Abstract
We challenged to identify the cutoff value of cTnT in chronic kidney disease (CKD) patients by point of care assessment way. A single center, prospective cross-sectional study was planned and performed. 201 consecutive patients who were visited emergency room for chest symptoms were enrolled in this study. All patients were performed routine practice for differential diagnosis of chest symptom by cardiologist. Simultaneously, semiquantitative measurement of cTnT was performed using same blood sampling on the blind condition to cardiologists for this study. Study patients were divided into four groups according to the estimated glomerular filtration rate (eGFR), CKD1-2, CKD3, CKD4-5, and CKD5D. Usefulness of semiquantitative measurement for diagnosing ACEs was investigated in each group. 77 (38%) of total patient was diagnosed as acute coronary events (ACEs). About 50% of patients were showing cTnT level less than 0.03 ng/mL. The cTnT level over 0.1 ng/mL was found in 30% of total subjects. Mean quantitative value of cTnT was 0.29 ± 0.57 ng/mL in total subjects. Estimated cutoff value in CKD3 patients was 0.088 ng/mL with a sensitivity of 59.3% and specificity of 80.0%. Interestingly, the cutoff values of CKD1-2, CKD4-5, and CKD5D were 0.047, 0.18, and 0.27 respectively, which are half, two times, and three times of CKD3 cutoff value 0.088. The specificities of four cutoff values in each CKD group were showing over 80%, which is higher than sensitivity, respectively. In CKD patients, semiquantitative, point of care assessment of cTnT could be a useful tool for screening for ACEs.
Introduction
The American Heart Association has recognized chronic kidney disease (CKD) as the strongest contributor to cardiac events. Among them coronary artery disease is still one of the major cause of death in those patients.Citation1 It has already reported in two major studies that a graded association was observed between a reduced estimated GFR and the risk of cardiovascular events including myocardial infarction.Citation2,Citation3 Angiographic assessment has shown that 40–50% of incident dialysis patients have had significant coronary artery disease (CAD).Citation4,Citation5 In order to differentially diagnose patients with suspicious cardiac events, cardiac biomarkers are useful tool in real-world clinical setting. Especially cardiac troponin I and T (cTnT) are components of the contractile apparatus of myocardial cells and are expressed almost exclusively in the heart. Elevations of these markers in the blood reflect injury leading to necrosis of myocardial cells.Citation6 Therefore, it is reported that cardiac troponins are good markers for identifying myocardial necrosis, but also cardiac systolic dysfunction,Citation7 left ventricular hypertrophy,Citation8 and CADCitation9 even in end-stage kidney disease (ESKD) patients.
A problem in the clinical setting is that, for CKD patients, there are no reference ranges for cardiac troponin that take into account, at least in part, kidney function. Indeed, nearly 30% of asymptomatic dialysis patients have shown cTnT levels above the cutoff value of 0.1 ng/mL for myocardial infarction.Citation10 This is thought to be a reason why cTnT does not often use for diagnosing acute coronary events (ACEs) in patients with renal insufficiency. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guideline recommended confirming dynamic change in the cTnT values of 20% or more for defining the ESKD patients with acute myocardial infarction.Citation11 However, it is not realistic in small clinic where CKD patients and dialysis patients are taken care usually that physicians measure cTnT two times in an interval of several hours and judge the difference of it. The ideal way for nephrologist is to be possible for diagnosing ACEs in advanced CKD patients by using cutoff value on single measurement like point of care assessment. To date, limited information are found about the cutoff value of cTnT for ACEs in CKD patients.
Therefore, in order to strengthen for diagnosing ACEs in CKD patients, we challenged to identify the cutoff value of cTnT in CKD patients. Moreover, in consideration of the practice style by noncardiologists in small clinic, simple, easy way, and point of care assessment were selected to measure cTnT in this study.
Materials and methods
Patients
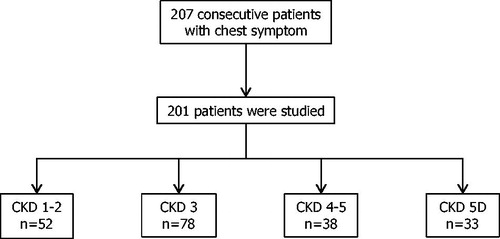
A single center, prospective cross-sectional study was planned and performed. From February to August 2011, 207 consecutive patients with chest symptom were visited emergency department at TOHO University Ohashi Medical Center. Six patients were excluded because of data unavailability. Finally, 201 patients were enrolled in this study. Then, all patients were performed routine practice for differential diagnosis of chest symptom by cardiologist. As regular way quick cTnT measurement was also performed at emergency department by qualitative test as usual which shows the level of cTnT over 0.1 ng/mL or less. Simultaneously, semiquantitative measurement of cTnT was also performed by using same blood sampling on the blind condition to cardiologists for this study. The measurement way is described in detail as follows. The patients were divided into four groups according to the estimated glomerular filtration rate (eGFR), CKD1–2, CKD3, CKD4–5, and CKD5D (). Usefulness of semiquantitative measurement for diagnosing ACEs was investigated in each group separately. Our study complied with the Declaration of Helsinki. Informed consent was obtained from all subjects. The ethics committee for clinical research of Toho University Ohashi Medical Center approved the study protocol [permission number: 22–55].
Data collection
Clinical information was recorded for all patients at the emergency department. According to the patients’ situation, patient and their family were interviewed to obtain data on age, sex, smoking habits, primary renal disease, previous hospitalizations, and history of hypertension, cardiac disease, and cerebrovascular disease. Information about the usage of medications was also collected. Blood pressure was recorded in the supine position, and a blood sample was collected just immediately after visiting emergency room. The body mass index (BMI) at optimal weight was calculated as the weight in kilograms divided by the square of the height in meters. The estimated glomerular filtration rate was calculated by using the Japanese equationCitation12 as follows; eGFR (mL/min/1.73 m2) = 194 × Cr−1.094 × age−0.287 (×0.739 for women). In this study, regardless the presence or absence of urine abnormalities, the patients with eGFR ≥90 mL/min/1.73m2 defined as CKD1, and the patients with eGFR 89–60 mL/min/1.73m2 defined as CKD2.
Measurement of cTnT
cTnT measurement was performed by Roche Cobas h232 CARDIAC T. The measurement is potable and fast testing way, and suitable for point of care assessment. Non-high-sensitive cTnT levels are shown as four patterns semiquantitatively, less than 0.03 ng/mL, 0.03–<0.1 ng/mL, 0.1–2.0 ng/mL (quantitative range), and >2.0 ng/mL. Only cTnT range of 0.1–2.0 ng/mL was displayed as numerical quantitative concentration.
Diagnosis of acute coronary event
ACEs were diagnosed by cardiologists on the blind condition to cTnT levels for this study. The definition of ACEs were defined as a patients with myocardial infarction and/or angiographical coronary narrowing >50% of reference segment. Myocardial infarction was defined according to the current definition of the joint criteria for the diagnosis of acute myocardial infarction by the European Society of Cardiology/American College of Cardiology/American Heart Association/WorldHeart Federation Task Force.Citation6
Statistical analysis
Data with normal distributions are expressed as the means ± standard deviations (SD). The data for parameters that did not have normal distributions are presented as the medians and interquartile ranges. The groups were evaluated using the χ2 test, analysis of variance, and the Kruskal–Wallis test. The optimal cutoff values for cTnT associated with ACEs were assessed by receiver–operator characteristic (ROC) curves. Except of cTnT quantitative range 0.1–2.0 ng/mL, dummy numerical values 0.029, 0.065, and 0.201 ng/mL were used for each categorical range <0.03 ng/mL, 0.03–<0.10 ng/mL, and >2.0 ng/mL respectively. Sensitivity, specificity, positive predictive value, and negative predictive value for ACES were calculated by using that value. p Values < .05 were considered significant. All statistical analyses were performed using IBM® SPSS® software version 20 (IBM Corporation, Armonk, NY).
Results
Patients’ characteristics
The patients’ baseline characteristics in each CKD groups are shown in . The mean age was higher in patients with CKD1–2 compared with those of CKD3 or more advance stage of CKD. Higher percentage of male and diabetes was observed in CKD5D than the other CKD groups. Interestingly, more chest pain/chest discomfort was found in patients with earlier stage of CKD, and converse phenomenon was observed in dyspnea. Lowest BMI was presented in CKD5D patients. Median NT-proBNP level was higher in more advanced stage of CKD. 77 (38%) of total patient was diagnosed as ACEs by cardiologist.
Table 1. Characteristics of 201 patients with chest symptoms.
Characteristics of cTnT in CKD groups
shows the distributions of patients in categorical levels of cTnT. About 50% of patients was showing cTnT level less than 0.03 ng/mL. The cTnT level over 0.1 ng/mL was found in 30% of total subjects. About 75% of patients with CKD1–2 were showing cTnT level less than 0.1 ng/mL, whereas about 50% of patients with CKD5D were showing cTnT level over 0.1 ng/mL. Mean quantitative value was 0.29 ± 0.57 ng/mL in total subjects, if dummy numerical values 0.029, 0.065, and 0.201 ng/mL were used for categorical range <0.03 ng/mL, 0.03–0.10 ng/mL, and >2.0 ng/mL respectively, and higher cTnT levels were observed in patients with more advanced stage of CKD.
Table 2. Distribution of patients in categorical cTnT levels.
Distribution of patients with ACEs in each categorical part of cTnT
In , percentages of patients with ACEs definitively are shown in separate category of cTnT level. About 75% of patients with cTnT less than 0.1 ng/mL were not suffered from ACEs definitely in total patients. About 65% and 85% of patients with cTnT 0.1–2.0 ng/mL and over 0.2 ng/mL were diagnosed ACEs, respectively. In CKD1–2 patients, around 70% of patients were diagnosed ACEs at relatively lower range of cTnT 0.03–0.1 ng/mL, whereas distribution of ACEs patients changed around cTnT level 0.1 ng/mL in CKD3 patients. Only 42% of patients were suffered from ACEs definitely in CKD4–5 patients with cTnT 0.1–2.0 ng/mL. In CKD5D, 40–60% of ACEs patients were observed in all three categories of cTnT ≥0.03 ng/mL. Considering these findings, it is suggested that higher cutoff value of cTnT for ACEs would be found in more advanced stage of CKD.
Table 3. Distribution of patients with ACEs in each categorical part of cTnT.
Cutoff value of cTnT on CKD patients
Optimal cutoff values for cTnT associated with ACEs were assessed by ROC curves in each CKD stage. Except of TnT quantitative range 0.1–2.0 ng/mL, dummy numerical values 0.029, 0.065, and 0.201 ng/mL were used for categorical range <0.03 ng/mL, 0.03–<0.10 ng/mL, and >2.0 ng/mL respectively. As shown in , estimated cutoff value in CKD3 patients was 0.088 ng/mL with sensitivity 59.3% and specificity 80.0%. Interestingly, the cutoff values of CKD1–2, CKD4–5, and CKD5D were 0.047, 0.18, and 0.27 respectively, which are half, two times, and three times of CKD3 cutoff value 0.088. The specificities of four cutoff values in each CKD group were showing over 80%, which is higher than sensitivity, respectively. Moreover, 75% or more of negative predictive values (NPVs) were observed in all CKD patients except of CKD1–2. These results imply false negative findings that 10–25% of CKD 3–5D patients had ACEs even though cTnT levels were lower than the potential cutoff values of each CKD groups.
Table 4. Cutoff value of cTnT for ACE in CKD patient groups.
Diagnostic accuracy of cTnT 0.1 ng/mL
shows the diagnostic accuracy of cTnT 0.1 ng/mL, which is known as the gold standard value for diagnosing ACEs. About 80% or more specificity and NPV were observed in CKD3 and 4–5 patients. In CKD 5D patients, all values of sensitivity, specificity, positive predictive value, and NPV were showing less than 70%.
Table 5. Diagnostic value of cTnT 0.1 ng/mL for ACE in CKD patient groups.
Discussion
Main findings of this study
To date, no reference ranges of cTnT for ACEs in advanced stage of CKD patients were found. This is thought to be a reason why cTnT does not often use for diagnosing ACEs in CKD patients, especially for advance stage. We challenged to identify the reference range of cTnT in four categorical stages of CKD patients, CKD1–2, CKD3, CKD4–5, and CKD5D. The strengthen point of this study is to measure cTnT quickly by using small portable system. As many CKD patients, even in dialysis patients, are taking care by physicians in small clinic which is not performed quick inspection, it is important clinical implication to evaluate the ability of quick measurement of cTnT by potable system for management of CKD patients in pre-hospital circumstance. Here, we would like to propose cutoff values of CKD stages for diagnosingACEs. Intriguingly, the cutoff values of CKD1–2, CKD4–5, and CKD5D were 0.047, 0.18, and 0.27 respectively, which are about half, two times, and three times of CKD3 cutoff value 0.088. Those cutoff values were associated with relatively higher percentage of specificity around 80% or more. These findings suggest that quick measurement of cTnT by potable system is useful for definitive diagnosis of ACEs in pre-hospital care. However, we need to pay attention to the false negative that 10–35% of CKD patients with below each potential cutoff values had ACEs.
Semiquantitative way
As mentioned in method section, Roche Cobas h232 can provide cTnT levels quickly, but semiquantitatively as four patterns, less than 0.03 ng/mL, 0.03–<0.1 ng/mL, 0.1–2.0 ng/mL (quantitative range), and >2.0 ng/mL. This means that our proposed cutoff value cTnT 0.047 ng/mL and 0.088 ng/mL for CKD1–2 and CKD3 are indicated as 0.03–<0.10 ng/mL, not showing numerically. As shown in , about 70% of CKD 1–2 patients with chest symptom had ACEs definitely, and about 90% of CKD3 patients with chest symptom did not have ACEs. Therefore, relatively rough judging way could be needed for patients with CKD1–2 and CKD3. In a similar way, it is better to know that all patients showing category cTnT >2.0 ng/mL have suffered from ACEs except of dialysis patients. We would like to emphasize that it is essential to use first all clinical signs such as symptoms, physical examinations, and other clinical tests for making a diagnosis for ACEs even in any CKD stage.
Cutoff value for ACEs
In this study, we proposed the cutoff values for ACEs in patients with various category of CKD. In CKD1–2 patients, nearly normal renal function, the cutoff value was 0.047 ng/mL, which is slightly higher than the level of 99th percentile of a normal reference population, 0.03 ng/mL of not high-sensitive cTnT. This is in line with the definition of the diagnosis for myocardial injury in international guideline for myocardial infarction.Citation6
In CKD3 patients, moderately impaired renal function, the cutoff value was increased up to 0.088 ng/mL. It is well-known that cTnT level is negatively associated with renal function.Citation13 Guclu et.al. also recently showed that high sensitive cTnT increases with decreasing eGFR values in outpatients without any chest symptoms. In their study, median cTnT level was 12.8 ng/L in CKD3 patients, which was almost two times higher in those of CKD1–2 patients.Citation14 This association is similar to our finding that the cutoff value in CKD3 was almost double of the cutoff value in CKD1–2. Moreover our proposed cutoff value 0.088 ng/mL in CKD3 patients would be supported by an evidence that cTnT 0.075 ng/mL is a potential candidate value for diagnosing significant coronary narrowing disease with sensitivity of 51% and specificity of 89% in CKD3 patients.Citation15
To our knowledge, there are few reports to examine the usefulness of cTnT for diagnosis of ACEs in CKD4–5 patients. In our study, 0.180 ng/mL was the best cutoff value for ACEs in CKD4–5 patients. Same as in CKD3 patients, it is reported that even patients without chest symptom and ACEs, high sensitive cTnT level was 29.0 ng/L in patients with eGFR 16 ml/min/1.73m2, which is near four times higher than cTnT level 7.3 ng/L in CKD1 patients. Same association was also found the cutoff values in our study between CKD1–2 and CKD4–5. Sittichanbuncha et.al. demonstrated that cTnT 0.200 ng/mL is useful value for diagnosing significant coronary narrowing disease with sensitivity 46% and specificity 94% in CKD4–5 patients.Citation15 This result may support our findings.
Extremely high cutoff value of cTnT 0.280 ng/mL for ACEs was observed in CKD5D patients in our study. This may be anticipated fully because it is reported that 53–59% of ESKD patients had a cTnT above the 10% coefficient of variation cutoff value.Citation16 Moreover, about 30% of stable HD patients without chest symptoms showed a cTnT level over 0.1 ng/mL.Citation10 A retrospective study from Korea revealed that 0.35 ng/mL is useful for identifying the ESKD patients with ACEs.Citation17 We interpret these results to indicate that around 0.3 ng/mL of cTnT may be a best cutoff value for diagnosing ACEs in ESKD patients.
The specificities of four cutoff values in each CKD group in this study were showing over 80%, which is higher than sensitivity, respectively. This means that cTnT assessment by this technique could be used to make a definitive diagnosis rather than an exclusive diagnosis. This tendency is supported by a recent evidence that point of care testing for cTnT is useful for diagnosing myocardial infarction with specificity 92%, which is higher than 68% of sensitivity in patients with almost normal renal function.Citation18 Finally, our proposed cutoff levels of cTnT for CKD patients were analyzed using dummy numerical values. Therefore, further study is needed to examine precise cutoff value in each CKD stages.
The present study had an important limitation in that the small number of patients involved could reduce the study power. Semiquantitative cTnT measurement was performed in this study. Therefore, dummy numerical values were used for identifying the cutoff value of cTnT in each CKD stage.
In conclusion, even in CKD patients, semiquantitative, point of care assessment of cTnT could be a useful tool for screening for ACEs. This easy way would help noncardiologists in small clinic for the management of CKD with chest symptoms.
Acknowledgements
The authors would like to express their appreciation to the cardiologists of Toho University Ohashi Medical Center for their kind support and assistance.
Disclosure statement
NJ has received financial support for this clinical research from Roche Diagnostics. The other authors declare that they have no conflicts of interest regarding this work.
Reference
- Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169.
- Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. New Engl J Med. 2004;351:1285–1295.
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. New EnglJ Med. 2004;351:1296–1305.
- Joki N, Hase H, Nakamura R, Yamaguchi T. Onset of coronary artery disease prior to initiation of haemodialysis in patients with end-stage renal disease. Nephrol Dial Transplant. 1997;12:718–723.
- Ohtake T, Kobayashi S, Moriya H, et al. High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: An angiographic examination. J Am Soc Nephrol. 2005;16:1141–1148.
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567.
- Satyan S, Light RP, Agarwal R. Relationships of N-terminal pro-B-natriuretic peptide and cardiac troponin T to left ventricular mass and function and mortality in asymptomatic hemodialysis patients. Am J Kidney Dis. 2007;50:1009–1019.
- Buiten MS, de Bie MK, Rotmans JI, et al. Serum cardiac troponin-i is superior to troponin-t as a marker for left ventricular dysfunction in clinically stable patients with end-stage renal disease. PLoS One. 2015;10:e0134245
- Hayashi T, Obi Y, Kimura T, et al. Cardiac troponin T predicts occult coronary artery stenosis in patients with chronic kidney disease at the start of renal replacement therapy. Nephrol Dial Transplant. 2008;23:2936–2942.
- Deegan PB, Lafferty ME, Blumsohn A, Henderson IS, McGregor E. Prognostic value of troponin T in hemodialysis patients is independent of comorbidity. Kidney Int.2001;60:2399–2405.
- Group NW, Wu AH, Jaffe AS, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: Use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem. 2007;53:2086–2096.
- Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992.
- Aviles RJ, Askari AT, Lindahl B, et al. Troponin T levels in patients with acute coronary syndromes, with or without renal dysfunction. New Engl J Med. 2002;346:2047–2052.
- Guclu T, Bolat S, Senes M, Yucel D. Relationship between high sensitivity troponins and estimated glomerular filtration rate. Clin Biochem. 2016;49:467–471.
- Sittichanbuncha Y, Sricharoen P, Tangkulpanich P, Sawanyawisuth K. The appropriate troponin T level associated with coronary occlusions in chronic kidney disease patients. Ther Clin Risk Manag. 2015;11:1143–1147.
- Roberts MA, Hedley AJ, Ierino FL. Understanding cardiac biomarkers in end-stage kidney disease: Frequently asked questions and the promise of clinical application. Nephrology (Carlton). 2011;16:251–260.
- Ryu DR, Park JT, Chung JH, et al. A more appropriate cardiac troponin T level that can predict outcomes in end-stage renal disease patients with acute coronary syndrome. Yonsei Med J. 2011;52:595–602.
- Vafaie M, Biener M, Mueller M, et al. Addition of copeptin improves diagnostic performance of point-of-care testing (POCT) for cardiac troponin T in early rule-out of myocardial infarction – A pilot study. Int J Cardiol. 2015;198:26–30.