Secondary hyperparathyroidism (SHPT) is a common complication in patients with end-stage renal disease (ESRD) and parathyroidectomy (PTX) is an effective treatment for SHPT. To examine the differential risk of post-surgical hyperkalemia after PTX for primary versus secondary hyperparathyroidism, we conducted a single-center retrospective observational study in 103 PTX patients admitted to the Third Affiliated Hospital of Soochow University between January, 2013 and August, 2019. Patients were divided into two groups according to pathogeny. PHPT group included symptomatic PHPT and asymptomatic PHPT with hypercalcemia. SHPT group included patients with maintenance hemodialysis for more than 3 months and having undergoing successful PTX. All SHPT patients received endoscopic total parathyroidectomy and forearm autotransplantation (tPTX + AT), while PHPT patients underwent open or endoscopic parathyroid adenomaectomy. shows the clinical characteristics of patients. No patients in PHPT group were diagnosed as hyperkalemia after surgery, while postoperative serum potassium (K+post) was more than 5.3 mmol in 28 (52.8%) patients with SHPT. Then, SHPT patients were further divided into hyperkalemia group and nonhyperkalemia group according to K+post. Compared with nonhyperkalemia group, K+base and K+pre were significantly higher in hyperkalemia group (, p < 0.001). Preoperative iPTH and the decline range of iPTH in hyperkalemia group were higher than those in nonhyperkalemia group, but there was no statistical significance (p = 0.095, p = 0.066). There was no significant difference in age, gender, BMI, dialysis age, HCO3-, Hb, BUN, SCr, ALP, Chol, TG, UA, serum-corrected calcium, phosphorus, magnesium, ACEI/ARB, Cinacalcet between two groups (). We chose the variables with p < 0.1 for multivariate Logistic regression analysis. K+pre was an independent influencing factor of postoperative hyperkalemia (OR = 18.888, 95%CI = 1.798–198.450, p = 0.014). ROC curve analysis showed that area under the curve (AUC) of K+pre in predicting postoperative hyperkalemia was 0.844 (p < 0.001). The optimal cutoff value of K+pre to predict hyperkalemia in SHPT patients after tPTX + AT was 4.30 mmol/L, with a sensitivity of 96.4% and a specificity of 56% ().
Figure 1. Receiver operating characteristic (ROC) curve of preoperative serum potassium associated with postoperative hyperkalemia.
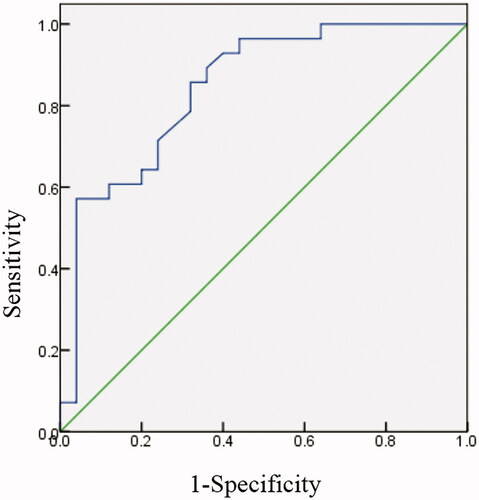
Table 1. Comparison of perioperative clinical data of patients with SHPT and PHPT.
Table 2. Demographic features of hyperkalemic and nonhyperkalemic groups of postoperative patients with SHPT.
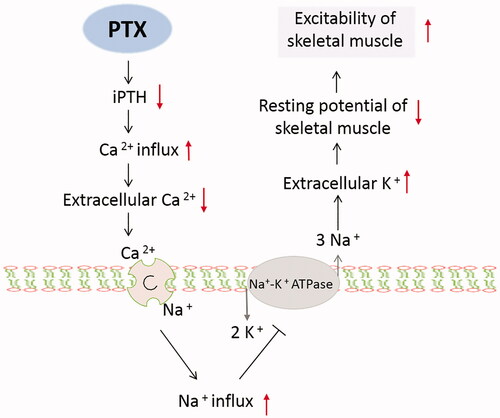
Hyperkalemia after PTX in hemodialysis patients is common. Previous study has found that serum potassium could rise rapidly from 4.4 mmol/L to 6.2 mmol/L within operation time [Citation1]. Rapidly rised severe hyperkalemia could lead to serious arrhythmia, even life-threatening [Citation2]. Risk of hyperkalemia is more ominous in face of coexisting hypocalcemia (which is expected take place after PTX), so this issue is getting more and more attention in recent years. In our study, the incidence rate of hyperkalemia in hemodialysis patients after PTX is 52.8%, which is consistent with 25-80% occurrence reported in previous studies [Citation3–7]. We speculate that the rapid decline of iPTH in a short time is an important reason for hyperkalemia after PTX. The possible interpretations are shown in . Due to a rapid decline of iPTH after patients undergoing PTX, a large number of calcium ions influx into the bone make the level of calcium in extracellular fluid (ECF) in skeletal muscle cells (SMC) decrease [Citation8]. An increased influx of sodium ions into SMC via membrane barrier action of sodium–calcium exchanger may influence the activation of Na/K ATPase pump which can promote efflux of sodium ion and influx of potassium. These result in increased level of potassium in ECF, reducing resting potential and increasing excitability of SMC [Citation9–10]. A small sample study showed that ESRD patients with prior treatment with cinacalcet had a higher risk of hyperkalemia and hypocalcemia during and immediately after PTX [Citation11]. However, we did not detect the significant association. Recent study has found preoperative serum potassium level <3.9 mmol/L would reduce the risk of developed potassium level >5.3 mmol/L in hemodialysis patients [Citation12]. According to our study, reducing the K+pre below 4.30 mmol/L is helpful to decrease the incidence of postoperative hyperkalemia.
Department of Nephrology, The Third Affiliated Hospital of Soochow University, Changzhou, China
Liwei Zhang
Department of Infection Management, The Third Affiliated Hospital of Soochow University, Changzhou, China
Hua Zhou, Yan Yang, Min Yang and Jia Di
Department of Nephrology, The Third Affiliated Hospital of Soochow University, Changzhou, China
[email protected]
Ethical approval
The study was approved by the Ethics Committee of the Third Affiliated Hospital of Soochow University, China (registration number 26/2019) and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Shpitz B, Korzets Z, Dinbar A, et al. Immediate postoperative management of parathyroidectomized hemodialysis patients. Dial Transplant. 1986;15:507–530.
- Rosenkrans DJ, Kolarczyk LM. Intraoperative hyperkalemia and ventricular arrhythmia during parathyroidectomy: a case report. A Case Rep. 2017;9(4):105–108.
- Yang G, Wang J, Xing C, et al. Perioperative hyperkalemia in hemodialysis patients undergoing parathyroidectomy for renal hyperparathyroidism. Intern Emerg Med. 2019;14(7):1065–1071.
- Hayes JF, Gross GF, Schuman ES. Surgical management of renal hyperparathyroidism in the dialysis patient. Am J Surg. 1982;143(5):569–571.
- Bajaj Y, Roberts S, Simon D, et al. Intra-operative hyperkalemia: a serious but under recognised complication of renal parathyroidectomy - a prospective study: how we do it. Clin Otolaryngol. 2011;36(1):69–72.
- Yang YL, Lu HF, Chung KC, et al. Young age, male sex, and end-stage renal disease with secondary hyperparathyroidism as risk factors for intraoperative hyperkalemia during parathyroidectomy. J Clin Anesth. 2015;27(3):195–200.
- Li S, Liu S, Chen Q, et al. Clinical predictor of postoperative hyperkalemia after parathyroidectomy in patients with hemodialysis. Int J Surg. 2018;53:1–4.
- Lu KC, Ma WY, Yu JC, et al. Bone turnover markers predict changes in bone mineral density after parathyroidectomy in patients with renal hyperparathyroidism. Clin Endocrinol (Oxf)). 2012;76(5):634–642.
- Clausen T. Na+-K + pump regulation and skeletal muscle contractility. Physiol Rev. 2003;83(4):1269–1324.
- Gonzalez-Serratos H, Hilgemann DW, Rozycka M, et al. Na-Ca exchange studies in sarcolemmal skeletal muscle. Ann N Y Acad Sci. 1996;779:556–560.
- Chong GC, Choi JDW, Lee TT, et al. Intraoperative and postoperative hyperkalaemia after total parathyroidectomy following exposure to cinacalcet in sixteen patients for renal hyperparathyroidism. Clin Otolaryngol. 2017;42(6):1369–1373.
- Song YH, Cai GY, Chen XM, et al. Can we predict who will develop postoperative hyperkalaemia after parathyroidectomy in dialysis patients with secondary hyperparathyroidism? BMC Nephrol. 2019;20(1):225–233.