Dear Editor,
Psoriasis is an immune-mediated chronic inflammatory disease that frequently affects the skin and joints and has been linked to several coexisting diseases, including diabetes, hypertension, metabolic syndrome, and atherosclerosis [Citation1]. Retinoids and immunosuppressive agents are the most commonly used systemic treatments for patients with moderate to severe psoriasis. However, for some patients, their efficacy remains unsatisfactory. Secukinumab, a fully human monoclonal IgG1 antibody with a molecular weight of 151 kDa that selectively binds IL-17A and inhibits its biological activity, has shown improved efficacy in clinical trials. Focal segmental glomerulosclerosis (FSGS) is a type of renal pathology, which is relatively rare in psoriasis patients. Here, we present the first case of FSGS in a plaque psoriasis patient who was successfully treated with secukinumab.
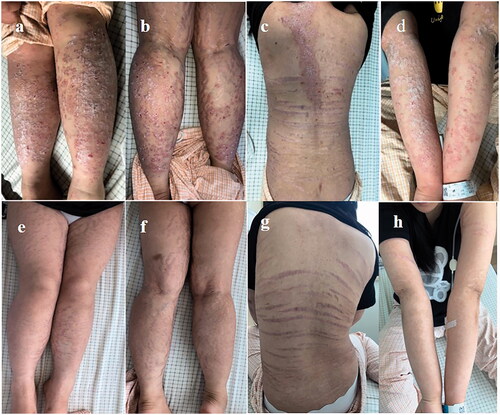
A 21-year-old female was admitted to nephrology department of our hospital for the first time for ‘persistent proteinuria and hyperuricemia for more than one year’ on 12 December 2019. She had plaque psoriasis when she was 15-year-old and never received systemic psoriasis treatment. She was diagnosed with ‘severe preeclampsia’ at 30 weeks of pregnancy in 2018. Her blood pressure was well managed by taking oral perindopril tert-butylamine tablets and the edema had gone away before this visit, but proteinuria had no improvement. The patient denied having any history of other diseases or a family history of psoriasis. Physical examinations: blood pressure, 123/72 mmHg; height, 158 cm; weight, 80 kg (BMI > 30 kg/m2). Scattered red plaques covering massive scales were on her back and extremities (). The striae atrophicae caused by long-term topical steroid preparations use appeared on her back (). She had no extremities edema. Other physical findings of the patient were normal.
Figure 1. Diffuse distribution of plaques and scales on the back (c) and extremities (a,b,d) before treatment. Psoriasis Area and Severity Index (PASI) score was 47.0. The lesions completely subsided after one month of secukinumab treatment (e–h). PASI score was 0.
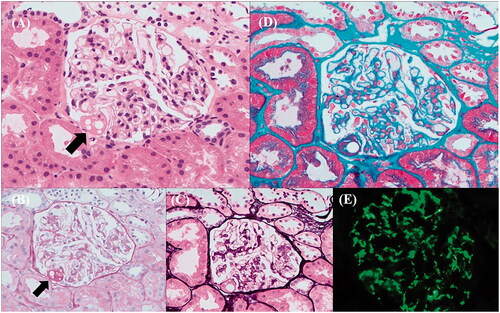
The laboratory examinations were performed. 24-hour(h) urine protein quantification, 0.891 g/d [normal, 0–0.150]; uric acid, 491.0 μmo/L [normal, 142.8–339.2]. Except for urine protein 3+, erythrocyte, leukocyte, cast and crystal on urine analysis were normal. Renal function was normal, with creatinine at 50 μmoI/L [normal, 41–73], urea at 4.20 mmol/L [normal, 2.60–7.50], and albuminemia at 50.4 g/L [normal, 40.0–55.0]. The blood and stool routine, the aldosterone/renin concentration ratio, and glycosylated hemoglobin were all normal. Abdomen CT scan revealed fatty liver. Immunoglobulin (Ig) A level was mildly elevated at 4.39 g/L [normal, 0.7–4.0] and ANA was 1:100 positive. The GBM-IgG, anti-PLA2R, ANCA, anti-dsDNA, the serum complement, and the IgG, IgM values were within normal limits. Viral serologies for HIV, hepatitis B and C were negative. The kidney biopsy was performed on 19 December 2019. On light microscopy, it showed partial glomerular ischemia shrinkage, adhesion balloon in the affected segment, and interstitial inflammatory infiltration, glomerular podocyte swelling, mesangial matrix slightly expanded (). The tubules showed a few erythrocyte and protein casts. Immunofluorescence was negative for IgG, IgA, C3 and C1q, only positive for IgM. Combining the medical history and pathology, the diagnosis of FSGS was considered first.
Figure 2. Pathology of kidney biopsy: (A: HE staining; B: PAS staining; C: PASM staining) partial glomerular ischemia shrinkage, an area of balloon adhesion, local capillary loop cavity dilation, plasma protein-like exudation in segmental capillary lumen and Bowman capsule wall, glomerular podocyte swelling, mesangial matrix slightly expanded (black arrows: the balloon adhesion). (D: Masson staining) mesangial area suspected a small amount of eosinophilic protein deposition. (E: Immunofluorescence staining) IgM (3+) deposition in the mesangial region.
She was hospitalized for nephropathy in our hospital several times, mainly to receive perindopril tert-butylamine tablets to control blood pressure and reduce urinary protein, as well as febuxostat pills to lower uric acid. However, there was no discernible change in urinary protein or uric acid from December 2019 to March 2021 (). In March 2021, she was hospitalized once more for severe psoriasis. Dermatologists recommended secukinumab (300 mg) injections into her subcutis on 18 March, 25 March, 1 April, 8 April, and 15 April, and then every 4 weeks until now. Meanwhile, she continued taking perindopril tert-butylamine tablets and febuxostat pills, and the moisturizer was applied to the lesions.
Figure 3. The first time secukinumab application was on 18 March 2021. Here is the change in the urinary protein, serum uric acid and PASI score (vertical thick arrow with Bx: the date of kidney biopsy; vertical thin arrows: the date of every dose of secukinumab).
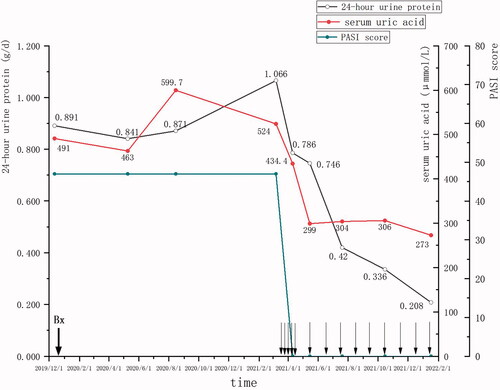
The patient's lesions appeared to improve after 1 week of secukinumab application, and all lesions disappeared after 1 month, with continuous remission up to now (). On 10 April 2021, the Psoriasis Area and Severity Index (PASI) score dropped from 47.0 to 0, and we could see that both 24-h urine protein and serum uric acid decreased significantly following the start of secukinumab therapy (). Surprisingly, as psoriatic lesions improved, we observed a sustained decrease in 24-h urine protein from April 2021 to January 2022, and serum uric acid decreased to the normal level (). Her weight dropped to 66 kg after 2 months of treatment and maintained this lever all the time (BMI = 26.4 kg/m2). Furthermore, her serum creatinine remained standard level throughout the period.
In recent years, psoriasis comorbidities, particularly cardiovascular diseases and diabetes, have received increased attention, but kidney diseases have received less. The term ‘FSGS’ refers to a clinicopathologic syndrome characterized by significant proteinuria and podocyte injury, as well as lesions of focal and segmental glomerular sclerosis and foot-process effacement. We gathered all the reported cases of FSGS with psoriasis () [Citation2–4]. The potential pathogenic significance of this uncommon association between psoriasis and FSGS is unknown, and the mechanism of pathogenesis must be determined. IL-17A, as a member of the IL-17 cytokine family, plays an important role in the pathogenesis of psoriasis. Patients with minimal-change nephrotic syndrome and IgA nephropathy have elevated levels of IL-17A in their urine [Citation5]. IL-17 promotes the production of pro-inflammatory cytokines and chemokines by renal tubular epithelial cells, but neutralizing IL-17A potentially improves renal pathology [Citation6]. IL-17A deficiency protects mice from glomerular and tubular injury by inhibiting the activation of distal tubular transport proteins, particularly sodium chloride co-transport proteins, and epithelial sodium channels [Citation7]. IL-17A also has been shown to play a crucial role in promoting vascular inflammation and atherosclerosis in renal impairment. There is substantial experimental evidence that the Th17/IL-17 axis is involved in the pathogenesis of glomerulonephritis, which can aid in the development of promising therapeutic strategies for treating various forms of glomerulonephritis.
Table 1. Cases of FSGS with psoriasis.
Microalbuminuria is common in preeclampsia, and the glomerular damage may be irreversible. Our patient had a history of preeclampsia as well as postpartum hypertension. Some preeclampsia patients show increased expression of IL-17 in the circulation and placenta. Proteinuria in preeclampsia may be associated with IL-17-induced podocyte apoptosis. Therefore, we concluded that FSGS in our case was most likely secondary to preeclampsia, and IL-17 may be vital in this course. Furthermore, in some patients with psoriasis and psoriatic arthritis, serum uric acid levels are elevated. The Th1 and Th17 cytokine pathways have been shown to play an important role in the pathogenesis of gout, with elevated levels of IL-17 in the peripheral blood and joints of gout patients [Citation8]. The improvement of psoriatic lesions in our patient following secukinumab treatment was accompanied by a significant decrease in her serum uric acid level. More research is needed to determine the link between IL-17 and the development of gout.
Proteinuria and blood uric acid alone improved when psoriatic lesions regressed after the start of secukinumab in our case, implying that IL-17A inhibition may be effective not only against psoriasis but also against FSGS to some extent. IgA nephropathy with psoriasis was reported to have improvements in skin lesions and urinary protein after treatment with secukinumab [Citation9]. Our patient experienced no side effects from secukinumab treatment and showed a trend of improvement in proteinuria. As previously stated, in this case IL-17A may act as a common pathway in psoriasis, FSGS, and hyperuricemia. Our shortcoming was that we did not collect the datas of serum/urinary IL-17A during treatments. We had no objective evidence to identify the change of IL-17A, so the role of IL-17A in the pathogenesis of renal damage and psoriasis requires further investigation. Biologic agents do not influence long-term renal function in psoriasis patients with chronic kidney disease, and whether their early intervention reduces progression to end-stage renal disease requires further investigation. Overall, this case suggested the use of IL-17A antagonist is beneficial not only for the relief of psoriatic lesions but also for the improvement of the clinical symptoms of the kidney, offering a safe and effective therapeutic option in managing psoriasis combined with nephropathy in the future.
Informed consent
Informed consent was obtained from the patient for the publication of this report.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76(3):826–390.
- Sirolli V, Bonomini M. Glomerulopathies associated with psoriasis: a report of three cases. Nephron. 2000;86(1):89–90.
- Ceri M, Kurultak I, Unverdi S, et al. An unusual cause of focal segmental glomerulosclerosis: psoriasis vulgaris. Ren Fail. 2010;32(5):639–641.
- Pradhan SK, Beriha SS. Focal segmental glomerulosclerosis associated with psoriasis. Saudi J Kidney Dis Transpl. 2014;25(3):670–671.
- Matsumoto K, Kanmatsuse K. Increased urinary excretion of interleukin-17 in nephrotic patients. Nephron. 2002;91(2):243–249.
- Schmidt T, Luebbe J, Paust HJ, et al. Mechanisms and functions of IL-17 signaling in renal autoimmune diseases. Mol Immunol. 2018;104:90–99.
- Norlander AE, Saleh MA, Kamat NV, et al. Interleukin-17A regulates renal sodium transporters and renal injury in angiotensin II-induced hypertension. Hypertension. 2016;68(1):167–174.
- Liu Y, Zhao Q, Yin Y, et al. Serum levels of IL-17 are elevated in patients with acute gouty arthritis. Biochem Biophys Res Commun. 2018;497(3):897–902.
- Ochi M, Toyama T, Ando M, et al. A case of secondary IgA nephropathy accompanied by psoriasis treated with secukinumab. CEN Case Rep. 2019;8(3):200–204.
