Abstract
Background: It is important to understand patterns and predictors of initiation and engagement in treatment for Medicaid-covered individuals with substance use disorders because Medicaid is a major source of payment for addiction treatment in the United States. Our analysis examined similarities and differences in predictors between adults and adolescents. Methods: An analysis of Oregon Medicaid claims data for the time period January 2010 through June 2015 assessed rates of substance use and of treatment initiation and engagement using the Healthcare Effectiveness Data and Information Set (HEDIS) definitions. The analysis included individuals aged 13–64 with a new alcohol and other drug dependence diagnosis who met the HEDIS enrollment criteria and did not have cancer. We created 4 logistic regression models to assess treatment initiation and engagement, separately for adults (ages 18–64) and adolescents (ages 13–17). Independent predictors included age, gender, race, the interaction of gender and race, urban/rural residence, presence of any chronic disease, a psychiatric diagnosis, or a pain diagnosis. Results: Among adults, odds of initiation were lower in white males than in nonwhite males, white females, and nonwhite females. Conversely, among adolescents, odds of initiation were higher in white males than in the other gender/race groups. Predictors of initiation also went in opposite directions for presence of a psychiatric diagnosis (negative in adults, positive in adolescents) and urban residence (positive in adults, negative in adolescents). We found similar patterns in models of engagement, although for engagement those with a psychiatric diagnosis had lower odds of engagement in both adults and adolescents. Conclusions: Predictors of treatment initiation and engagement for alcohol and drug use disorders differed between adults and adolescents on Medicaid. A better understanding of these differences will enable development of targeted treatment programs that are effective within age groups.
Introduction
Medicaid expenditures for treatment of substance use disorders are expected to double from $5.2 billion to $11.9 billion between 2009 and 2020.Citation1 The prevalence of substance use disorders is elevated among Medicaid populations compared with commercially insured populations,Citation2,Citation3 but little is known about drivers of successful treatment in this population. Evidence about adolescents is particularly sparse. Fewer than half of pediatricians screen adolescents for substance use, and most of these do not use standardized instruments.Citation4 Fewer than 10% of adolescents with a substance use disorder (SUD) are referred for treatment.Citation5 The National Committee for Quality Assurance (NCQA) reports national rates of initiation and engagement for adults and adolescents combined. In 2010, the rate of initiation was 43% for Medicaid members, falling slightly to 41% in 2016. Rates of engagement were quite low, at 14% in 2010 and 12.5% in 2016.Citation6
Eligibility for Medicaid varies by state. Oregon expanded Medicaid coverage in 2014 as part of the Affordable Care Act. Prior to expansion, pregnant women were covered up to 185% of the Federal Poverty Guidelines (FPG); parents were covered up to 40% FPG; other nondisabled adults were not covered; and children were covered up to 300% FPG (through the Children’s Health Insurance Program, or CHIP). After Medicaid expansion, pregnant women were covered up to 190% FPG: parents were covered up to 138% FPG; other nondisabled adults were covered up to 138% FPG; and children were covered up to 305% FPG through CHIP.Citation7 Thus, the increase in the Medicaid population in Oregon after expansion was primarily among parents and other nondisabled adults.
Given the high rates of substance use, the low rates of engagement in treatment, and the public financial impacts of addiction in this population, it is important to understand predictors of initiation and engagement, information that could lead to better targeted treatments. Therefore, we provide an analysis of treatment initiation and engagement among Oregon Medicaid members between 2010 and 2015, focusing on similarities and differences between adults and adolescents with SUD, in order to provide insight on the factors associated with higher and lower treatment initiation and engagement rates.
Methods
We obtained de-identified Oregon Medicaid data for the time period January 2010 to June 2015 under a data use agreement with the Oregon Health Authority. The data set included Medicaid enrollment, claims, and pharmacy data. The Oregon Health and Science University Institutional Review Board approved the study protocol.
Study population
The analysis included Medicaid recipients aged 13–64 who had a new diagnosis of alcohol or other drug (AOD) dependence based on the Healthcare Effectiveness Data and Information Set (HEDIS) definition for AOD, which includes abuse of alcohol, opioids, cannabis, cocaine, amphetamines, hallucinogens, and antidepressant drugs, or a sedative-, hypnotic-, or anxiolytic-related disorder, or the onset of delirium tremens, based on ICD-9 (International Classification of Diseases, Ninth Revision) codes.Citation8 HEDIS defines a new AOD diagnosis as one without an AOD diagnosis in the previous 60 days and also requires that members are continuously enrolled in Medicaid for at least 60 days prior to the new AOD diagnosis and 44 days after the AOD diagnosis.Citation8 We excluded members who were dually eligible for Medicare (because we did not have access to Medicare claims data) or had cancer.
Initiation and engagement definitions
We used HEDIS definitions to identify initiation and engagement in treatment (IET): Patients initiated treatment if they had an inpatient admission with a substance use diagnosis, or an outpatient visit, intensive outpatient encounter, or partial hospitalization within 14 days of the diagnosis. Patients engaged in treatment if they initiated treatment and had at least 2 subsequent inpatient or outpatient encounters with a substance use diagnosis within 30 days after initiation. The denominator for both rates was defined as enrollees with a new AOD diagnosis.Citation8
Statistical analysis
We performed bivariate tests of initiation and engagement with independent variables of interest stratified by adolescents and adults using the last time unit in the study period (January–June 2015). We developed 4 logistic regression models that predicted initiation and engagement separately over the entire study period, stratified by age group: adolescents (ages 13–17) and adults (ages 18–64). Independent variables included indicators for time in 6-month periods from January–June 2010 (the reference category) to January–June 2015; age, gender, race (non-Hispanic white compared with nonwhite); urban or rural residence, defined from zip codes and the Rural Urban Commuting Area (RUCA) algorithmCitation9; presence of any psychiatric diagnosis; acute pain diagnosis, or chronic pain diagnosis; and presence of any chronic diseases based on the Chronic Illness and Disability Payment System (CDPS), which was developed for use with Medicaid populations.Citation10 We excluded cancer, substance use disorder, and psychiatric illness categories from the CDPS for this analysis; cancer was an exclusion criterion, psychiatric diagnosis was considered separately, and all members had a substance use disorder diagnosis. Standard errors were clustered at the individual member level to account for members who had more than 1 new diagnosis of AOD dependence during the study period and thus had multiple observations in the model. Nonwhite races and ethnicities were grouped together due to small numbers among adolescents in some of the nonwhite groups. This grouping also facilitated investigation of potential interactions between those of white versus nonwhite race/ethnicity and gender, and between race/ethnicity and time. Additional potential interactions between gender and rural/urban residence and between gender and time were investigated.
Results
In the first half of 2010, a total of 198,505 Medicaid members aged 13–64 were eligible for this analysis, increasing to 689,565 by 2015. Most of the increase came from adults added during Accountable Care Act (ACA) expansion in 2014. The overall rate of members with an SUD diagnosis remained flat at around 3% during the study period; adults had slightly higher rates than adolescents ().
Table 1. Sample description.
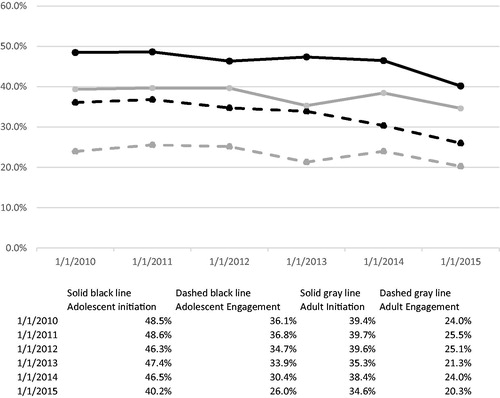
Among adolescents, the initiation rate was 48.5% in 2010 and dropped to 40.2% by 2015. Among adults, the initiation rate was 39.4% in 2010 and dropped to 34.6% by 2015. The patterns for engagement were similar; in 2010, the engagement rate in adolescents was 36.1%, falling to 26.0% in 2015, and in adults the engagement rate was 24.0% in 2010, falling to 20.3%. ().
Figure 1. Rates of treatment initiation and engagement in adults and adolescents, 2010–2015. Solid black line: Adolescent treatment initiation rate. Solid gray line: Adult treatment initiation rate. Dashed black line: Adolescent treatment engagement rate. Dashed gray line: Adult treatment engagement rate.
In the unadjusted tests, rates of initiation did not differ by gender, race, or urban/rural location in either adults or adolescents. In adults, rates of initiation were lower in those with chronic or acute pain, a psychiatric diagnosis, or any chronic disease. A similar pattern was seen in adolescents, with slightly lower rates of initiation in those with any chronic condition, acute pain, or chronic pain. However, none of the differences reached statistical significance in adolescents (). For engagement, rates were higher in males among adolescents and among Asians and Hispanics among adults. For adults, rates of engagement were strongly significantly higher among those with no chronic conditions, no psychiatric diagnoses, and no acute or chronic pain. Again, similar trends were seen in adolescents for the predictors based on diagnoses, but with weaker or no significance in the differences ().
Table 2. Bivariate tests of treatment initiation and engagement.
In logistic regressions, odds of treatment in the final time period (January–June 2015) were significantly lower than in the initial time period (January–June 2010) in all 4 models: initiation and engagement, separately among adults and adolescents. For the most part, the odds did not differ significantly from the initial time period until 2012 in adults and 2014 in adolescents.
In both initiation and engagement models, the direction of association for several covariates differed between adults and adolescents. Among adults, odds of initiation were lower for individuals with psychiatric diagnosis, but in adolescents psychiatric diagnoses were associated with a higher likelihood of initiation. Conversely, urban residence was associated with a higher odds of initiation in adults but lower odds in adolescents. Interactions between race and gender were included in all 4 models. In the initiation model for adults, white males had the lowest odds of initiation, whereas in the model for adolescents white males had the highest odds of initiation. Associations were more consistent for other predictors: Adults and adolescents with chronic disease and with acute pain were less likely to initiate treatment. Chronic pain had a significant negative association with initiation in adults but not in adolescents ().
Table 3. Logistic regression results for treatment initiation.
In the models of engagement, once again the association with urban residence was positive in adults and negative in adolescents, and white males had the lowest odds among race/gender groups in adults but the highest odds in adolescents. The predictors related to diagnoses were more consistent; the presence of any chronic disease, psychiatric diagnosis, and acute pain diagnosis were all associated with a reduction in the odds of meeting the engagement measure for both the adult and adolescent models ().
Table 4. Logistic regression results for treatment engagement.
Discussion
Oregon saw significant declines in the adjusted odds of both initiation and engagement in treatment between 2010 and 2015, both in adults and in adolescents. Declines in treatment initiation and engagement rates were also seen nationally as reported by NCQA,Citation6 although the decline in Oregon appeared more pronounced than the national trend. A decreasing trend in medication treatment for SUD between 2009 and 2014 among youths was also reported by Hadland et al.Citation11 Although more attention has been given in recent years to problems of addiction to opioids and other drugs, this does not appear to be leading to increased treatment rates either in Oregon or nationally.
Predictors of treatment initiation differed between adults and adolescents, with psychiatric diagnosis, urban versus rural residence, and gender and race having opposite effects in the 2 age groups. No previous literature was found that included predictors for both adolescents and adults, so we are unable to verify whether this finding is consistent with previous work. However, literature looking at patterns of treatment in adults had mixed findings on treatment predictors. These articles used different sample inclusion criteria, different definitions of treatment, and different types of insurance coverage. Yarborough et al. looked specifically at the HEDIS initiation and engagement measures in adults with commercial or Medicare insurance and reported lower odds of treatment initiation among nonwhite compared with whites and higher odds among patients with psychiatric diagnoses, but gender was not significant.Citation12 Stein et al. found follow-up treatment in Medicaid adults to be higher in females and those with serious mental illness and lower in urban areas. They also reported rates lower in African Americans compared with whites but higher in Hispanics.Citation13 However, their study looked at subsequent engagement in treatment after detox or residential treatment. McCaul et al. also found a significant interaction between gender and race in the length of treatment among adults, with white males receiving the longest treatment, followed by white females, African American males, and African American females.Citation14
For adolescents, it was noted that SUD is one of the most frequently missed diagnoses by primary care providers,Citation5 and that there are lower rates of pediatricians trained and waivered to prescribe buprenorphine compared with family and internal medicine providers.Citation15 Also, adolescents are less likely than either adults or younger children to have preventive care visits, so the adolescents with SUD included in this analysis may overrepresent those with comorbidities requiring office visits.Citation16
One analysis looked at receipt of medication-assisted treatment for opioids in a national sample of youth aged 13–25 and found that rates were lower in females and nonwhite race/ethnicities, but that there was no difference in metropolitan versus nonmetropolitan areas.Citation11 Another looked at adolescents aged 12–17, most of whom had commercial insurance, and found that females had lower odds of treatment than males and blacks had lower odds than whites.Citation17
It is probable that the apparent inconsistencies in predictors in previous work are due to differences in definitions and populations, making it difficult to determine the consistency of our findings with that work. For example, restricting the sample to those with Medicaid coverage could have a major impact on findings related to treatment in both adolescents and adults, as Cummings et al. reported that counties with higher proportions of nonwhite residents and those in rural areas were less likely to have any outpatient SUD treatment facilities that accepted Medicaid, which would limit access among some subsets of Medicaid members.Citation18
Some of the differences in predictors between adults and adolescents may be explained by external factors that are often the motivating reasons for adolescents to enter treatment, such as parents, schools, or the criminal justice system.Citation19
This study has a number of limitations. First, it is restricted to Medicaid members in one state, Oregon, and the degree to which these findings apply to other states is not known. Second, claims data are limited in completeness, and because they are created for administrative/financial uses, they do not contain all of the detail that would be useful for research purposes. Third, collapsing nonwhite racial and ethnic groups due to small counts in some of these groups precludes us from examining the heterogeneities among these groups in relation to treatment initiation and engagement.
Nonetheless, this analysis illustrates that there is substantial room for improvement in rates of SUD treatment in Medicaid members. Furthermore, our findings suggest that there is substantial heterogeneity in initiating and engaging treatment and that these differences are not consistent when comparing adults and adolescents. Whereas adult women and nonwhite adults had rates of initiation and engagement that were comparable to or better than their white male counterparts, these findings ran in the opposite direction for adolescents. In particular, our findings suggest substantial disparities for adolescent females and racial minorities both in treatment and engagement. These findings suggest that efforts to improve treatment and engagement generally may need to differentiate strategies for adult and adolescent populations. In particular, efforts that may be successful for improving these measures for adult populations may be ineffective for adolescent populations and, depending on the strategies, could exacerbate existing racial and gender disparities.
Author contributions
DM and RB were involved in the conception and implementation of the study. BKL and YG performed the statistical analysis and wrote the first draft of the manuscript. BKL, DM, YG, RB, and KJM contributed to the discussion section and revisions to the manuscript. All authors approved the final manuscript.
Additional information
Funding
References
- Andrews C, Abraham A, Grogan CM, et al. Despite resources from the ACA, most states do little to help addiction treatment programs implement health care reform. Health Aff. 2015;34(5):828–835
- Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167:293–301.
- Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP Study. Pain. 2008;138(2):440–449.
- Harris SK, Herr-Zaya K, Weinstein Z, et al. Results of a statewide survey of adolescent substance use screening rates and practices in primary care. Subst Abus. 2012;33(4):321–326.
- Beaton A, Shubkin CD, Chapman S. Addressing substance misuse in adolescents: a review of the literature on the screening, brief intervention, and referral to treatment model. Curr Opin Pediatr. 2016,28:258–265
- National Committee for Quality Assurance. http://www.ncqa.org/report-cards/health-plans/state-of-health-care-quality/2017-table-of-contents/alcohol-treatment. Accessed March 26, 2018.
- The Henry J. Kaiser Family Foundation. The Kaiser Family Foundation state health facts: trends in Medicaid income eligibility limits. https://www.kff.org/data-collection/trends-in-medicaid-income-eligibility-limits/. Accessed August 16, 2018.
- National Committee for Quality Assurance. HEDIS 2014: healthcare effectiveness data and information set. Technical specifications for health plans. Vol 2. Washington, DC: National Committee for Quality Assurance; 2013.
- Rural-Urban Commuting Area Codes. US Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. Accessed March 26, 2018.
- Kronick R, Gilmer T, Dreyfus T, Lee L. Improving health-based payment for Medicaid beneficiaries: CDPS (chronic illness and disability payment system). Health Care Financ Rev. 2000;21(3):29.
- Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr. 2017;171(8):747–755.
- Yarborough BJ, Chi FW, Green CA, et al. Patient and system characteristics associated with performance on the HEDIS measures of alcohol and other drug treatment initiation and engagement. J Addict Med. 2018;12:278–286.
- Stein BD, Kogan JN, Sorbero M. Substance abuse detoxification and residential treatment among Medicaid-enrolled adults: rates and duration of subsequent treatment. Drug Alcohol Depend. 2009;104:100–106.
- McCaul ME, Svikis DS, Moore RD: Predictors of outpatient treatment retention: patient versus substance use characteristics. Drug Alcohol Depend. 2001;62:9–17.
- Levy S, Mountain-Ray S, Reynolds J, Mendes SJ, Bromberg J. A novel approach to treating adolescents with opioid use disorder in pediatric primary care. Subst Abuse. 2018;29:1–9.
- Ozechowski TJ, Becker SJ, Hogue A. SBIRT-A: adapting SBIRT to maximize development fit for adolescents in primary care. J Subs Abuse Treat. 2016;62:28–37
- Winstanley EL, Steinwachs, Stitzer ML, Fishman MJ. Adolescent substance abuse and mental health: problem co-occurrence and access to services. J Child Adolesc Subst Abuse. 2012;21(4):310–322.
- Cummings JR, Wen H, Ko M, Druff BG. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190–196
- Yeterian JD, Greene MC, Bergman BG, Kelly JF. Does mandated treatment benefit youth? A prospective investigation of adolescent justice system involvement, treatment motivation, and substance use outcomes. Alcohol Treat Q. 2013;31(4):431–434
