Abstract
Background: The target blood pressure in older patients is controversial. Recent studies provided clinical evidence supporting a target systolic blood pressure <120 mmHg in patients >50 years at high risk of cardiovascular events.
Methods: Retrospective study of 380 consecutive patients ≥60 years with stages 1–5 pre-dialysis chronic kidney disease seen between January 2013 and November 2015. The outcomes of a systolic blood pressure <120 mmHg in older patients with chronic kidney disease and multiple comorbidities were analyzed.
Results: Sixty-eight patients had a systolic blood pressure <120 mmHg, 312 patients had a systolic blood pressure ≥120 mmHg. Forty-three patients died during the follow up (11.3%). Patients with a systolic blood pressure <120 mmHg had a higher risk of death: 21 (30.9%) vs 22 (7%).
Primary cause of death: Cardiovascular: 11 (25.6%), infectious 9 (20.9%), cancer 5 (11.6%), renal failure 6 (13.9%), COPD/pulmonary fibrosis 2 (4.6%), end stage liver disease 3 (6.9%), traumatic brain injury 1 (2.3%), gastrointestinal hemorrhage 4 (9.3%), complications of diabetes 1 (2.3%), unknown 1 (2.3%). After adjusting for confounding factors, a systolic blood pressure <120 mmHg remained associated with increased mortality. There was a trend to more cardiovascular outcomes in those with a lower blood pressure.
Conclusions: A systolic blood pressure below 120 mmHg in older patients with high disease burden was associated with adverse outcomes. Individualization of blood pressure therapy to each specific patient is warranted.
Introduction
Chronic kidney disease (CKD) is very prevalent in the older population. It is believed that one in every two adults with CKD is older than 70 years.Citation1
The Eighth Joint National Committee (JNC-8) recommends to start treating blood pressure values ≥150/90 mmHg in patients older than 60 years. The target for patients younger than 60 and/or with CKD is 140/90 mmHg or below.Citation2
The JNC-8 guidelines were criticized for what was perceived as relaxation of the blood pressure targets. On the other hand, in the guidelines provided by the American Society of Hypertension and the International Society of Hypertension the treatment threshold of ≥150/90 mmHg only applies to patients 80 years or older.Citation3
Recently, the SPRINT trial added significant evidence supporting a more aggressive systolic blood pressure target (below 120 mmHg) in patients older than 50 years at high risk of cardiovascular events but without diabetes. Targeting a systolic blood pressure lower than 120 mm Hg, as compared with less than 140 mm Hg, resulted in lower rates of heart failure events, cardiovascular deaths and total deaths.Citation4
Before widespread application of the SPRINT trial results, careful identification of the type of patients that could benefit from this strategy is warranted.
The objective of this study was to assess the outcomes of a systolic blood pressure <120 mmHg in older patients with CKD and multiple comorbidities.
Methods
After obtaining approval from the Rice Memorial Hospital Institutional Review Board (Willmar, MN), a retrospective cohort study of 380 consecutive clinic patients older than 60 years with stages 1–5 pre-dialysis CKD was carried out. These patients were seen between January 2013 and November 2015.
Blood pressure targets: it was a standard practice during the follow-up years to keep the blood pressure below 130/80 mmHg in most patients with an ideal blood pressure defined as 120/80 mmHg or below.Citation5
CKD was defined as evidence of structural or functional kidney abnormalities (abnormal urinalysis, imaging studies, or histology) that persisted for at least 3 months, with or without a decreased glomerular filtration rate, as defined by a GFR of less than 60 mL/min per 1.73 m2.
Exclusion criteria: patients on renal replacement therapy, history of organ transplant, patients younger than 60 years.
Variables collected: Demographic, clinical, and laboratory data at baseline and during follow up.
Primary outcome: all-cause mortality. The cause of death was obtained from the medical records or death certificates.
Secondary outcomes: CKD stage 5 and/or end stage renal disease requiring dialysis; changes in GFR; new cardiovascular events.
Cardiovascular events: composite of new episodes of acute coronary event, angioplasty, decompensated heart failure, cerebrovascular accident (stroke, transient ischemic attack), atrial fibrillation, vascular surgery including carotid endarterectomy during the follow-up period.
Estimation of blood pressure: Office systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured with an automated device, using an adult cuff, with the patient in a seated position. Pulse pressure was determined by subtracting the DBP from the SBP. In the calculation of the mean blood pressure, we used blood pressures collected during regular visits to maintain consistency among all participants. A mean of 21 ± 13.6 blood pressure readings were obtained for each patient. Severe hypotension was defined as an SBP ≤90 mmHg.
Estimation of glomerular filtration rate (GFR): GFR was estimated by the four-variable Modification of Diet in Renal Disease formula (MDRD).Citation6
Estimation of proteinuria: Random urine albumin (albumin-to-creatinine ratio, expressed as mg/g) or total protein (protein-to-creatinine ratio, expressed as mg/g) were obtained after reviewing the medical records.
Statistical analyses: Data are presented as mean and standard deviation if normally distributed and median [25% and 75% percentiles] or range if not. For parametric data, differences in the mean were compared by the Student’s t-test. For highly skewed data, the Wilcoxon–Mann–Whitney test was used.
Differences in proportions were assessed by the Chi square or Fisher’s exact test.
Survival curves were generated using the Kaplan–Meier method. Cox proportional hazards models were used to study associations and adjust for confounding factors.
p Values ≤.05 were considered as statistically significant. All the analyses were performed using JMP statistical software version 11.2.0 (SAS Campus Drive, Cary, NC).
Results
Baseline characteristics ( and ): A total of 380 patients were analyzed.
Table 1. Baseline patient characteristics, N = 380.
Table 2. Baseline characteristics of patients with SBP lower and higher than 120 mmHg.
Patients with SBP < 120 mmHg had more congestive heart failure (CHF), atrial fibrillation, coronary artery disease, lower ejection fraction, and lower hemoglobin level. These factors were added in Cox Proportional Hazard Models.
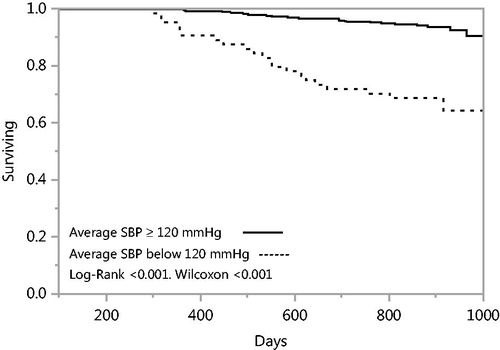
Clinical outcomes: Forty-three patients died during the follow up (11.3%). Patients with a SBP <120 mmHg had a significant higher risk of death ( and ; ).
Table 3. Primary and secondary outcomes.
Table 4. Cox proportional hazards models for mortality.
Primary cause of death: cardiovascular: 11 (25.6%), infectious: 9 (20.9%), cancer: 5 (11.6%), renal failure: 6 (13.9%), chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis: 2 (4.6%), end stage liver disease (ESLD): 3 (6.9%), traumatic brain injury: 1 (2.3%), gastrointestinal hemorrhage: 4 (9.3%), complications of diabetes: 1 (2.3%), unknown: 1 (2.3%).
Cardiovascular causes of death included fatal arrhythmias, CHF exacerbation, cardiogenic shock, and cardiac ischemia. These were more common in patients in the lower SBP group (six patients vs five patients in the group with higher SBP).
Minor differences were noted in the degree of renal function deterioration, with slightly worse outcomes in patients with lower SBP. Twenty-six patients progressed to CKD 5 or ESRD (6.8%) ().
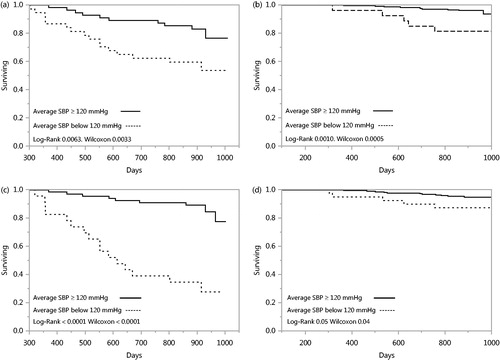
Worse outcomes were seen with a SBP < 120 mmHg in patients with and without CHF and cardiovascular events (). After adjusting for confounding factors, a SBP < 120 mmHg remained associated with increased mortality ().
Figure 2. (a) Systolic blood pressure below 120 mmHg and survival in patients with CHF. (b) Systolic blood pressure below 120 mmHg and survival in patients without CHF. (c) Systolic blood pressure below 120 mmHg and survival in patients with new cardiovascular events during the follow up period. (d) Systolic blood pressure below 120 mmHg and survival in patients without cardiovascular events during the follow-up period.
Episodes of severe hypotension (SBP< 90 mmHg) were more common in those with SBP < 120 mmHg: 23 patients (33.8%) vs 20 (6.4%) in the higher SBP group (p < .0001). Thirty percent of patients with one or more episodes of severe hypotension died vs 8.9% of those with no episodes of severe hypotension (p = .0003, not shown).
Ninety-five patients (25.9%) had new cardiovascular events during the follow-up period. In univariate analysis, an SBP lower than 120 mmHg was associated with increased hazard for cardiovascular events (). In a multivariate model (after adjusting for CHF, CAD, and PVD) this association was not statistically significant. The main predictor of new cardiovascular events was the presence of established cardiovascular disease ().
Table 5. Cox proportional model for new cardiovascular events.
Discussion
In this study, the effect of a SBP <120 mmHg was analyzed. Although this was an observational study, the follow up was extensive, given the unique geographical characteristics of this population. Most patients get their care in one of two local clinics and are admitted to one or two hospitals, which share electronic medical records. This allows for follow up of outcomes of interest.
The pattern of practice during the follow-up period and before was to achieve a target blood pressure of 130/80 mmHg in most patients, with an ideal blood pressure of 120/80 mmHg or below.Citation5
A significant number of office blood pressure readings were obtained and analyzed in each patient. This might be a strength, but also a limitation since ambulatory blood pressure measurements are better associated with cardiovascular outcomes than office blood pressures.Citation7
The target blood pressure in older patients is a subject of controversy. In the older population, a landmark study was HYVET. This study focused on people older than 80 years and showed benefits in treating hypertension in this population. However, the baseline blood pressure was in the 170s/90s mmHg and the blood pressure after intervention was <150/80 mm Hg. Comparing to placebo, active treatment was associated with a 30% reduction in the rate of fatal or nonfatal stroke, a 39% reduction in the rate of death from stroke, a 21% reduction in the rate of death from any cause, a 23% reduction in the rate of death from cardiovascular causes and a 64% reduction in the rate of heart failure.Citation8
In the SPRINT trial, the mean age of the study population was 67 years. Approximately, 15% of the patients had a clinical diagnosis of cardiovascular disease and 28% had CKD. The mean number of antihypertensive agents used was 2.8 in the intensive group vs 1.8 in the standard treatment group. Although lower rates of heart failure events, cardiovascular deaths and total deaths were achieved with the intensive treatment, lower blood pressure failed to prevent CKD progression. Furthermore, patients exposed to the intensive treatment had a significant higher rate of acute kidney injury, electrolyte abnormalities, hypotension, and syncope.Citation4
Diabetics were excluded from the SPRINT trial. On the other hand, in the ACCORD trial, in patients with type 2 diabetes at high risk for cardiovascular events, targeting a SBP <120 mm Hg, as compared with <140 mm Hg did not reduce the rate of the composite outcome of fatal and nonfatal major cardiovascular events. Of note, the mean age was 62 years and the renal function was excellent, with GFRs in the 90s at baseline. Again, hypotensive episodes, electrolyte abnormalities and creatinine elevation were more common in the intensive treatment group.Citation9
The studies cited above are landmarks that provided physicians with scientific-based evidence for blood pressure treatment in a significant number of patients.
The question remains if those studies can be applied to elderly and frail patients. Several observational studies have assessed the association of blood pressure with mortality in older patients with CKD. Kovesdy et al found that patients with a SBP of 130 to 159 mm Hg combined with a DBP of 70 to 89 mm Hg had the lowest adjusted mortality rates, comparing to those with higher or lower BP readings.Citation10
Similarly, Simm et al, in a study of almost 400,000 hypertensive patients showed higher mortality rates for BP higher and lower than 130–139 mmHg systolic and 60–79 mmHg diastolic. In their study, patients older than 70 years had the lowest risk at a value of around 140/70 mmHg.Citation11
The oldest patients might be more susceptible to aggressive lowering of the blood pressure. In 21,000 patients older than 65 with stage 3–5 CKD not yet on dialysis, there was an increased mortality with a baseline SBP < 120 mmHg comparing to a SBP between 131–140 mmHg. A SBP higher >140 mmHg was associated with increased mortality only in the younger patients with CKD. These results remained significant even in patients with no heart failure.Citation12
Why older patients with CKD have increased mortality with lower blood pressure readings remains to be elucidated. The elderly have several alterations in blood pressure regulatory mechanisms and hypotensive episodes might increase the risk of syncope, organ hypoperfusion, electrolyte abnormalities, and worsening renal disease.
Excessive use of antihypertensive medications in older patients leads to serious fall injuries, hip and other major fractures, traumatic brain injuries, and joint dislocations, especially in patients receiving more intensive therapy.Citation13
Epidemiological studies show a linear rise in SBP between the ages of 30 to 80 and a concurrent early increase in DBP until the age of 50–60. Aging leads to increased vascular stiffness with a predominant increase in the systolic blood pressure and pulse pressure. Arterial stiffness is a risk factor for adverse cardiovascular events.Citation14,Citation15
It might be that older adults with multiple comorbidities and increased vascular stiffness are at risk of decreased organ perfusion with lower blood pressure targets. In this study, 237 patients (62.4%) had a pulse pressure above 55 mmHg and 162 (42.7%) patients had a pulse pressure higher than 60 mmHg. Furthermore, episodes of severe hypotension (SBP< 90 mmHg) were more common in those with SBP < 120 mmHg, affecting one third of the patients, with significant higher mortality.
Our results indicate increased mortality with a SBP < 120 mmHg in patients with significant disease burden (all patients had CKD, 50% had diabetes, a significant number had coronary artery disease, and cancer). Although this is a sicker population at baseline than the one studied in the SPRINT trial, it is representative of the type of patients that we see on a regular basis.
Twenty-five percent of the deaths were due to a cardiovascular event, with the 75% remaining due to a myriad of other conditions, reflecting the high burden of comorbidities in this type of population. This should prompt to individualization of therapy in each specific situation. Exposing older and sicker patients to lower blood pressure targets and polypharmacy might not benefit them given other competing conditions that would cause death even before a cardiac event ensues.
In this cohort, the prevalence of coronary artery disease and CHF was higher in those in the lower SBP group. Patients with SBP < 120 mmHg had more new cardiovascular events during the study period as well, but the association was not significant after adjusting for a history of prior cardiovascular disease.
A mean SBP < 120 mmHg remained significantly associated with increased mortality even after adjusting for multiple confounding factors, although the effects are less dramatic in those free from ongoing cardiovascular events.
One could argue these patients are managed more aggressively due to their comorbidities or have more severe cardiovascular disease, which translates into persistent hypotension. On the other hand, we have demonstrated previously in a similar population that avoidance of polypharmacy is associated with an improved GFR and a higher but still normal blood pressure, which points to some reversibility of the persistently low blood pressure readings at least at the beginning.Citation16
In regards of the renal outcomes, the number of events might be too small to make definite conclusions. A lower blood pressure goal was not associated with delay of CKD progression, but rather slightly worse renal outcomes.
Limitations of this study include the small sample size, retrospective nature which increases the possibility of bias, low number of minorities, and low number of events.
Conclusion
A systolic blood pressure below 120 mmHg in older patients with high disease burden was associated with adverse outcomes. Individualization of blood pressure therapy to each specific patient is warranted.
Disclosure statement
The authors disclose no conflict of interest.
References
- O’Hare AM, Choi AI, Bertenthal D, et al. Age affects outcomes in chronic kidney disease. J Am Soc Nephrol. 2007;18:2758–2765.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520.
- Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: A statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;16:14–26.
- Wright JT, Jr., Williamson JD, Whelton PK, et al. SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116.
- Bakris GL, Williams M. Preserving renal function in adults with hypertension and diabetes: A consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis. 2000;36:646–661.
- Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254.
- Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: The Dublin outcome study. Hypertension. 2005;46:156–161.
- Beckett NS, Peters R, Fletcher AE, et al. HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898.
- Cushman WC, Evans GW, Byington RP, et al. ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585.
- Kovesdy CP, Bleyer AJ, Molnar MZ, et al. Blood pressure and mortality in U.S. veterans with chronic kidney disease: A cohort study. Ann Intern Med. 2013;159:233–242.
- Simm JJ, Shi J, Kovesdy CP, Kalantar-Zadeh K, Jacobsen SJ. Impact of achieved blood pressures on mortality risk and end-stage renal disease among a large, diverse hypertension population. J Am Coll Cardiol. 2014;64:588–597.
- Weiss JW, Peters D, Yang X, et al. Systolic BP and mortality in older adults with CKD. Clin J Am Soc Nephrol. 2015;10:1553–1559.
- Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–595.
- Palombo C, Kozakova M. Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 2016;77:1–7.
- Madhavan S, Ooi WL, Cohen H, Alderman MH. Relation of pulse pressure and blood pressure reduction to the incidence of myocardial infarction. Hypertension. 1994;23:395–401.
- Franco Palacios CR, Haugen EN, Rasmussen RW, Thompson AM. Avoidance of polypharmacy and excessive blood pressure control is associated with improved renal function in older patients. Ren Fail. 2015;37:961–965.