Abstract
Aim of the Study: During the reconstruction of alar defects involving the upper lip, reconstructive surgeons face the need for various thicknesses of tissues crucial to preserving the facial sulcus which is important for a cosmetically acceptable result. Our aim was to reconstruct the deep perialar and thinner lateral nasal alar defect in a single step procedure with a suitable flap which is reliable, has appropriate blood supply and provides an esthetically good result. Materials and Methods: Extended alar defect was reconstructed with a combined flap in 10 cases. During the procedure, a subcutaneous pedicle was created and the proximal part of the flap was rotated into the defect as a rotational flap. The procedure and the follow-up have been photo-documented in all cases. Furthermore, the perfusion of the flaps was monitored by means of laser Doppler flowmetry. Postoperative complications were evaluated with a semi-quantitative score and the patients completed a patient satisfaction questionnaire, too. Results: An optimal esthetic result was obtained in all cases after the operation. The lateral nasal alar part of the defect was reconstructed with the thinner proximal part of the flap while the deeper perialar region involving the upper lip was covered with the thicker distal part. The flaps have shown sufficient blood flow after the operation. There was no significant pin cushioning or “trap-door” effect in any case. Mild erythema and edema was found in few cases. The patients were satisfied with the cosmetic result of the intervention. Conclusions: The flap is suitable for the reconstruction of alar defects involving the perialar region. It has the advantage of covering the deeper perialar and the thinner alar defects, whilst eliminating the pin cushioning effect of the conventional subcutaneous island pedicle flaps.
INTRODUCTION
Skin malignancies often develop on the lateral nasal alar and adjacent regions [Citation1]. According to a recent study, 33% of nasal skin tumors affect the alar area [Citation2]. The remaining defect usually involves multiple cosmetic units, destroying the supra-alar, alar-facial groove, and the melolabial fold [Citation1]. Traditionally, the defined C- shaped perialar area includes the superior labial tissue, melolabial fold, medial cheek, and nasal tissue superior to the nasal alar crease [Citation3].
If the defect is localized to a single esthetic unit and side-to-side closure is not possible, owing to the size, V-Y advancement island pedicle flap is the most frequently chosen technique [Citation4]. It is an important principle that if the defect affects more than 50% of an esthetic subunit, the whole subunit is advised to be reconstructed with the excision of the remaining subunit [Citation2]. Maintenance of the natural curvatures and facial symmetry without impaired airflow are important factors when performing flap closure in the alar region [Citation2]. Defects localized to the nasal ala and C-shaped region usually require multiple combined flaps and further additional procedures (e.g. pedicle plasty in case of interpolational flap or correctional procedures to obtain optimal esthetic result). The present study introduces a variation of cutaneous-subcutaneous pedicled rotation-advancement flap for the reconstruction of the thin alar and adjacent deep perialar defects in a single step procedure with an appropriate cosmetic result.
MATERIALS AND METHODS
Patients
Ten patients were included in this study, mean age was 77 years (ranges from 66 to 84 years, 6 males, 4 females). Skin defect was localized to the alar region, the alar-facial groove, the upper lip and the cranial part of the nasolabial fold after the tumor was removed (). The extent of the defects following tumor excision ranged from 1.8 cm ×1.8 cm to 2.6 × 2.9 cm. Histological examination revealed basal cell carcinoma with tumor-free margins in all cases. Reconstruction was only performed once final histological result was obtained. This took 2–3 days, during which period a temporary coverage was used (Epigard, Biovision GmbH, Ilmenau, Germany). The mean follow-up was 7.5 months (ranges from 5 to 15 months). Prior to the intervention, all participants have given their informed consent in writing which granted the authors to use their photographs for scientific purpose.
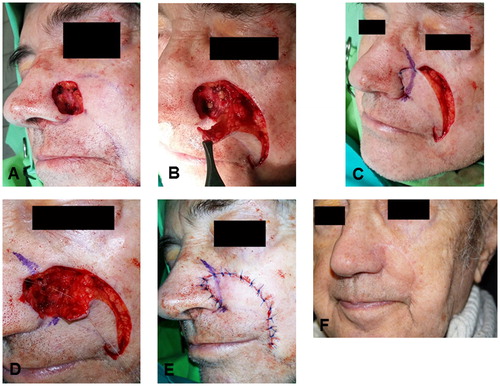
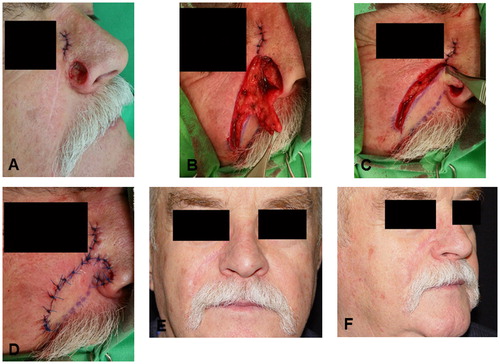
FIGURE 1. Different steps of the operation. A: preoperative status, B: dissection of the subcutaneous and cutaneous pedicled flap, C: temporarily situated flap, blue ink shows the position of alar-facial groove on the skin flap, D: alar-facial groove is fixed with 5/0 absorbable sutures, E: the flap is sutured into the defect, F: late postoperative status.
Surgical Procedures
Both the removal of the tumor and the reconstruction were performed under local anesthesia. The flap was designed by marking the nasolabial fold and a curved line from the distal-lateral part of the defect according to the relaxed skin tension lines. These lines matched in a distal point, marking the size and shape of the flap. Incision was performed on the lateral line, followed by subcutaneous tissue dissection and mobilization of the lateral wound edge, if necessary. It is important not to undermine the flap during the preparation and mobilization of the pedicle and to keep the perforator branches of the facial artery intact to preserve the vascular supply of the flap (). The cutaneous branches from the medial part and the subcutaneous perforator branches from the inferior part of the flap were hereby preserved. The flap was pulled to the cranial point of the defect. If necessary, a cut back was performed distally in the nasolabial fold so that the flap could be easily placed into the defect. Following temporary fixation of the proximal part a marking was performed on the flap according to the alar-facial groove (). The flap was thinned proximally from this marking. This part was used to cover the alar fragment of the defect. The prospective fold can be fixed to its base in the alar-facial groove with one or two 5/0 absorbable sutures if the flap is elevated (). Wound closure was performed with 5/0 absorbable and 5/0 permanent sutures (). Drainage or compression was not necessary. Scars were treated with silicone-ointment. Massage of the flap was advised after 4 weeks postoperatively (). demonstrate the steps of operation in three other patients.
FIGURE 2. Reconstruction in another patient. A: preoperative status, B: preparation of the flap, C: positioning of the flap, D: early postoperative status, E and F: late postoperative status.
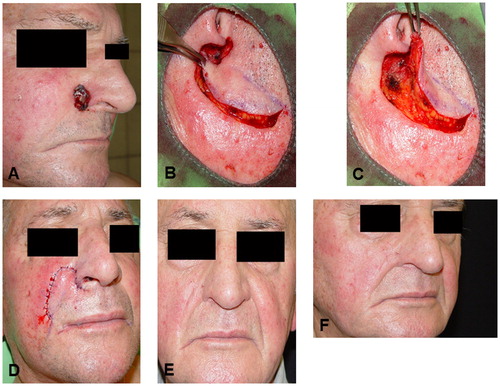
FIGURE 3. Application of the combined flap in a third patient. A: preoperative status, B: dissection of the flap, C: positioning of the flap, white arrow: the subcutaneous part of the flap via which perforators enter the flap, black arrow: direction of the cutaneous branches from the medial part of the flap, D: early postoperative status, E and F: late postoperative status.
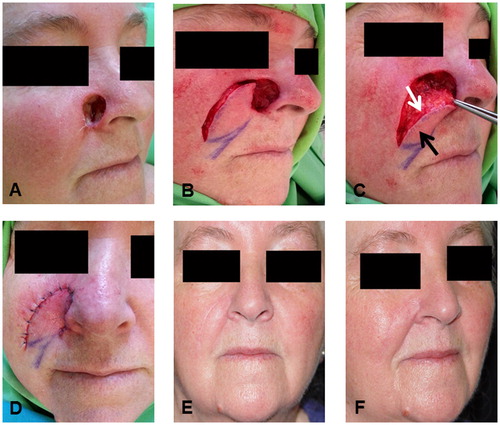
FIGURE 4. A further patient with the combined flap. A: preoperative status, B: preparation of the flap, C: positioning of the flap, D: early postoperative status, E and F: late postoperative status.
Patients were discharged on 2nd–3rd postoperative day. An examination was performed 10 days after the surgery, stitches were removed this time. The second examination was in the 3rd postoperative week. Following this, the patients were examined in each 3 months. During the postoperative period, different complications were monitored and evaluated as described below. If it was necessary, antibiotic therapy was launched which involved daily 1,000 mg cefuroxime (2 × 500 mg) administered orally.
Laser Doppler Flowmetry
Laser Doppler flowmetry was chosen for the determination of the microcirculation since it is an accepted and reliable method for this aim [Citation5]. Perfusion of the flaps was monitored by means of the PeriFlux System 5000 (Perimed, Järfälla, Sweden), as described in a previous study [Citation6]. The sensor was fixed to the tissue with a sterile adhesive strip provided by the manufacturer. Measurements were performed at five different time points: before the incision (baseline), after preparation of the flap, after fixation of the flap, 1 day after surgery and 3 weeks after surgery. At each time point, recordings were made for 5 minutes. Perisoft for Windows software was used for data collection, storage and analysis. The data are presented as perfusion unit (P.U.).
Evaluation of Complications
The following signs and aspects were monitored: edema, erythema, hematoma, trap-door deformity and need for resuturing/reoperation (). Complications were evaluated with a semi quantitative scoring system. Briefly, 0: the given sign is not present; 1, 2, 3: mild, moderate, and severe manifestation of the given sign, respectively.
TABLE 1. Frequency and severity of the postoperative complications
Patient Satisfaction
Each patient was asked to complete a patient satisfaction questionnaire in the 6th postoperative month. Eight questions were given concerning the postoperative pain and the satisfaction with the results of the intervention (Table 2). Patients were asked to rate the pain on a 10-point scale: no pain (=0), unbearable pain (=10) while a 5-point Likert scale was suggested for the other questions: very satisfied (=5), relatively satisfied (=4), fairly satisfied (=3), relatively dissatisfied (=2), and very dissatisfied (=1).
Statistical Analysis
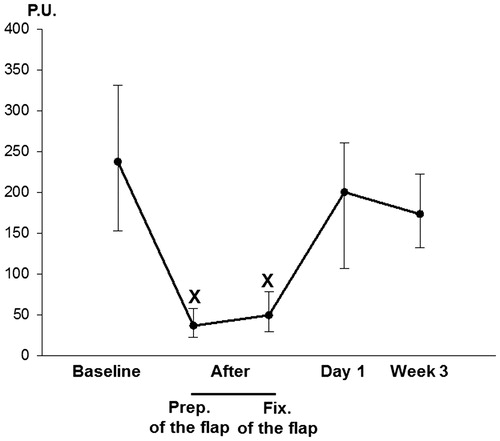
Data analysis was performed with SigmaStat for Windows (Jandel Scientific, Erkrath, Germany). Friedman repeated measures analysis of variance on ranks was applied for the evaluation of the data obtained from laser Doppler flowmetry. Time-dependent differences from the baseline were assessed by Dunn’s method. In , median values (M) with the 25th and 75th percentiles (25p and 75p, respectively) are given, p < .05 was considered statistically significant. Scores describing the complications and patient satisfaction are presented as mean values (m) and standard deviation (SD).
RESULTS
The authors performed a combined cutaneous and subcutaneous pedicled rotation-advancement skin flap, contrary to the widely applied subcutaneous island pedicle flap. With this method, there is no (or short) incision in the nasolabial fold. This preserves the vascular supply better and provides more preferable cosmetic results with fewer scars.
As concerns perfusion of the flaps, laser Doppler flowmetry has revealed a significant decrease in the blood flow after preparation of the flap (M = 36.57 P.U., 25p = 22.02, 75p = 58.03) and fixation of the flap (M = 49.49 P.U., 25p = 29.1, 75p = 77.99) as compared to the baseline (M = 237.59 P.U., 25p = 152.89, 75p = 331.2). However, microcirculation has shown a considerable improvement during the 1st postoperative day. Day 1 perfusion values (M = 200.32 P.U., 25p = 106.34, 75p = 260.59) did not differ significantly from baseline. Sufficient blood flow was observed in the later period, as well. Week 3 values (M = 173.39 P.U., 25p = 132.59, 75p = 222.94) did not display significant difference as compared to the baseline ().
Mild edema was noticeable in three cases during the 2nd-8th postoperative weeks (score: m = 0.3; SD =0.48) that was resolved with scar treatment and massage of the flap. In two cases, mild erythema was observed (score: m = 0.2; SD =0.42) which ceased after the antibiotic therapy. Mild trap-door deformity was found in one case (score: m = 0.1; SD =0.32). Hematoma was not observed and none of the patients required reoperation/resuturing (). The 6-month postoperative cosmetic result was outstanding. There were no further complications or need for additional correction ().
Table 2 summarizes the findings of the patient satisfaction survey. The majority of the patients reported only mild or moderate postoperative pain. They were also satisfied with the esthetic and the functional results of the intervention. Moreover, they have received positive feedback from other people.
DISCUSSION
The reconstruction of nasal soft tissue defects localized to multiple esthetic subunits is a challenging task for plastic surgeons. The combined reconstruction of alar and perialar regions is difficult. The alar region has a rigid structure and low mobility, while the perialar soft tissues are different. Preserving the natural alar contours and concavities of the alar crease also keeping the respiratory function and symmetry with the contralateral side is important [Citation2]. There are various reconstructive techniques available that can be used in this region, including direct closure, skin grafts, local flaps, regional pedicled flaps or combinations of these [Citation7]. Direct closure is only preferable in case of small defects, because it can easily cause alar rim distortion. Skin grafts may result in depressed scars and impaired nasal valve patency when used to repair deeper alar defects [Citation8]. Almost all local and regional flaps have significant drawbacks. The single staged nasolabial transposition flap results in a deformed alar groove thus producing an obvious asymmetry with the contralateral side [Citation7]. The conventional subcutaneous pedicled island flaps may also lead to distortion and more frequently pin-cushioning or trapdoor effect due to the all-round incision of the flap [Citation4,Citation9]. The combination of these procedures or multiple correctional surgeries can also be laborious and costly.
Our aim was to find a one-step intervention which fulfills all the above mentioned requirements with the least complications. The blood supply of our flap is dual. It can be considered as the combination of the unipedicle melolabial advancement flap and the melolabial island advancement flap described by Baker [Citation10]. Contrary to the above mentioned ones, our flap receives blood supply from two different directions. On the one part, cutaneous vessels enter the flap from the area of the nasolabial fold (because the flap is not incised medially). Furthermore, the flap is not undermined (except the cranial part) therefore it has subcutaneous perforators, as well.
For the better mobilization, cutback can be performed hereby making a hatchet flap, however it is not necessary in most cases. This technique allows the reconstruction of alar and perialar defects localized to more esthetic subunits. As concerns preparation of the flap, two different movements shall be performed. The flap is first moved to the inferior part of alar rim like an advancement flap. This is the pivot point around which the cranially thinned flap is rotated into the remaining part of the defect.
Regarding the results of the follow-up, there were no partial or complete flap losses. This may originate in the above mentioned advantageous blood supply which involves both cutaneous branches and subcutaneous perforators. Although surgical intervention itself may lead to a decrease in capillary flow during the early postoperative period, this parameter shows regeneration then [Citation11]. Neither hematoma, nor recurrence of the tumor was observable. Although in two cases sign of infection was detected, this may originate in the age and the comorbidities of the patients. Symmetry with the opposite side remained intact with no significant distortion or disfiguring of facial folds or creases. Large defects may be accompanied with the risk of temporary or permanent distortion of upper lip and melolabial fold. The biggest defect in our study was 2.6 × 2.9 cm which has not led to such problem. However, each case shall be judged individually, and our elderly patients possess a skin laxity which may facilitate the procedure. However, a slight edema of the flap was seen in some cases but this resolved with scar treatment and massage of the flap by the end of the 8th postoperative week. Mild trap-door deformity was found in one case and there was no need for a second operation in any of the cases. Furthermore, the patients were satisfied with the results of the intervention.
Planning of the flap is easy and with cautious dissection and trimming of the cranial part of the flap, the vascular supply can be fully preserved. Our study involves mainly elderly patients since extended basal cell carcinoma is rare in younger patients. Elder skin may differ from that of younger patients in terms of laxity and microcirculation. Lax skin may facilitate positioning of the flap. Microcirculation often displays impairment with the age, but we have found good postoperative regeneration of blood flow and optimal flap survival. Nevertheless, our future aim is to increase the number of cases in order to gain more reliable data on this technique.
In conclusion, our flap design provides the benefits of the combined vascular supply of subcutaneous and cutaneous pedicled flaps without the disadvantages of all-round incisions causing trapdoor deformities. It is suitable for the reconstruction of both deeper perialar and thinner alar defects with appropriate cosmetic result.
DECLARATION OF INTEREST
The authors report no conflict of interest. The authors are alone responsible for the content and writing of the paper.
TABLE 2. Patient satisfaction
REFERENCES
- Cvancara JL, Wentzell JM. Shark island pedicle flap for repair of combined nasal ala-perialar defects. Dermatol Surg. 2006;32(5):726–729.
- Padoveze EH, Cernea SS. Reconstruction of nasal defects after tumor excision through Mohs micrographic surgery. Surg Cosmet Dermatol. 2013;5(2):116–120.
- Levasseur JG, Mellette JR, Jr. Techniques for reconstruction of perialar and perialar-nasal ala combined defects. Dermatol Surg. 2000;26(11):1019–1023.
- Li JH, Xing X, Liu HY, Li P, Xu J. Subcutaneous island pedicle flap: variations and versatility for facial reconstruction. Ann Plast Surg. 2006;57(3):255–259. doi:10.1097/01.sap.0000221639.76906.3a.
- Swiontkowski MF. Laser Doppler flowmetry – development and clinical application. Iowa Orthop J. 1991;11:119–126.
- Varga J, Mohos G, Varga Á, et al. A possible technique for the complex reconstruction of exposed breast implant: applicability and microcirculation of the capsule flap. J Invest Surg. 2018:1. doi:10.1080/08941939.2018.
- Tregaskiss A, Allan J, Gore S, Aldred R. Use of nasal sidewall island inversion flap for single-stage ala nasi reconstruction: a report of 103 consecutive cages. Plast Reconstr Surg. 2014;133(2):377–385. doi:10.1097/01.prs.0000436797.81928.24.
- Pipitone MA, Gloster HM. Jr., Repair of the alar groove with combination partial primary closure and second-intention healing. Dermatol Surg. 2005;31(5):608–609.
- Szolnoky G, Mohos G, Dobozy A, Kemény L. Manual lymph drainage reduces trapdoor effect in subcutaneous island pedicle flaps. Int J Dermatol. 2006; 45(12):1468–1470. doi:10.1111/j.1365-4632.2006.03165.x.
- Baker SR. Melolabial flaps. In: Baker SR (ed). Local flaps in facial reconstruction. 2nd ed. Edinburgh: Elsevier Mosby; 2007: 231–264.
- Figus A, Mosahebi A, Ramakrishnan V. Microcirculation in DIEP flaps: a study of the haemodynamics using laser Doppler flowmetry and lightguide reflectance spectrophotometry. J Plast Reconstr Aesthet Surg. 2006; 59(6):604–612.