, p < 0.001). Multiple logistic regressions showed that red cell distribution width was still associated with early-stage renal injury after adjusting for many other potential cofounders. Compared with the first quartile, the risk ratio of the second, the third and the fourth quartile were 1.38 (95%CI: 1.06–1.80), 1.57 (95%CI: 1.21–2.97), 2.71 (95%CI: 2.08–3.54), respectively. Besides, systolic blood pressure, estimated glomerular filtration rate, uric acid and blood urea nitrogen were also significantly associated with renal injury in gestational diabetes mellitus patients. The elevated red cell distribution width level might be a predictor of early-stage renal injury in pregnant women with gestational diabetes mellitus. As an easy and routine examination index, red cell distribution width may provide better clinical guidance when combined with other important indices.
Introduction
Gestational diabetes mellitus (GDM) is a condition in which women without previously diagnosed diabetes exhibit high blood glucose, especially during their third trimester.Citation1 The frequency of GDM is rising globally and may also increase further as less-stringent criteria for the diagnosis are potentially adopted.Citation2 Women with uncontrolled GDM are at increased risk of developing type 2 diabetes mellitus after pregnancy, as well as having a higher incidence of pre-eclampsia and Cesarean section.Citation3,Citation4 In addition to these, the vascular diseases and related target-organ injury caused by GDM also cannot be ignored.Citation5–7 The renal injury is one of common complications of GDM. This could further elevate the risk of adverse pregnancy outcomes, and also causes the cardiovascular disease events for pregnancy women in the long-term future.Citation8,Citation9 It was reported that 30–40% of diabetic nephropathy patients eventually developed into end-stage renal disease.Citation10 If the effective treatment was given in early diabetic nephropathy, significant improvement of clinical symptoms and prognosis could be achieved. Therefore, the early diagnosis of renal injury in GDM patients would be particularly important.
Red cell distribution width (RDW), an index of the routine blood cell count, is not only used to evaluate different types of anemia but also is a potential predictor of morbidity and mortality in a variety of settings, especially for many cardiovascular diseases.Citation11 Recent studies found that RDW was related to the mortality of cardiovascular diseases in the whole population.Citation12,Citation13 Indeed, the level of elevated RDW hinted that red blood cell could be uneven in shape, which was associated with degradation and impairment of erythropoiesis, and the change of erythropoiesis was a sign of over-activity of oxidative stress and increased inflammation reaction.Citation14 Both of the conditions were adverse signs in GDM.Citation15 Li et al.Citation16 found that RDW level was associated with early renal injury in hypertensive patients, which was the first study about relationship between RDW and renal injury. The patients with renal injury tend to be higher RDW level. Consistent with this study, Majri et al.Citation17 also found that RDW was associated with diabetes-associated complications including diabetic nephropathy. It should be noted that people in this study had been diagnosed with diabetes nephropathy. It is known that inflammatory cytokines, such as interleukin (IL)-1, IL-6, tumor necrosis factor (TNF)-α, desensitize bone marrow erythroid progenitors to erythropoiesis, inhibiting red blood cell maturation and thereby promote aniysocytosis.Citation18 Elevated RDW may be from an underlying inflammatory reaction. Hyperglycemia is closely associated with vascular endothelial injury caused by inflammatory, which is one of the main reasons leading to renal injury. It is possible that there is a relationship between RDW and renal function. Obviously, early identification was rather important for diabetes mellitus, especially for pregnant women. The present study is to evaluate the relationship between RDW and early renal injury in patients with GDM.
Materials and methods
Study population
Study population were pregnant women from Department of Obstetrics in our hospital during March 2013 to June 2015. Using a cross-sectional design, a total of 334 patients with GDM were enrolled according to inclusion and exclusion criterion.
All subjects received glucose screening test during 14–27 weeks and 28–36 weeks, and oral glucose tolerance test (OGTT) was conducted for abnormal glucose level. The criteria for inclusion: aged from 23 to 38 years old, first pregnant, no history of smoking and alcohol, no family history of diabetes mellitus, conform to the diagnostic criteria of GDM. The criteria for exclusion: pre-gestational diabetes, family history of diabetes, preeclampsia, eclampsia, pregnancy-induced hypertension, history of hypertension before pregnancy, severe liver and kidney diseases or chronic kidney disease, multiple pregnancies, receiving drug treatment, myeloproliferative disorders, malignant neoplasms, and acute or chronic infection and chronic inflammatory disease. This study was approved by the Second Affiliated Hospital of Zhengzhou University Institutional Review Boards.
Diagnostic criteria
We screened GDM in accordance with diagnosis and treatment of GDM (2014) established by the Obstetrics and Gynecology Group of Chinese Medical Association and Association of Diabetic Pregnancy Study Group of Perinatal Medicine of Chinese Medical Association:Citation19 Fast plasma glucose (FPG) ≥ 7.0 mmol/L for pre-GDM; for GDM, 75 g OGTT was conducted. Three values were obtained: before OGTT, 1 and 2 h after OGTT with cutoff values of 5.1, 10.0 and 8.5, respectively. Those with one or more values equal to or more than the cutoff value were diagnosed with GDM. The early renal injury of GDM patients was defined as albuminuria to creatinine ratio (ACR) fallen into the range between 30 μg/mg and 300 μg.Citation20
Data collection
Data collection included demographic and clinical examination data. The demographic data included age, history of smoking and alcohol, history of all kinds of diseases, and family history of diseases. The clinical examination data mainly included physical index [height and weight for calculating body mass index (BMI); waist and hip circumstance for waist to hip ratio (WHR); systolic blood pressure (SBP); diastolic blood pressure (DBP)] and biochemical indices. Specifically, 5 ml blood samples were collected in the morning. The Hitachi (7020, Japan) Hematology Analyzer was used to conduct hematologic testing including red blood cell count, white blood cell count, hemoglobin, RDW, mean platelet volume (MVP), platelet and erythrocyte sedimentation rate (ESR). Hemoglobin A1c (HA1c) was used for an index. High-sensitivity C-reactive protein (Hs-CRP) was taken as a marker of inflammation. Besides, FPG, 2 h glucose level and serum lipid level [total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein (HDL-C)] were also collected. We used the Roche/Hitachi Modular System (Roche Diagnostics GmbH, Mannheim, Germany) to measure creatinine and blood urea nitrogen (BUN) level. Estimated glomerular filtration rate (eGFR) was according to the following formula: 186 × SCr−1.154×age in years−0.203 ×0.742.Citation21 Urine albumin was examined through the method of immunoturbidimetric (DPC, USA). Three early-morning urine samples were collected in order to measure albuminuria.
Statistical analysis
Study population were divided into early-stage renal injury and control groups according to ACR. Depending on the normal distribution of the Kolmogorow–Smirnow test, continuous data were expressed as mean ± standard deviation or median with range. For continuous data, Student’s t-test was used to measure the difference between two groups. Pearson or Spearman correlation coefficient was calculated to assess the relationship between RDW and other covariates. A multiple logistic regression model was built to evaluate the predictors of early-stage renal injury in patients with GDM, adjusting the following covariates: age, gestational week, BMI, WHR, SBP, DBP, triglyceride, HDL-C, LDL-C and FBP; Two hours of FPG, HbA1c, alanine aminotransferase (ALT), aspartate amino transferase (AST), serum creatinine, uric acid, BUN, Hs-CRP and blood routine index. RDW was divided into four categories according to the quartile (25, 50 and 75%). Collinearity diagnostics within variables was applied before regression model was built. Eigenvalue and condition index are used to decide whether multi-collinearity exits or not. If eigenvalue is close to zero or condition index is >30, it will mean that multi-collinearity exists. We used the Statistical Product and Service Solutions software (19.0 SPSS Inc., Chicago, IL) to conduct the whole analysis. p sp;< 0.05 was treated as the statistical significant standard.
Ethics statement
The study protocol was approved by the institutional review board of Zhengzhou University (IRB No. 0371–20150229-0023). Informed consent was waived by the IRB.
Results
General characteristics of study population
Initially, 387 pregnant women with GDM were ready for screening. Fifty-three women were excluded according to the criteria for inclusion and exclusion. Finally, 334 women with GDM were included for statistical analysis in the study. The early-stage renal injury included 118 women and control had 216 ones. To summarize, the age of all subjects was from 23 to 38 years old. The baseline data shown that no significant differences were observed in age (p = 0.065), gestational week (p = 0.176), BMI (p = 0.223) and waist–hip ratio (p = 0.500). Compared with patients without early renal injury, those without renal injury tend to be higher SBP (115.4 ± 16.4 vs. 106.7 ± 14.2, p < 0.001), DBP (78.3 ± 10.5 vs. 74.8 ± 9.6, p = 0.002), total cholesterol (4.6 ± 1.0 vs. 4.4 ± 1.0, p = 0.041), FPG (10.5 ± 3.3 vs. 9.6 ± 3.5, p = 0.011) and 2 h PG (19.9 ± 5.5 vs. 18.2 ± 6.2, p = 0.006). The uric acid (266.4 ± 93.5 vs. 239.9 ± 113.2, p = 0.015) and BUN levels (6.6 ± 1.9 vs. 5.7 ± 1.5, p < 0.001) for case group were higher than control while the eGFR level was lower compared with control (73.9 ± 35.5 vs. 96.5 ± 21.3, p < 0.001). The elevated RDW (13.6 ± 0.9 vs.12.5 ± 0.6, p < 0.001) and Hs-CRP [2.1 (1.0–5.0) vs. 2.0 (1.3–3.7), p = 0.023] were also objected. Besides, the reduced platelets, red blood cell and hemoglobin levels were proved between two groups. However, there were no significances about MPV and white blood cell. All results were shown in .
Table 1. Comparisons of clinical data between case group and control group.
Univariate analysis of RDW and other covariates
For the whole study population, a positive relationship between RDW and ACR was found (r = 0.567, p < 0.001, ), and Hs-CRP also shown a positive correlation with RDW (r = 0.206, p = 0.018). In addition to SBP (p = 0.016), triglyceride (p = 0.032), FPG (p = 0.004), creatinine (p < 0.001), uric acid (p = 0.015) and BUN (p = 0.005), eGFR (p = 0.020) also show positive correlation with RDW. The relationship between RDW and BMI was weak. The rest shown no obvious significant (p > 0.05). The results were shown .
Table 2. Correlation analysis between RDW and other variables in patients with GDM.
Multiple logistic regression analysis for early-stage renal injury
To explore the potential predictors of early-stage renal injury in patients with GDM, a stepwise multiple logistic regression analysis was conducted. The ACR was treated as the dependent variable, and the quartile of RDW and other factors were considered as covariates. The logistic regression results shown that RDW was one of the potential predictors for early-stage renal injury among GDM patients. Compared with the first quartile, the risk ratio of the second, the third and the fourth quartile were 1.38 (95%CI: 1.06–1.80), 1.57(95%CI: 1.21–2.97), 2.71(95%CI: 2.08–3.54), respectively. Besides, SBP (OR =1.98, 95%CI: 1.51–2.59), eGFR (OR = 2.13, 95%CI: 1.31–3.46), uric acid (OR = 1.33, 95%CI: 1.15–2.22) and BUN (OR =1.43, 95%CI: 1.05–1.96) were also significantly associated with renal injury in GDM patients. The specific results were presented in .
Table 3. Independent predictors of development of early renal injury in patients with GDM.
Discussion
The present study found that there was a positive correlation between high RDW level and high ACR in pregnant women with GDM. RDW could be a potential predictor of early-stage renal injury in patients with GDM. The risk ratio increased with the RDW quartile compared with the first quartile after adjusting for lots of potential cofounders. Previous study suggested that RDW was associated with diabetic nephropathy in patients with type 2 diabetic.Citation17 The multiple logistic regressions shown the risk ratio of RDW was 1.64 with 1.15–2.35 of 95%CI. It should be noted that there are several different points needed to be addressed. First, the population setting is different. Our study was set in pregnant women with GDM while the latter included type 2 diabetic. Second, the outcome index is different. Our aim is exploring the relationship between RDW and early-stage renal injury while the patients included in the latter study had been diagnosed with diabetic nephropathy. Finally, the present study included larger sample sizes than previous study. Li et al.Citation16 found that RDW level was related to early renal injury in patients with hypertension, which was the first study about relationship between RDW and early-stage renal injury. The present study further confirmed and extended these findings and provided stronger support about the role of RDW in target-organ injury of diabetes mellitus.
The possible reason of relationship between RDW and early-stage renal injury could be that elevated RDW level reflected the change of renal hemodynamics. It was suggested that renal injury in patients with diabetic was related to fragmentation of red blood cell, which induced the increase of RDW.Citation22,Citation23 The elevation of blood pressure caused by the increased sheer wall tension of intraglomerular mesangial cell was involved in the process of renal injury in patients with diabetic.Citation24,Citation25 The wall tension changed the red blood cell fragmentation, resulting in the increased RDW level. Moreover, the long-term hyperglycemia situation will lead to the loss of red blood cell deformability and this situation will get worse in diabetic with renal damage.Citation26,Citation27 The loss of deformability further increased erythrocyte fragility. This probably occurred to pregnant women with GDM. Besides, the increased erythrocyte fragility could also impair the microcirculation, lead to tissue hypoxia and formation of thrombosis, which were considered to play an important in the development of renal injury of diabetic. The other possible explanation was inflammation. It was found that there was a graded association between RDW and hs-CRP, which was in consistent with the present results.Citation28 In addition to hs-CRP, some other inflammation factors such as IL-6 level had been related to RDW level.Citation29 It was known that inflammation response was thought to play an important role in the pathogenesis of renal injury of diabetic.Citation30 Over expression of IL-6 happened in patients with diabetic, and this volume of IL-6 became more obvious in patients with albuminuria than those with micro albuminuria.Citation31 This partly explained that RDW could be a predictor of early-stage renal injury in pregnant with GDM. Another reason could be oxidative stress. Because the serum selenium could predict the RDW level in a study with women aged >65 years old.Citation29 However, the fact that Magri et al. had not found that RDW was associated with retinopathy made this less possible because oxidative stress had been thought to be involved in the process of retinopathy in diabetic.Citation17
There are still several limitations. First, this study is a cross-sectional design. We couldn’t confirm the cause-and-effect relationship between RDW and early-stage renal injury in pregnant women with GDM. There may be some bias such as survival bias. However, after a review of publications about RDW and others adverse outcomes, this kind of bias may have underestimated the association. Second, the results of our study was from pregnant women with GDM. It should be cautious when adjusted this finding to other people setting. But in view of the findings, the present study results didn’t have much overlap in relative to other studies. On the contrary, our results extend the recognition of the relationship between RDW and some outcomes. Third, we didn’t affirm the long-term effect of RDW. Therefore, a well-designed cohort study is still needed to verify these findings.
In conclusion, the elevated RDW level may be a predictor of early-stage renal injury in pregnant women with GDM after adjusting to some potential cofounders. As an easy and convenient routine examination, RDW may provide better clinical guidance along with other important indices.
Acknowledgments
We thank all our colleagues working in the Second Affiliated Hospital of Zhengzhou University.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Kerner W, Bruckel J, German Diabetes A. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabet. 2014;122:384–386.
- Jiwani A, Marseille E, Lohse N, et al. Gestational diabetes mellitus: Results from a survey of country prevalence and practices. J Matern Fetal Neonatal Med. 2012;25:600–610.
- Anderberg E, Kallen K, Berntorp K. The impact of gestational diabetes mellitus on pregnancy outcome comparing different cut-off criteria for abnormal glucose tolerance. Acta Obstet Gynecol Scand. 2010;89:1532–1537.
- Dalfra MG, Ragazzi E, Masin M, et al. Pregnancy outcome in immigrant women with gestational diabetes mellitus. Gynecol Endocrinol. 2011;27:379–383.
- Yogev Y, Xenakis EM, Langer O. The association between preeclampsia and the severity of gestational diabetes: The impact of glycemic control. Am J Obstet Gynecol. 2004;191:1655–1660.
- Savyon M. The risk of overt diabetes mellitus among women with gestational diabetes: A population-based study. Diabet Med. 2010;27:852.
- Leiva A, Pardo F, Ramirez MA, et al. Fetoplacental vascular endothelial dysfunction as an early phenomenon in the programming of human adult diseases in subjects born from gestational diabetes mellitus or obesity in pregnancy. Exp Diabetes Res. 2011;2011:349286.
- Bayraktar F, Akinci B, Celtik A, et al. Insulin need in gestational diabetes is associated with a worse cardiovascular risk profile after pregnancy. Intern Med. 2012;51:839–843.
- Sullivan SD, Umans JG, Ratner R. Gestational diabetes: Implications for cardiovascular health. Curr Diab Rep. 2012;12:43–52.
- Adler AI, Stevens RJ, Manley SE, et al. Development and progression of nephropathy in type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63:225–232.
- Lin CK, Huang MJ, Hsu HC. The role of red blood cell distribution width in the differential diagnosis of microcytic anemia. Gaoxiong Yi Xue Ke Xue Za Zhi. 1988;4:491–494.
- Perlstein TS, Weuve J Pfeffer MA, et al. Red blood cell distribution width and mortality risk in a community-based prospective cohort. Arch Intern Med. 2009;169:588–594.
- Patel KV, Ferrucci L Ershler WB, et al. Red blood cell distribution width and the risk of death in middle-aged and older adults. Arch Intern Med. 2009;169:515–523.
- Wiwanitkit V. Plateletcrit, mean platelet volume, platelet distribution width: Its expected values and correlation with parallel red blood cell parameters. Clin Appl Thromb Hemost. 2004;10:175–178.
- King GL, Loeken MR. Hyperglycemia-induced oxidative stress in diabetic complications. Histochem Cell Biol. 2004;122:333–338.
- Li ZZ, Chen L, Yuan H, et al. Relationship between red blood cell distribution width and early-stage renal function damage in patients with essential hypertension. J Hypertens. 2014;32:2450–2455.
- Zhang M, Zhang Y, Li C, et al. Association between red blood cell distribution and renal function in patients with untreated type 2 diabetes mellitus. Ren Fail. 2015;37:659–663.
- Macdougall IC, Cooper A. The inflammatory response and erythropoiesis sensitivity. Nephrol Dial Transplant. 2002;17:48–52.
- Obstetrics and Gynecology Group of Chinese Medical Association. Diagnosis and treatment of gestational diabetes mellitus. Chin J Obstet Gynecol. 2014;49:561–569.
- Assadi FK. Quantitation of microalbuminuria using random urine samples. Pediatr Nephrol. 2002;17:107–110.
- Kidney Disease Outcomes Quality Initiative (K/DOQI) Group. K/DOQI clinical practice guidelines for management of dyslipidemias in patients with kidney disease. Am J Kidney Dis. 2003;41(Suppl. 3):i–iv, S1–S91.
- Paueksakon P, Revelo MP, Ma LJ, et al. Microangiopathic injury and augmented PAI-1 in human diabetic nephropathy. Kidney Int. 2002;61:2142–2148.
- Banno S, Ito Y, Tanaka C, et al. Quantification of red blood cell fragmentation by the automated hematology analyzer XE-2100 in patients with living donor liver transplantation. Clin Lab Haematol. 2005;27:292–196.
- Lewko B, Stepinski J. Hyperglycemia and mechanical stress: Targeting the renal podocyte. J Cell Physiol. 2009;221:288–295.
- Gnudi L, Thomas SM, Viberti G. Mechanical forces in diabetic kidney disease: A trigger for impaired glucose metabolism. J Am Soc Nephrol. 2007;18:2226–2232.
- Sutera SP, Mehrjardi MH. Deformation and fragmentation of human red blood cells in turbulent shear flow. Biophys J. 1975;15:1–10.
- Shin S, Ku YH, Ho JX, et al. Progressive impairment of erythrocyte deformability as indicator of microangiopathy in type 2 diabetes mellitus. Clin Hemorheol Microcirc. 2007;36:253–261.
- Lee WS, Kim TY. Relation between red blood cell distribution width and inflammatory biomarkers in rheumatoid arthritis. Arch Pathol Lab Med. 2010;134:505–506.
- Semba RD, Patel KV, Ferrucci L, et al. Serum antioxidants and inflammation predict red cell distribution width in older women: The Women’s Health and Aging Study I. Clin Nutr. 2010;29:600–604.
- Navarro JF, Milena FJ, et al. Renal pro-inflammatory cytokine gene expression in diabetic nephropathy: Effect of angiotensin-converting enzyme inhibition and pentoxifylline administration. Am J Nephrol. 2006;26:562–570.
- Aso Y, Yoshida N, Okumura K, et al. Coagulation and inflammation in overt diabetic nephropathy: association with hyperhomocysteinemia. Clin Chim Acta. 2004;348:139–145.