ABSTRACT
The objective of this research was to understand the effect of pet ownership on healthcare-seeking behavior among persons experiencing homelessness with animals. Mixed-method, semi-structured interviews were conducted with 44 people experiencing homelessness with animals in Seattle, Washington to collect stories of barriers and facilitators due to animal ownership, health-seeking behaviors for themselves and their animals, and self-assessed health status and health conditions of the owners and their pets. The interviews also explored the ways in which the participants would like to receive healthcare services for themselves and their animals. Quantitative results showed that the medical care sourced for pets exceeded that for the owner’s own health, with 86% of participants seeking healthcare for themselves within the past year and 93% of participants seeking veterinary care for their pet within the past year. Results also displayed self-described health of the animal faring better than that of the owner, with 47% of participants reported being “Healthy” or “Very healthy” compared with 90% of pets being reported as the same. Themes emerging from the qualitative research included that persons experiencing homelessness with animals place a high value on the health and welfare of their pets, that the animals can pose a barrier to traditional health services and access to overall services, and that the owner’s need for animal companionship and support is high. These findings suggest that utilizing the human–animal bond and creating integrated (human and animal), interprofessional health services using a One Health approach for unhoused populations owning pets can reduce barriers to services and improve both human and animal health. In an integrated health clinic setting, the owner may seek care for their animal but stay for the human healthcare.
Background
Homelessness rates in the United States have been steadily increasing over the last decade, with roughly 568,000 people counted during the 2019 national One-Night-Count, with large metropolitan cities such as Los Angeles, New York City, and Seattle leading the numbers (Henry et al., Citation2020). While the number of individuals experiencing homelessness with animals has not been officially counted, an estimated 6–24% of this population experience homelessness with a dog, cat, or other animal (Cronley et al., Citation2009; Irvine et al., Citation2012; Rhoades et al., Citation2015). Many qualitative studies have shown the self-stated benefits and detriments of animal ownership while unhoused. Stated benefits include companionship, sense of purpose, and protection (Cleary et al., Citation2019; Gillespie & Lawson, Citation2017; Rew, Citation2000). Barriers caused by animal ownership include restricted access to shelters, housing, and services due to building restrictions (Howe & Easterbrook, Citation2018; Kerman et al., Citation2020; Rhoades et al., Citation2015), accessing personal healthcare (Howe & Easterbrook, Citation2018; Toylor et al., Citation2004), increased social integration barriers (Irvine et al., Citation2012), and additional stigmatization of pet ownership (Irvine et al., Citation2012; Scanlon et al., Citation2020; Toylor et al., Citation2004).
Human Health Aspects of Homelessness
Living in homelessness has been well documented to have many negative effects on health. Amongst those experiencing homelessness there is an increased prevalence of a range of infectious diseases, psychiatric disorders, sexually transmitted diseases, and substance misuse/addiction (Edidin et al., Citation2012), as well as higher rates of premature mortality than the rest of the population, especially from suicide and injuries (Desai et al., Citation2003; Morrison, Citation2009; Votta & Manion, Citation2004; Zhang et al., Citation2019). High rates of non-communicable diseases, chronic diseases, and age-related conditions, such as cognitive impairment and functional decline have also been described, with evidence of accelerated aging (Fazel et al., Citation2014). Limited access to medical coverage, coupled with competing priorities such as food insecurity and barriers to transportation, contribute to low rates of healthcare utilization. Nearly two-thirds (64%) of responses from Seattle/King County’s Count Us In Survey, a yearly survey that counts the number of sheltered and unsheltered people experiencing homelessness during the last 10 days of the month of January, reported living with at least one health condition (Winslow et al., Citation2020). The most frequently reported health conditions were psychiatric or emotional conditions (36%), post-traumatic stress disorder (35%), and drug or alcohol abuse (32%). Twenty-seven percent (27%) of respondents reported chronic health problems and 23% reported a physical disability. The rates of these health conditions in homeless populations exceed those in the general (housed) population in Seattle/King County in all case except in reports of physical, mental, or emotional disabilities, which is comparable at 22.4% in the general population (King County Hospitals for a Healthier Community, Citation2020; Public Health- Seattle & King County, Citation2021).
Access to healthcare has been shown to affect people experiencing homelessness differently based on age, sex, and gender identity. Women living in homelessness have disproportionate physical, behavioral, and social health burdens compared with homeless men (Muñoz et al., Citation2005). Transgender health outcomes are shown to be even more negatively impacted owing to pervasive cultural stigmas and violence that increase risk of homelessness and unstable housing as compared with cisgender peers (Minter & Daley, Citation2003; Spicer, Citation2010). Surveys of homeless youth identify barriers to accessing healthcare which may be both structural (limited clinic sites, limited hours of operation, priority health conditions, and long wait times) and social (perception of discrimination by uncaring professionals, law enforcement, and society in general) (Hudson et al., Citation2010).
Health Impact of the Human–Animal Bond
The human–animal bond, defined by the American Veterinary Medical Association (Citationn.d.) as “a mutually beneficial and dynamic relationship between people and other animals that is influenced by behaviors that are essential to the health and wellbeing of both,” is important for community health and has been documented in numerous studies to improve the emotional, psychological, and physical health between people, animals, and the environment (Barcelos et al., Citation2020). Curl et al. (Citation2017) reported that people who had a greater attachment with their dogs were more likely to both walk their dogs and to walk them for more minutes, which was associated with better health and health behaviors. Pet ownership has been shown to be beneficial for those with mental health conditions (Brooks et al., Citation2018; Gan et al., Citation2020; McNicholas et al., Citation2005), though ownership and end-of-life concerns can negatively impact mental health (Friedmann & Krause-Parello, Citation2018; Hawkins et al., Citation2021; Scanlon et al., Citation2021a). Research on animal-assisted therapy reports positive health impacts in clinical settings (Coakley et al., Citation2020), while other studies show the benefits of service animals to veterans experiencing Post-Traumatic Stress Disorder (Johnson et al., Citation2013; O’Haire & Rodriguez, Citation2018; Yarborough et al., Citation2018).
Numerous studies have reported benefits of animal ownership on the mental health of owners (Lem et al., Citation2016; Rhoades et al., Citation2015). Research exploring the effects of animal companionship while experiencing homelessness reveals benefits including friendship, responsibility, and improved emotional wellbeing (Arkow, Citation2020; Howe & Easterbrook, Citation2018; Rhoades et al., Citation2015). Addiction research suggests that pets such as dogs can be used as transitional objects in the treatment of patients with drug dependency (Toylor et al., Citation2004). Levels of animal attachment and empathy in the homeless community may surpass those relationships found in the housed community (Irvine, Citation2013a; Toylor et al., Citation2004), aligning with findings that people experiencing homelessness with their animals often tend to have a “pet-first” approach to resources (Irvine, Citation2013b). Specifically, pet health and wellbeing have often been reported as being prioritized over the owner, with the animals receiving food and care first (Irvine et al., Citation2012; Rhoades et al., Citation2015). To date, however, little research has causally linked animal ownership in homeless populations to improved health outcomes of owners (Kerman et al., Citation2019).
Limited research has been done looking at the health of pets owned by those living in homelessness. In an owner-reported study, Williams and Hogg (Citation2016) found that dogs owned by persons experiencing homelessness were generally healthy and less likely to be obese or exhibit behavioral issues such as aggression to strangers and separation anxiety, when compared with dogs from the housed community (Williams & Hogg, Citation2016). A recent publication utilizing a veterinary team and assessment tool to assess dog health and wellbeing indicates that while obesity may be lower than the housed population, it is still high in dogs living in homelessness (Scanlon et al., Citation2021a). Additionally, Scanlon et al. report high rates (61.9%) of behavioral problems in dogs, most often separation anxiety. Additional research is necessary to address this gap in the data.
Arkow (Citation2020) and Kerman et al. (Citation2020) suggest that increased attention to the human–animal bond can improve the delivery of services provided by social workers, identify their clients’ risk and resiliency factors, enhance social and environmental justice, expand academic inquiry, and increase attention to all of the vulnerable members of families and communities. Additionally, Kerman et al. (Citation2020) discuss the need for an integrated care model to support people experiencing homelessness with pets.
In order to investigate whether leveraging the human–animal bond could promote access to healthcare for the human–animal unit, we conducted a mixed-method study among persons in Seattle experiencing homelessness with their animals to further explore these issues. The goal of the research was to develop frameworks for utilizing the strength of the human–animal bond in order to improve access to health services for both the humans and their animals using a One Health approach to clinical care – an approach that simultaneously considers the health of humans, animals, and their shared environment.
Methods
Study Team
The study team included three young adults with lived experience of homelessness who provided outreach to their peers and acquaintances as well as an introduction to the community for the research. The team also included a human health specialist and an anthropologist.
Research Study Design
All study protocols were reviewed and approved by the University of Washington’s Institutional Review Board (STUDY00005322). Additional attention was given to provide unaccompanied minors Human Subjects Protection in the event they had no legal guardian to provide consent.
Mixed-method, semi-structured, one-on-one interviews were conducted with persons experiencing homelessness with animals in Seattle, Washington State, from October 2018 to June 2019. The interview instrument included 62 questions, both quantitative and qualitative in nature, and was written and reviewed for content by co-investigators from nursing, social sciences, law, and public health. Quantitative survey questions were used to collect data about the health of the participants and their pets utilizing a review of systems approach, which collects an inventory of signs and symptoms, as well as including questions to identify barriers and facilitators to services using yes/no and Likert-scale response formats. For each quantitative question, respondents were asked, using open-ended questions, to expand on the response. Qualitative questions were phrased in an open-ended format to solicit themes in the narrative. Drafts of questions were reviewed and piloted by one of the authors and the community members with lived experience of homelessness for culturally appropriate language and understandability.
Inclusion criteria were owning at least one animal and being currently or at risk of homelessness. We utilized the definition of homeless/at risk of homelessness provided by the Department of Housing and Urban Development and thus including rough sleepers, couch surfers, those living in cars or RVs, and those in shelter or transitional housing (Losinski et al., Citation2013; US Department of Housing and Urban Development, Citation2019). Additionally, owing to the difficulties of transitioning into traditional housing, we also included those who were housed within the previous year.
Recruitment of Participants and Conduct of Interviews
Recruitment occurred in Seattle. Animal owners experiencing homelessness were recruited through a number of different outreach methods. Utilizing the relationships built with service providers in the city, case managers and shelter/drop-in staff provided information about the project with clients who owned animals and utilized their services. Additionally, members of the research team actively walked and drove through neighborhoods to look for potential participants to enroll in the study.
All interviews were held in locations requested by the participant, including shelter spaces, coffee shops, and outdoor spaces. Interviews were facilitated by three members of the research team trained in qualitative data collection, to minimize variance in data collection styles and methods (Bernard, Citation2017). Two of the three interviewers had lived experience of homelessness, though currently housed, and the third was a medical anthropologist.
Prior to the interviews, participants provided oral consent to participate in the study. Researchers worked with shelter caseworkers and counselors to create a trauma response protocol in the event interview questions raised difficult emotions or past traumatic episodes. The protocol included ending the interview early and immediately connecting the participant with a healthcare specialist. Additionally, all participants were given the option to skip any questions they did not want to respond to. All participants were advised that they would be referred to by pseudonyms in order to preserve their anonymity, and all but one participant gave permission to be directly quoted in research reports.
Interviews averaged 35 minutes in length, and participants were provided incentives of $15 and a bag of pet food for their participation. All qualitative components in the interviews were audio-recorded using cell phone voice-recording applications and were manually transcribed by study staff in preparation for coding and theme identification. Quantitative survey responses were recorded on paper forms and later entered into an electronic database.
Data Analysis
Deductive and inductive coding strategies were used to identify study themes. As the overall project contained two separate but related research arms – one using the interview methods indicated above and one exploring similar themes through PhotoVoice (manuscript forthcoming) – the leads of each arm of the research together generated and defined deductive codes a priori to be used across both datasets. Codes and their definitions were stored in a data dictionary accessible to all coders. As additional themes emerged from the data, inductive codes were added and defined by the leads. This allowed for a more reflexive coding practice across the two arms of the study, allowing for the richer themes to arise from the images and text.
Transcribed interviews were entered and coded in ATLAS.ti V.8.4.18.0. The first and third authors coded all transcripts to apply intercoder reliability to the analysis. All incongruences were discussed and a decision was made to utilize one code or to keep both codes. These discussions also at times included refining the definition of the code in the codebook to add additional reflexivity and a further depth to the understanding of the codes. The interview recordings were used to clarify any responses.
Themes were identified as those leading to reoccurring patterns of meaning, consistent with Braun and Clarke’s (Braun et al., Citation2014; Braun & Clarke, Citation2013) “central organizing concept.” They were generated from codes with shared meaning derived from responses across the complete interview tool.
The authors utilized a critical realist analytical approach as a means to integrate reflexive thematic analysis (TA), codebook TA, and quantitative methods with which to build knowledge on this new line of research (Fletcher, Citation2017; Wiltshire & Ronkainen, Citation2021).
Quantitative data were entered into Microsoft Excel (Microsoft, Richmond WA) and cleaned. Descriptive and statistical significance tests were calculated using R Version 3.6.3 (R Core Team, Citation2019) with an a priori p-value threshold of 0.05. The non-parametric Fisher exact test was used owing to a small dataset. An a priori sample size calculation, with a two-sided alpha of 0.05, required a sample size of 203. Likert-scale survey results were treated as ordinal data for analysis.
Results
Demographics
Forty-four persons experiencing homelessness, with a total of 53 animals, participated in the study. All were English speakers and the study team did not have to refrain from enrolling a participant in the study owing to language barriers. Participant demographics closely paralleled the age, race/ethnicity and gender of the homeless population in Seattle (Winslow et al., Citation2020), though with a higher representation of Native American/Indigenous participants. All age groups were represented (). Participants identified their housing status as streets/sleeping rough, city-sanctioned encampments, shelters, RV/mobile home, government-funded housing, transitional housing, couch surfing, recently housed, other, and two or more of the options ().
Table 1. Participant age (mean, SD), gender, race/ethnicity, housing status.
Although some respondents indicated that, because their animals were service animals or emotional support animals, they should not be considered “pets,” the authors chose to use the terms pets and animals interchangeably for brevity. Additionally, some respondents would not use the term “ownership” to define the relationship between themselves and their animal, but for the context of this paper we have used this term to denote the human–animal pair. Finally, the sample size varies in the following results as some participants were not able to answer all the questions, for various reasons.
Health Status
Responses from participants’ self-reported health status covered all components of the health systems checklist, and 90% (38/42) indicated that they had two or more comorbidities. The most commonly reported health issue was psychiatric problems, which was reported by 71% (29/41) of respondents. The major psychiatric problems were depression, anxiety, and/or PTSD (). Bipolar disorder, “paranoia,” and obsessive compulsive disorder were each only reported by one individual.
Table 2. Human health conditions.
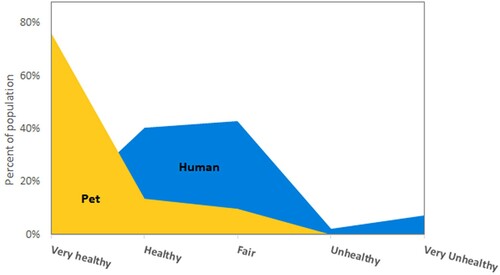
Participants were asked to rank both their own and their pet’s overall health on a Likert scale (1–5), with 1 being “Very Unhealthy” and 5 being “Very Healthy.” Owing to our small study size, we used a two-sided Fisher exact test and found significant differences in health status between participant health status and pet health status (p < 0.001). Most participants rated themselves as “Fair”/“Healthy,” while most pets were rated as “Very Healthy” ().
Time Since Last Healthcare Visit
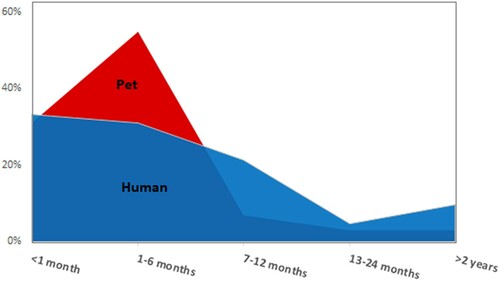
We did not find significant differences between participant time since last doctor visit and pet time since last veterinarian visit (Fisher exact test p = 0.1501). When asked about time since their last doctor or veterinary visit, most participants’ pets (86%) had visited a provider within the past month (31%) or in the past 1–6 months (55%). Only one participant reported their pet had not seen a veterinarian in more than two years. By contrast, a lower percent of owners had visited a healthcare provider in the past 6 months (64%), with one-third of the participants reporting having seen a healthcare provider in the past month (33%), and approximately one-third reporting a healthcare visit in the past 1–6 months (31%). Four (10%) of the 40 participants reporting health status reported not having seen a healthcare provider in more than 2 years ().
Interest in Accessing Healthcare
Sixty-one percent of participants were interested in veterinary primary healthcare for their pet, while only 43% of those same participants were interested in primary healthcare for themselves. Seven participants (16%) reported having trouble accessing healthcare because of their pets. Among these, when asked if they would seek health services at a clinic that provided healthcare for both themselves and their animals, six participants (86%) indicated that they would.
Qualitative Findings – Themes
Although the experience of every individual was distinct, common themes emerged from the interviews pertaining to needing the animal for personal health, animals as a barrier to accessing resources, animal barriers causing health problems, animals as priorities, harassment from the community owing to animal ownership, and interest in a clinic serving both humans and animals.
Theme 1: Needing the Animal for Personal Health
Companionship
In an open-ended question of “What do you feel are the benefits of you having a pet?” all respondents reported similar benefits related to companionship, such as “It’s really nice to be able, like, to have that companion … to have an animal to call yours and be able to take care of and make you feel you have a purpose in life, you know, like to take care of an animal,” “He never says anything bad – never tells me I’m a criminal, or I’m a lawbreaker, a drug addict, a junkie” and “When I get home from work, he’s really excited, and I feel like he’s the only one that does that. He’s just real happy just to see me exist.”
Emotional Support
More specifically, the majority of participants indicated that their animals provided a service for their health. In fact, 56% of respondents indicated that their animals provided emotional support. A common theme included a “need” for the animals to be present in order to prevent mental health episodes:
I have to have her because I get anxiety attacks when stuff doesn’t work out the way it’s supposed to, in a timely manner … She keeps me calm ‘cause if I freak out completely, it would get me put in jail, or something worse.
And when I’m going through something he knows, and he goes ‘Mom, I’m here for you. ‘Cause I have PTSD.
She helps me a lot with anxiety. When I get really upset and don’t have to go to [the] ER, I sit there and pet and talk to her, and she just lays there right on my stomach until I feel better.
Other respondents indicated that while their animals were not officially “service animals” because they did not have formal training, they did provide services for their owner:
Actually, my vision is pretty poor and it’s going out. I was born pretty blind – I’ve had several operations – and he’s helped me out with that. A couple of weeks ago I found out I have cataracts on my eyes, too … Even him just walking in front of me, stepping on and off curbs, that really helps me. I watch him … I got the best eyes and ears in town!
Theme 2: Animals as Barriers to Accessing Healthcare, Housing, and Other Resources
Dependence on an animal for emotional support and/or companionship can also be problematic for those experiencing homelessness as access into certain buildings can be prohibitive for those animals not fitting in to the federal definition of “service animals.” Over half of the respondents indicated animal ownership as a barrier to accessing shelters, receiving supportive needs, and accessing housing.
Many respondents spoke of sleeping outdoors because the shelter would not permit their animals, while others reported being unable to access housing because of no-pet laws or not being able to pay the additional rental charges for their pet.
If I were still trying to find a new place to live, and it wouldn’t let me keep my dog around; if it was between having my dog or staying on the street – it wouldn’t even be a decision for me. I’d go back to the street in a second. And I feel like 90% of dog owners are like that, unless they have a family or other obligations.
A number of respondents indicated that animal ownership was a barrier to accessing healthcare for themselves. This was owing to animals not being allowed inside the premises and not having a place to leave the animals while they were away.
I have been putting off dental treatment because it may require a day surgery or something and I need to be here for her. So until we get stabilized in our own place and I know she is going to be alright, I am not going to do it. I don’t have a babysitter.
That was a leap of faith. I was so sick about 2 months ago. I had an anxiety attack so bad, I couldn’t talk. It was awful. And I had a seizure that day too. The doctor says, I think you should go to [the hospital where the dog was not allowed]. I made a decision to come back here and tough it out. It was the right decision.
Theme 3: Animal Ownership Barriers Causing Health Issues
Some respondents followed up on this refusal of access to services by describing negative health repercussions owing to the stress involved in the altercations serving as a confluence of themes 1 and 2.
I walked 6 miles to go there, to this particular shelter, at night. They said, you can’t have a dog in here and they threw me in the street. I had a major panic attack. I called the cops myself, they sent me to [the hospital] and sorted me out. I needed my Ativan.
One story in particular told of barriers caused by animal ownership leading directly to negative human health and wellbeing outcomes. Not being allowed to bring their non-service animal (but still essential support dog) into a federal building for check-ins with the judge served as a detriment to the participant’s personal health as well as the image they presented before the judge or probation officer.
Like [the] courthouse, they don’t allow a PTSD or anxiety animal with you … I got to go and stand in front of the judge. And I can’t stand in front of the judge without my dog, … It’s just not fair to me, because it’s just making me and my anxiety go kind of through the roof, while I am sitting there talking to you, when I can be calm, cool, and collected, and not be shaking my knee 25,000 times, and doing this, and scratching myself, because I am all anxious and nervous, and you think I am on drugs, so then you take a piss test, and you find out I am not. But you think something is not right, and I am hiding something – no, I am anxious, and panicky, I can’t find that comfort that I need that she gives me, and that’s really hard on me.
Theme 4: The Animal’s Care Prioritized Above Self-Care
Most respondents indicated that their pet’s wellbeing took priority over everything else, including their own needs. Reponses resonated along this common theme:
If I’m gonna eat, I make him food first before I eat. If I can’t eat, I’m still gonna feed my dog, that’s my main priority, he’s my dog. I don’t care if I don’t eat, but my dog needs to eat and have food and water I don’t care about anything else.
Theme 5: Harassment from the Community Because of Animal Ownership
Sixty-seven percent of respondents expressed experiencing harassment from the community; this was a common theme in the open-ended interview responses. Harassment often translated into emotional stressors, ranging from different standards for those in homelessness with animals on public transportation to accessing services. Those who indicated that their animal met the local definition of a service animal indicated that they met disbelief from the community and businesses about the animal’s qualifications because of their homeless status:
She’s a service dog and I face discrimination every day just because people don’t always understand that you can have an invisible illness that isn’t exactly seen, and you don’t have to be blind to have a service dog. I have had harassment, I’ve had to call the police on establishments, I’ve filed complaints with the ADA, I’ve had arguments, I’ve had screaming matches, I’ve broken down crying from being kicked out of a place.
Theme 6: Interest in Concept of a Clinic Providing Healthcare for Both Owner and Animal
The majority of respondents indicated that they would utilize a clinic where they and their animals could receive healthcare at the same visit. They cited the reduction of transportation barriers, and the saving of time, where both the human and animal health issues could be addressed at once. Responses to the interest in a human–animal clinic included:
Yeah that would be extremely useful, that would be very useful. Say I have the flu, my dog has diarrhea, it makes it to where I can get taken care of, get my antibiotics, and my dog gets checked out.
It would be convenient for both of us, because I’m getting checked and my dog’s getting checked. and it would be at the same place, instead of multiple places. One and done.
Two ducks, one stone.
One individual said they might use the clinic depending on what services were offered, and two respondents said they would not because their cats would not respond well.
Discussion
Our mixed-methods study of the health impacts of animal ownership among people experiencing homelessness in the Seattle area produced several key findings. For many owners, the pets provided important companionship and emotional support. At the same time, persons experiencing homelessness with pets reported harassment from community members owing to their animal ownership; and there were barriers to housing and healthcare owing to the animal ownership. Participants rated the health of their animals as being better than their own health, and many indicated that they would prioritize healthcare for their animals over healthcare for themselves, although the direction of correlation is unable to be parsed out as pet health being a higher priority may in turn be leading to better pet health outcomes. The overwhelming majority of participants responded positively to the concept of being able to receive healthcare services at a clinic offering integrated human and veterinary healthcare.
Our finding that animals were providing important companionship and emotional support as well as other specific health benefits was consistent with previous studies regarding the physical, psychological, and emotional benefits of pet ownership within the unhoused community (Irvine, Citation2013a). In our study, health benefits ranged from support navigating street curbs owing to vision impairment and retrieving necessary items for the owner, to intentional physical response to an adverse health event like seizure or state of panic, to simply being available to provide passive emotional support. Participants used words such as “need” and “have to have” to describe their relationship with their animals, regardless of whether they described the animal as a service animal, emotional support animal, companion animal, or pet.
Similarly, the reported barriers to housing and healthcare owing to animal ownership were consistent with previous reports. These barriers included housing, accessing services, and entering buildings (Henwood et al., Citation2020; Scanlon et al., Citation2020). At the same time, other studies have reported higher rates of healthcare access problems owing to pets (Howe & Easterbrook, Citation2018; Rhoades et al., Citation2015); in our study this was reported by only 16%. This discrepancy could be owing to a number of factors, including the existence of social networks that allow people to leave their pet with a trusted individual, local pet-friendly policies for healthcare facilities, or as a result of people not seeking the care they need. Further research should examine regional variation in the impact of pet ownership on healthcare access.
Participants Reported High Rates of Adverse Medical Conditions
Participants self-reported an average of 5.59 medical issues and comorbidities, higher than the age-adjusted mean number of comorbidities (2.22–2.32) in the general population of Washington State (Akinyemiju & Moore, Citation2016). Participants reported high rates of psychiatric problems followed by musculoskeletal, respiratory, and neurological issues. This increased prevalence of chronic disease problems – along with lower reported health-seeking behavior as compared with their animals – indicate a pressing need for improved access to healthcare, including mental health and medical specialty care.
An important theme emerging from our analysis was the negative health implications of harassment from the community owing to a person’s relationships with their animals. At their most extreme, harassment events resulted in hospital visits owing to panic attacks and altercations with the police. In less severe cases, harassment led to continuation of sleeping outdoors as they were refused access owing to their companion animal. These findings suggest there is an unseen health impact of harassment related to coping mechanisms when one is unhoused with an animal (Irvine et al., Citation2012).
Animals in Better Health and Have Had Their Healthcare Prioritized Above Owners
In contrast to their own self-reported health, owners reported their animals to be in better health than themselves, with most pets having received veterinary care more recently than the owner had received healthcare. To add additional contrast, it should be noted in that the animals described as “Fair”/“Unhealthy” were geriatric with age-relevant issues. Themes of the care of the animal being a priority flowed through the majority of the interviews where, like Irvine described in 2013 (Irvine, Citation2013b), the pets would receive food first. Additionally, effort would be made to ensure it was “good food,” often defined as food from specialty animal stores, “grain-free,” and not found at the Foodbank or on supermarket shelves.
Interest in a Clinic Model Providing Both Human Healthcare and Veterinary Care
Interest in utilizing a clinic with joint human and veterinary healthcare was overwhelmingly popular. Since some participants also reported that they would rather search out healthcare for their animals before themselves, it suggests that a clinic providing human health and veterinary care at the same site could lower barriers to the owner receiving healthcare services. This could be most beneficial in those human–animal pairs where the owner is reporting barriers to accessing human healthcare owing to animal ownership.
Strengths and Limitations
This study had a number of strengths, which included conducting semi-structured interviews with 44 animal-owning participants ranging from ages 15 to 66, and we received many overlapping responses and distinct responses owing to experience and age. The data provided valuable insight into the health status of owners and their animals, as well as into health-seeking behaviors and needs. Narratives of animal ownership and what their animals meant to them validated previous studies’ themes on companionship, support, and love. Additionally, responses highly supported the creation of a clinic to meet the healthcare needs of both owner and pet at the same time, citing that a clinic like this would reduce barriers and provide the support both owners and animals need.
The study also had some limitations. The authors center the experiences of the study participants, while recognizing that the study sample size limits representation of a larger community. Additionally, although the participants of the study were representative of the demographics of Seattle’s homeless population, there are considerable differences between the sub-communities in the overall community, and the number of participants in each group are small. Funding for homeless services often follows age brackets where there are resources for youth under 18, those 18–26, and then for those over that age. So, while the study had representation from every age group, the number in each is small. Future research could explore differences of health issues related to animal ownership between age groups, housing types (rough sleeper, shelter users, RV community, etc.) gender, and other groups. Further research may also be needed for more representative and generalizable data.
An additional limitation is that the study only utilized self-reported human and animal health status and healthcare visits, instead of clinical chart records, which could lead to social desirability bias in the responses.
Finally, the study was restricted to a community with specific regulations affecting animal ownership. Seattle is a particularly animal-friendly city where, in 2011, dog ownership outnumbered children by over 45,000, and in 2015, cat households were reported to be 50% greater than households with children, making up 17% more households than dog households (Balk, Citation2013; Wurn, Citation2011).
Conclusion
Overall, the results of this research display the general health of animal-owning persons experiencing homelessness in Seattle, as well as the positive and negative health impacts of animal ownership while unhoused. The data clearly show that homeless pet owners prioritize seeking healthcare for their animals before fulfilling their own healthcare needs. Owners also report that the lack of societal acceptance of pet ownership in this demographic is a significant barrier to accessing healthcare. Services should consider using an integrated, interprofessional One Health approach that considers the health needs of the human and their pet to successfully provide them healthcare.
Acknowledgements
Foremost, the authors thank all those who agreed to participate in this research. Without their patience and trust, we could not keep working toward equitable health and healthcare. We also acknowledge a number of people who helped advise, implement, and participate in this study. This includes University of Washington faculty Charlotte Sanders, MSW, Lisa Kelly, JD and Josephine Ensign, DrPH, MPH, FNP; Gemina Garland-Lewis for co-collaboration on parallel data collection; Amanda Richer for providing guidance and knowledge from the lived-experience perspective, as well as reviewing the manuscript for cultural sensitivity and to indicate bias; Richard Soiseth, Noah Weatherton, and Anna Humphreys who helped with the creation of materials, recruitment, and data collection; Tianai (Scyler) Li for transcription; and Chloe Lancaster for her research into the laws surrounding animal ownership.
Disclosure Statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Akinyemiju, T., & Moore, J. X. (2016). Data on burden of comorbidities in the United States and Medicaid expansion status. Data in Brief. https://doi.org/10.1016/j.dib.2016.05.019
- American Veterinary Medical Association. (n.d.). The human–animal interaction and human–animal bond. https://www.avma.org/policies/human-animal-interaction-and-human-animal-bond
- Arkow, P. (2020). Human–animal relationships and social work: Opportunities beyond the veterinary environment. Child and Adolescent Social Work Journal. https://doi.org/10.1007/s10560-020-00697-x
- Balk, G. (2013). In Seattle, it’s cats, dogs and kids—In that order. Seattle Times. https://www.seattletimes.com/seattle-news/data/in-seattle-its-cats-dogs-and-kids-in-that-order-2/
- Barcelos, A. M., Kargas, N., Maltby, J., Hall, S., & Mills, D. S. (2020). A framework for understanding how activities associated with dog ownership relate to human well-being. Scientific Reports. https://doi.org/10.1038/s41598-020-68446-9
- Bernard, H. R. (2017). Research methods in anthropology: Qualitative and quantitative approaches (6th ed.). Rowman & Littlefield.
- Braun, V., & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. Sage.
- Braun, V., Clarke, V., & Rance, N. (2014). How to use thematic analysis with interview data. In A. Vossler & N. Moller (Eds.), The counselling & psychotherapy research handbook (pp. 183–197). Sage.
- Brooks, H. L., Rushton, K., Lovell, K., Bee, P., Walker, L., Grant, L., & Rogers, A. (2018). The power of support from companion animals for people living with mental health problems: A systematic review and narrative synthesis of the evidence. BMC Psychiatry. https://doi.org/10.1186/s12888-018-1613-2
- Cleary, M., Visentin, D., Thapa, D. K., West, S., Raeburn, T., & Kornhaber, R. (2019). The homeless and their animal companions: An integrative review. Administration and Policy in Mental Health and Mental Health Services Research. https://doi.org/10.1007/s10488-019-00967-6
- Coakley, A. B., Annese, C. D., Hughes, E., & Flanagan, J. M. (2020). The experience of animal assisted therapy on patients in an acute care setting. Clinical Nursing Research. https://doi.org/10.1177/1054773820977198
- Cronley, C., Strand, E. B., Patterson, D. A., & Gwaltney, S. (2009). Homeless people who are animal caretakers: A comparative study. Psychological Reports. https://doi.org/10.2466/PR0.105.2.481-499
- Curl, A. L., Bibbo, J., & Johnson, R. A. (2017). Dog walking, the human–animal bond and older adults’ physical health. The Gerontologist. https://doi.org/10.1093/geront/gnw051
- Desai, R. A., Liu-Mares, W., Dausey, D. J., & Rosenheck, R. A. (2003). Suicidal ideation and suicide attempts in a sample of homeless people with mental illness. Journal of Nervous and Mental Disease. https://doi.org/10.1097/00005053-200306000-00003
- Edidin, J. P., Ganim, Z., Hunter, S. J., & Karnik, N. S. (2012). The mental and physical health of homeless youth: A literature review. Child Psychiatry and Human Development. https://doi.org/10.1007/s10578-011-0270-1
- Fazel, S., Geddes, J. R., & Kushel, M. (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. The Lancet. https://doi.org/10.1016/S0140-6736(14)61132-6
- Fletcher, A. (2017). Applying critical realism in qualitative research: Methodology meets method. International Journal of Social Research Methodology. https://doi.org/10.1080/13645579.2016.1144401
- Friedmann, E., & Krause-Parello, C. A. (2018). Companion animals and human health: Benefits, challenges, and the road ahead for human–animal interaction. Revue Scientifique et Technique (International Office of Epizootics). https://doi.org/10.20506/rst.37.1.2741
- Gan, G. Z. H., Hill, A. M., Yeung, P., Keesing, S., & Netto, J. N. (2020). Pet ownership and its influence on mental health in older adults. Aging and Mental Health. https://doi.org/10.1080/13607863.2019.1633620
- Gillespie, K., & Lawson, V. (2017). “My dog is my home”: Multispecies care and poverty politics in Los Angeles, California and Austin, Texas. Gender, Place and Culture. https://doi.org/10.1080/0966369X.2017.1339021
- Hawkins, R. D., Hawkins, E. L., & Tip, L. (2021). “I can’t give up when I have them to care for”: People’s experiences of pets and their mental health. Anthrozoös. https://doi.org/10.1080/08927936.2021.1914434
- Henry, M., Watt, R., Mahathey, A., Ouellette, J., & Sitler, A. (2020). The 2019 annual homeless assessment report (AHAR) to Congress. Part 1: Point-in-time estimates of homelessness. US Department of Housing and Urban Development.
- Henwood, B., Dzubur, E., Rhoades, H., St. Clair, P., & Cox, R. (2020). Pet ownership in the unsheltered homeless population in Los Angeles. Journal of Social Distress and Homelessness. https://doi.org/10.1080/10530789.2020.1795791
- Howe, L., & Easterbrook, M. J. (2018). The perceived costs and benefits of pet ownership for homeless people in the UK: Practical costs, psychological benefits and vulnerability. Journal of Poverty. https://doi.org/10.1080/10875549.2018.1460741
- Hudson, A. L., Nyamathi, A., Greengold, B., Slagle, A., Koniak-Griffin, D., Khalilifard, F., & Getzoff, D. (2010). Health-seeking challenges among homeless youth. Nursing Research. https://doi.org/10.1097/NNR.0b013e3181d1a8a9
- Irvine, L. (2013a). Animals as lifechangers and lifesavers: Pets in the redemption narratives of homeless people. Journal of Contemporary Ethnography. https://doi.org/10.1177/0891241612456550
- Irvine, L. (2013b). My dog always eats first: Homeless people and their animals. Lynne Rienner.
- Irvine, L., Kahl, K. N., & Smith, J. M. (2012). Confrontations and donations: Encounters between homeless pet owners and the public. Sociological Quarterly. https://doi.org/10.1111/j.1533-8525.2011.01224.x
- Johnson, A. L., Pride, D., Donahue, D. A., Stern, S. L., Hatch, J. P., Allison, S., & Lancaster, C. L. (2013). Potential benefits of canine companionship for military veterans with posttraumatic stress disorder (PTSD). Society & Animals. https://doi.org/10.1163/15685306-12341286
- Kerman, N., Gran-Ruaz, S., & Lem, M. (2019). Pet ownership and homelessness: A scoping review. Journal of Social Distress and the Homeless. https://doi.org/10.1080/10530789.2019.1650325
- Kerman, N., Lem, M., Witte, M., Kim, C., & Rhoades, H. (2020). A multilevel intervention framework for supporting people experiencing homelessness with pets. Animals. https://doi.org/10.3390/ani10101869
- King County Hospitals for a Healthier Community. (2020). King County community health needs assessment 2021/2022. https://kingcounty.gov/depts/health/data/community-health-indicators/~/media/depts/health/data/documents/2021-2022-Joint-CHNA-Report.ashx
- Lem, M., Coe, J. B., Haley, D. B., Stone, E., & O’Grady, W. (2016). The protective association between pet ownership and depression among street-involved youth: A cross-sectional study. Anthrozoös. https://doi.org/10.1080/08927936.2015.1082772
- Losinski, M., Katsiyannis, A., & Ryan, J. B. (2013). The McKinney-Vento education for homeless children and youth program: Implications for special educators. Intervention in School and Clinic. https://doi.org/10.1177/1053451213493170
- McNicholas, J., Gilbey, A., Rennie, A., Ahmedzai, S., Dono, J. A., & Ormerod, E. (2005). Pet ownership and human health: A brief review of evidence and issues. British Medical Journal. https://doi.org/10.1136/bmj.331.7527.1252
- Minter, S., & Daley, C. (2003). Trans realities: A legal needs assessment of San Francisco’s transgender communities (Report). National Center for Lesbian Rights and Transgender Law Center. https://www.nclrights.org/wp-content/uploads/2013/07/transrealities0803.pdf
- Morrison, D. S. (2009). Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. International Journal of Epidemiology. https://doi.org/10.1093/ije/dyp160
- Muñoz, M., Crespo, M., & Pérez-Santos, E. (2005). Homelessness effects on men’s and women’s health. International Journal of Mental Health. https://doi.org/10.1080/00207411.2005.11043400
- O’Haire, M. E., & Rodriguez, K. E. (2018). Preliminary efficacy of service dogs as a complementary treatment for posttraumatic stress disorder in military members and veterans. Journal of Consulting and Clinical Psychology. https://doi.org/10.1037/ccp0000267
- Pigott, D. M., Golding, N., Mylne, A., Huang, Z., Henry, A. J., Weiss, D. J., Brady, O. J., Kraemer, M. U., Smith, D. L., Moyes, C. L., Bhatt, S., Gething, P. W., Horby, P. W., Bogoch, I. I., Brownstein, J. S., Mekaru, S. R., Tatem, A. J., Khan, K., & Hay, S. I. (2014). Mapping the zoonotic niche of Ebola virus disease in Africa. Elife, 3, e04395. https://doi.org/10.7554/eLife.04395
- Public Health- Seattle & King County. (2021). Community health indicators. https://kingcounty.gov/depts/health/data/community-health-indicators.aspx
- R Core Team. (2019). R: A language and environment for statistical computing (R Foundation for Statistical Computing, Ed.).
- Rew, L. (2000). Friends and pets as companions: Strategies for coping with loneliness among homeless youth. Journal of Child and Adolescent Psychiatric Nursing, 13(3), 125–132. https://doi.org/10.1111/j.1744-6171.2000.tb00089.x
- Rhoades, H., Winetrobe, H., & Rice, E. (2015). Pet ownership among homeless youth: Associations with mental health, service utilization and housing status. Child Psychiatry and Human Development. https://doi.org/10.1007/s10578-014-0463-5
- Scanlon, L., Hobson-West, P., Cobb, K., McBride, A., & Stavisky, J. (2021a). Assessment of health and welfare in a small sample of dogs owned by people who are homeless. Veterinary Record. https://doi.org/10.1002/vetr.776
- Scanlon, L., Hobson-West, P., Cobb, K., McBride, A., & Stavisky, J. (2021b). Homeless people and their dogs: Exploring the nature and impact of the human–companion animal bond. Anthrozoös. https://doi.org/10.1080/08927936.2021.1878683
- Scanlon, L., McBride, A., & Stavisky, J. (2020). Prevalence of pet provision and reasons for including or excluding animals by homelessness accommodation services. Journal of Social Distress and Homelessness. https://doi.org/10.1080/10530789.2020.1754602
- Spicer, S. S. (2010). Healthcare needs of the transgender homeless population. Journal of Gay and Lesbian Mental Health. https://doi.org/10.1080/19359705.2010.505844
- Toylor, H., Williams, P., & Gray, D. (2004). Homelessness and dog ownership: An investigation into animal empathy, attachment, crime, drug use, health and public opinion. Anthrozoös. https://doi.org/10.2752/089279304785643230
- US Department of Housing and Urban Development. (2019). HUD’s definition of homelessness: Resources and guidance. HUD Exchange website: https://www.hudexchange.info/news/huds-definition-of-homelessness-resources-and-guidance/.
- Votta, E., & Manion, I. (2004). Suicide, high-risk behaviors, and coping style in homeless adolescent males’ adjustment. Journal of Adolescent Health. https://doi.org/10.1016/S1054-139X(03)00271-4
- Williams, D. L., & Hogg, S. (2016). The health and welfare of dogs belonging to homeless people. Pet Behaviour Science. https://doi.org/10.21071/pbs.v0i1.3998
- Wiltshire, G., & Ronkainen, N. (2021). A realist approach to thematic analysis: Making sense of qualitative data through experiential, inferential and dispositional themes. Journal of Critical Realism. https://doi.org/10.1080/14767430.2021.1894909
- Winslow, D., Van, T., Green, L., Donahue, L., Jain, V., Garcia, T. T., Seia, J., Zylstra, K., Salcedo, D., & Groce, D. (2020). Seattle/King County: Count us in 2020 – Point-in-time count of individuals experiencing homelessness. https://regionalhomelesssystem.org/wp-content/uploads/2020/07/Count-Us-In-2020-Final_7.29.2020.pdf
- Wurn, D. (2011). Seattle’s dog obsession. Seattle Magazine. https://seattlemag.com/article/seattles-dog-obsession
- Yarborough, B. J. H., Stumbo, S. P., Yarborough, M. T., Owen-Smith, A., & Green, C. A. (2018). Benefits and challenges of using service dogs for veterans with posttraumatic stress disorder. Psychiatric Rehabilitation Journal. https://doi.org/10.1037/prj0000294
- Zhang, P., Bassil, K., Gower, S., Katic, M., Kiss, A., Gogosis, E., & Hwang, S. W. (2019). Cold-related injuries in a cohort of homeless adults. Journal of Social Distress and the Homeless. https://doi.org/10.1080/10530789.2018.1523103