Abstract
Introduction
Low-grade appendiceal mucinous neoplasm (LAMN) is a rare disorder. There is no consensus on the prognosis and management of LAMN.
Materials and methods
We reviewed 51 consecutive patients with LAMN from 2013 to 2018. We divided our patients into two groups. The first is patients with an intact appendix. The second group comprises patients with the potential to develop a malignant condition. Comparisons of serum tumor markers between two groups were performed. Survival curves were estimated. Univariate and multivariate Cox proportional hazards were computed for 46 patients with median follow-up of 2.7 years.
Results
Comparison of patients in two groups revealed significant differences in the mean level and abnormal ratio of CA125 (p < 0.001, p < 0.001), CA19-9 (p = 0.04, p = 0.04), and CEA (p = 0.001, p = 0.02). Eight patients had relapsed by the last follow-up in the second group. Patients with normal CEA had significantly longer disease-free survival (DFS) time than those with abnormal CEA (p = 0.04). CA19-9 exhibited a significant association with DFS (HR = 5.72, p = 0.02) in the Univariate Cox proportional hazards.
Discussion
The prognosis of LAMN is related to serum tumor markers, the surgical procedure and the pathology.
Introduction
According to the Peritoneal Surface Oncology Group International (PSOGI) classification from 2015, epithelial neoplasia of the appendix is classified into low-grade appendiceal mucinous neoplasm, high-grade appendiceal mucinous neoplasm, serrated polyp, adenoma, adenocarcinoma, mucinous adenocarcinoma, and poorly differentiated adenocarcinoma with signet ring cells [Citation1]. The concept of low-grade appendiceal mucinous neoplasm (LAMN) is consistent with the recent edition of the World Health Organization (WHO) classification, with a benign morphologic appearance and aggressive biological potential [Citation2]. The appearance of LAMN is commonly an appendiceal mucocele, which is characterized by the large amount of mucoid matter in the appendix lumen. The reoccurrence of LAMN is very rare with intact removal of a mucocele. However, the potential to develop a malignant condition is increased in patients with positive margin; appendiceal rupture; mucin, cells, or both outside the appendix; or pseudomyxoma peritonei (PMP) [Citation3–6]. PMP is the most malignant condition in these situations with a high relapse rate [Citation1]. LAMN is a precursor lesion for PMP. Appendiceal mucocele might rupture and disseminate throughout the abdominal cavity spontaneously or by accident. [Citation7]. Nevertheless, PMP could only be diagnosed via the spread of cells and mucin beyond the right lower quadrant of the abdomen [Citation8]. To perform better surveillance of patients with LAMN with the potential to develop a malignant condition, many investigations have been performed. Relapse rates are evaluated in patients [Citation3–6]. It also raises our interest in focusing on these patients. There is no consensus regarding surgical treatment for LAMN. A single appendectomy is sufficient for patients with a tumor only in the appendix [Citation2]. Right-sided hemicolectomy and caecectomy are recommended by some authors when the tumors extend to the peri-appendiceal area [Citation6,Citation9]. Right-sided hemicolectomy and other surgical procedures exhibit no evidence of having a better prognosis than appendectomy in patients with LAMN [Citation10]. Regarding patients with PMP, cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) are regarded as standard treatments [Citation11].
The aim of this study is to demonstrate the characteristics of LAMN and the prognosis of patients with the potential to develop a malignant condition, including patients with positive margin; spontaneously appendiceal rupture; mucin, cells, or both outside the appendix; or PMP.
Materials and methods
The Institutional Review Board (IRB) in our hospital has reviewed our protocol and has determined that 1) the applicant(s) are qualified to conduct the proposed study; 2) the design of the study is rationale and scientifically sound; 3) human subject protection is adequate. In compliance with the Declaration of Helsinki, the IRB approve our protocol. We performed a retrospective observational study with the 51 patients diagnosed with LAMN according to the pathology of resected specimens and treated in our hospital, which are consecutive cases from November 2013 to June 2018. We used SPSS version 22.0 (SPSS, Inc., Chicago, IL, USA) for statistical analyses.
Study subjects
Patients diagnosed with LAMN according to the PSOGI classification between November 2013 and June 2018 were included in this retrospective cohort study. The patients were diagnosed via histology and immunohistochemistry of the excised appendix and other organs in the pelvic area and abdomen after operation performed by an experienced gastrointestinal pathologist. Demographic data, clinical data, results of a physical examination, imaging characteristics, the current status, and relapse rate were assessed for all patients. Patients with an intact appendix were discovered to have a macroscopic intact and dilated appendix during laparoscopic exploration, and the appendix was removed and the margin confirmed to be negative by pathologist. In the patients with the potential to develop a malignant condition, appearance of positive margin; appendiceal rupture/perforation; mucin, cells, or both outside the appendix; or PMP were confirmed by histology and immunohistochemistry. These patients underwent appendectomy, appendectomy and ileocecectomy, or CRS including hysterectomy plus bilateral salphingo-oophorectomy and omentectomy, according to the situation during surgery. In patients confirmed to have PMP, HIPEC were performed during follow-up.
Serum tumor marker
Serum tumor markers were obtained before surgery. Serum tumor markers including AFP, CA242, CA72-4, CA15-3, CA125, CA19-9, and CEA were measured in 41 patients and were categorized as normal or abnormal (AFP < 20 vs ≥20 ng/ml, CA242 < 20 vs ≥20 U/ml, CA72-4 < 9.8 vs ≥9.8 U/ml, CA15-3 < 25 vs ≥25 U/ml, CA125 < 35 vs ≥35 U/ml, CA19-9 < 37 vs ≥37 U/ml, CEA < 5 vs ≥5 ng/ml). Patients measured with CA125, CA19-9, and CEA were divided into two groups, patients with the potential to develop a malignant condition and patients with an intact appendix. Comparisons of patient demographics were performed using the Mann-Whitney U test and Fisher’s exact test. p < 0.050 was considered statistically significant.
Imaging
Available ultrasound and computed tomography (CT) images were reviewed by radiologists.
Prognosis
In 18 patients believed to have higher potential to develop a malignant condition, relapse rates were evaluated. Overall survival (OS) was defined as the number of years between the date of diagnosis and the date of death. Patients who were alive at the last follow-up are censored at the date of last follow-up. Disease-free survival (DFS) was defined as the number of years between the date of diagnosis and the date of disease recurrence or death, whichever occurred first. Patients who were alive, with or without disease recurrence, are censored at the date of last follow-up. Survival curves were estimated using the Kaplan-Meier methods. Univariate and multivariate Cox proportional hazards were performed to evaluate the relationship between patient clinical characteristics and DFS. Patient clinical characteristics that were significant with p < 0.2 in the univariate model were included in the multivariate. Other clinical characteristics supposed to be relevant to DFS were also included. Forward elimination was implemented when all indicators had p < 0.05.
Results
Clinical characters of the 51 patients
A total of 51 patients (45 women and 6 men) were diagnosed with LAMN according to the pathology of the excised appendix after the surgery, shown in . Most of the patients were women (88%). Eighteen patients (35%) were diagnosed with the potential to develop a malignant condition based on pathology after operation. Clinical features on presentation included abdominal pain (16,31%), abdominal mass (8,16%), haematochezia (2,4%), and abdominal distention (11,22%). Fourteen patients (27%) exhibited no clinical presentation. The physical examinations revealed tenderness and rebound pain similar to acute appendicitis (3,6%) and tenderness pain without rebound pain (4,8%). Eight patients (16%) exhibited recurrence, all of which were patients with the potential to develop a malignant condition. Twenty patients (39%) were diagnosed with appendiceal mucocele before operation. Three patients (6%) were diagnosed with appendicitis before operation and were discovered with an intact and dilated appendix during operation. As for 18 patients (36%) diagnosed with adnexal mass or undefined mass in pelvic area before operation, 17 patients were discovered with dilated appendix (12 macroscopic intact; 5 not intact) instead of adnexal mass during operation. One patient was discovered with a mass on left ovary during operation. The mass was resected, which was suspected to be mucinous tumor originated from appendix by intraoperative frozen pathology. CRS involving hysterectomy plus bilateral salphingo-oophorectomy, mentectomy was then performed. As for 10 patients (20%) diagnosed with ovarian cancer with metastasis before operation, 4 patients were discovered with perforated appendix and adnexal mass. These 4 patients were suspected to have appendiceal mucinous tumor by intraoperative frozen pathology during operation based on the removed appendix. The other 6 patients’ intraoperative frozen pathology were based on removed adnexal mass (no appendix involved). Two of the six patients were suspected to have muscinous tumors originated from appendix. Four of the six patients were suspected to have muscinous tumors with unknown origin. CRS involving hysterectomy plus bilateral salphingo-oophorectomy, mentectomy was then performed in the 10 patients diagnosed with ovarian cancer with metastasis before operation. In total, 15 patients (29%) underwent a single appendectomy and did not experience recurrence. One patient (2%) underwent right hemicolectomy and 23 (45%) patients underwent appendectomy and ileocecoectomy without recurrence. Twelve patients (24%) underwent CRS.
Table 1. Clinical characteristics of 51 LAMN patients.
Clinical characteristics of the patients with an intact appendix and the patients with the potential to develop a malignant condition were summarized in . In 33 patients with an intact appendix, 1 patient (3%) underwent right hemicolectomy. Fourteen patients (42%) underwent appendectomy and 18 patients (55%) underwent appendectomy and ileoceoectomy. There was no additional treatment after surgery. CT and serum tumor marker were performed every 6 months. Until recent follow-up, all 33 patients (100%) were alive with no diseases.
Table 2. Clinical characteristics of patients with an intact appendix and patients with the potential to develop a malignant condition.
As for 18 patients with the potential to develop a malignant condition, In accordance with the pathology of the resected organs, collected mucin and cells in peritoneal cavity, 3 patients (17%) were diagnosed with mucin, cells, or both outside the appendix, with no extension beyond right lower quadrant. Two of these three patients underwent CRS involving hysterectomy plus bilateral salphingo-oophorectomy, mentectomy. One of these three patients underwent appendectomy and ileocecoectomy. There was no additional treatment for all 3 patients after surgery and they were alive with no disease until recent follow-up. Four patients (22%) were diagnosed with appendiceal rupture or perforation. One of these four patients underwent appendectomy. Three of these four patients underwent appendectomy and ileocecoectomy. There was no additional treatment for 4 patients after surgery and they were alive with no disease until recent follow-up. One patient (7%) was diagnosed with positive margin. Appendectomy and ileocecoectomy was performed. The patient received no additional treatment and was alive with no disease until recent follow-up. Ten patients (55.6%) were diagnosed with PMP. All 10 patients underwent CRS involving hysterectomy plus bilateral salphingo-oophorectomy, mentectomy. All 10 patients received HIPEC after surgery. Until recent follow-up, 6 patients were alive with disease. One patient was dead. Contact was lost with 1 patient, but the patient was confirmed to have experienced recurrence 1 year after surgery. Two patients were alive with no diseases.
Serum tumor marker
The comparison of patients with the potential to develop a malignant condition and patients with an intact appendix is shown in . The mean serum CA125 level of 14 patients found to have the potential to develop a malignant condition is greater than that of 17 patients observed to have an intact appendix, 90.7 (66.3–115.1 U/ml) versus 12.2 (10.7–13.8 U/ml) (p < 0.001). The ratio of abnormal levels of CA125 in patients found to have the potential to develop a malignant condition is also greater than that of patients observed to have an intact appendix, 86% versus 0% (p < 0.001). The mean serum CA19-9 level of 15 patients found to have the potential to develop a malignant condition is greater than that of 23 patients observed to have an intact appendix, 59.0 (33.2–84.9 U/ml) versus 16.6 (12.3–20.8 U/ml) (p = 0.04). The ratio of abnormal levels of CA19-9 in patients found to have the potential to develop a malignant condition is also greater than that of patients observed to have an intact appendix, 40% versus 9% (p = 0.04). The mean serum CEA level of 14 patients found with the potential to develop a malignant condition is greater than that of 22 patients observed to have an intact appendix, 59.0 (43.2–74.8 ng/ml) versus 4.8 (3.4–6.1 ng/ml) (p = 0.001). The ratio of abnormal levels of CEA in patients found to have the potential to develop a malignant condition is also greater than that of patients observed with an intact appendix, 64% versus 23% (p = 0.02).
Table 3. Comparison of serum tumor marker levels between patients with the potential to develop a malignant condition and patients with an intact appendix.
Imaging
Ultrasound imaging was available for 34 patients. Two of 34 (6%) patients had been diagnosed with appendiceal mucocele before surgery. Twelve of 34 (35%) patients were considered to have an adnexal mass before surgery. More intriguingly, 4 of these 12 patients were found to exhibit mucin, cells or both outside appendix; or a ruptured appendix after surgery, whereas 8 of these 12 patients were confirmed to have an intact appendix. The rest of the 20 patients (59%) were observed to have masses in the right lower abdomen, pelvic cavity, right iliac fossa, or close to the uterus.
CT imaging was available for 29 patients. Twelve of 29 (41%) patients had been diagnosed with appendiceal mucocele before surgery. Four of 29 patients (14%) were considered to have an adnexal mass before surgery. All of these 4 patients were confirmed to exhibit mucin, cells or both outside appendix. The rest of the 13 patients (45%) were observed to have masses in the right lower abdomen, pelvic cavity, right iliac fossa, or close to cecum.
Prognosis
There was no occurrence of relapse or death in patients with an intact appendix. Eight of 18 (44%) patients with potential to develop a malignant condition relapsed by the last follow-up. One (6%) patient died. Contact was lost with 1 (6%) by the last follow-up, but the patient was confirmed to have experienced recurrence 1 year after surgery. Serum CA125 is available for 14 patients. CA19-9 is available for 15 patients. CEA is available for 14 patients. The relapse rate of patients with abnormal serum CA125 is greater than that of patients with normal serum CA125 (67% versus 0% (p = 0.165)). The relapse rate of patients with abnormal serum CA19-9 is greater than that of patients with normal serum CA19-9 (67% versus 33% (p = 0.315)). The relapse rate of patients with abnormal serum CEA is significantly greater than that of patients with normal serum CEA (67% versus 0% (p = 0.03)).
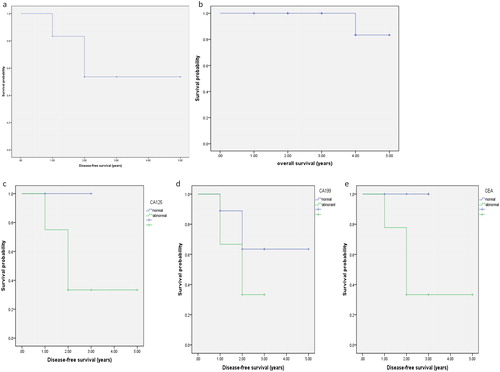
The Kaplan-Meier estimates of OS and DFS are shown in . The median follow-up time of 18 patients with the potential to develop a malignant condition was 2.9 years (SE = 1.2 years). The median DFS time was 3.4 years (SE = 0.4 years). The median overall survival time was 4.8 years (SE = 0.2 years). The median DFS time of patients with abnormal CA125 was 2 years (SE = 0.3), whereas there was no recurrence in patients with normal CA125. The median DFS time of patients with abnormal CA19-9 is 2 years (SE = 0.3), whereas the median DFS time of patients with normal CA19-9 is 3.8 years (SE = 0.6). The median DFS time of patients with abnormal CEA is 2 years (SE = 0.4), whereas there was no recurrence in patients with normal CEA. The median DFS time of patients with normal CEA was significantly longer than patients with abnormal CEA (p = 0.04).
Figure 1. OS and DFS of patients with metastasis to other organs or a ruptured appendix.
OS, overall survival; DFS, disease free survival. The Kaplan-Meier estimates of OS and DFS are shown in a and b. The Kaplan-Meier estimates of DFS by CA125, CA19-9 and CEA level are given in c, d and e.
There was no recurrence in patients with no potential to develop a malignant condition. Five patients underwent a surgery within one year, and no recurrence was reported. The univariate Cox proportional hazards model for DFS of the remaining 46 patients with median follow-up of 2.7 years is reported in . CA19-9 was the only indicator that exhibits a significant association with DFS (HR = 5.72, p = 0.02). The multivariate Cox proportional model exhibits no significance. All of the 8 patients with recurrence were diagnosed with PMP, abnormal CA125 and CEA. All 8 patients underwent cytoreductive procedure including hysterectomy plus bilateral salphingo-oophorectomy, ileocecoectomy, omentectomy, and HIPEC in the later follow-up.
Table 4. Univariate Cox proportional hazards model for the DFS of 46 patients.
Discussion
Most of patients in our study were women (88%), which is consistent with the results of former study that appendiceal mucocele was observed predominantly in women, with a female-to-male ratio of 4/1 [Citation12]. We also discovered that 27% of patients exhibited no clinical presentation before surgery. In these patients with no clinical presentation, LAMN was accidently discovered via transvaginal ultrasound during annual routine medical examination, which is performed exclusively on women. We think that this routine examination might cause the extremely high ratio of female patients in our study. Although it is reported that half of the patients are asymptomatic [Citation12,Citation13], our study reveals that clinical features on presentation included abdominal pain, abdominal distention, abdominal mass and hematochezia. A number of Appendiceal mucocele patients were misdiagnosed as acute appendicitis [Citation14,Citation15]. However, only 3 of 51 patients in our study was found to have tenderness and rebound pain typical of acute appendicitis.
The preoperative diagnosis of LAMN is challenging. Appendiceal mucocele was only diagnosed in 39% patients in our study. It is difficult to distinguish appendiceal mucinous tumors from ovarian tumors because of the close location, the nonspecific serum tumor markers, and the fact that appendiceal mucinous tumors always metastasize to ovaries mimicking ovarian tumors, which is consistent with a recent study [Citation16]. Besides, ovarian tumors are more common than appendiceal mucinous tumors, increasing the challenge of diagnosing LAMN. Even though the preoperative diagnosis of LAMN is hard, the laparoscopic exploration of appendix and intraoperative frozen pathology of appendix during operation could discover the pathologic changes of appendix in most cases. In cases when appendix was not removed for intraoperative frozen pathology, the correct diagnosis during operation is affected. In our study, 2 of 6 patients were suspected to have mucinous tumors originated from appendix, while 4 of 6 patients were suspected to have mucinous tumors with unknown origin. In both situations, CRS should be performed to avoid the worst scenario (PMP) [Citation17]. Additional treatment involving HIEPC should be applied when patients are diagnosed with PMP after operation.
Serum tumor markers including CA125, CA19-9 and CEA have been reported to have diagnostic and prognostic value for patients with mucinous neoplasms [Citation12,Citation18]. In our study, serum tumor markers were obtained before surgery. We compared the serum tumor markers of patients with the potential to develop a malignant condition with those of patients confirmed to have an intact appendix. The mean serum levels of CA125, CA19-9, and CEA are significantly higher in patients with the potential to develop a malignant condition. Some of the patients confirmed to have PMP by pathology had extremely high levels of serum tumor markers. To exclude the excursion, we compared the abnormal ratio between two groups, which was also significantly different. We believe that ruptured appendix; mucin, cells, or both outside the appendix; positive margin; or PMP lead to increased serum tumor markers, which are also closely related to prognosis.
The typical appearance of appendiceal mucocele in ultrasound images is that of an “onion skin” [Citation19]. Visualization of the appendix revealing the diameter of the appendix exceeding 15 mm are considered to be a specific appendiceal mucocele index [Citation20,Citation21]. In CT, a well-capsulated cystic formation with calcificates in the wall is visualized [Citation22,Citation23]. Another indicator is the presence of appendiceal lumen exceeding 13 mm [Citation24]. In our study, CT exhibited a higher accuracy of diagnosing patients with masses in the appendix before surgery than ultrasound. Appendiceal mucocele is always misdiagnosed with adnexal mass by imaging [Citation25,Citation26]. Eight of 12 patients considered as having an adnexal mass when diagnosed via ultrasound before surgery were confirmed to have an intact appendix with no mucins or cells in the pelvic cavity and no metastasis to adnexal mass. Meanwhile, all patients considered to have an adnexal mass according to the CT imaging were confirmed to exhibit metastasis to adnexal mass after surgery. CT seems to be a better method to avoid misdiagnosis of adnexal mass compared with ultrasound.
In 18 patients diagnosed with the potential to develop a malignant condition, patients with abnormal levels of serum CA125, CA19-9 or CEA had a higher relapse rate compared to those with normal levels of serum CA125, CA19-9 or CEA. The difference in relapse rate is only significant when comparing patients with normal serum CEA and patients with abnormal serum CEA, probably due to the small sample. The Kaplan-Meier estimates of DFS indicated that patients with normal CEA had significantly longer DFS time compared to those with abnormal CEA. There was no significant difference in DFS time comparing patients with abnormal and normal CA19-9 or CA125, but patients with normal CA19-9 or CA125 showed longer DFS time.
The univariate Cox proportional hazards model for DFS of 46 patients with a median follow-up of 2.7 years revealed that CA19-9 was the only indicator exhibiting a significant association with DFS (HR = 5.72, p = 0.02). Moreover, all patients with recurrence had abnormal serum level of CA125 and CEA. It is believed that LAMN patients with positive margin; appendiceal rupture/perforation; or mucin, cells, or both outside the appendix might develop a malignant condition. All 8 patients with recurrence were diagnosed with PMP instead of the situation listed above. Fifteen patients that underwent a single appendectomy did not experience recurrence. Even though 1 of 15 patients was believed to present appendix perforation/rupture, single appendectomies are mostly performed on patients with no potential to develop a malignant condition in our study, which is believed to have a better prognosis. We cannot conclude that single appendectomy can reduce the risk of relapse, but single appendectomy is probably sufficient when treating patients with an intact appendix. No additional treatment is required for patients without PMP if the correct surgical procedure is selected and well performed. As a result, we believe that CA125, CA19-9, and CEA are good indicators for patients’ prognosis. LAMN patients with positive margin; appendiceal rupture/perforation; or mucin, cells, or both outside the appendix are less likely to result in a malignant condition compared to PMP. We cannot decide whether single appendectomy is sufficient for patients with an intact appendix, but CRS and HIPEC must be performed on PMP patients to reduce the relapse rate.
In this study, only 51 LAMN patients from a single center were retrospectively included. More studies are needed to obtain a better understanding of the pathophysiology of LAMN.
Conclusion
In summary, we reviewed the clinical data of 51 LAMN patients treated in our hospital. To avoid misdiagnosis and obtain a better understanding of the prognosis, serum tumor marker, especially CA125, CA19-9 and CEA, must be tested before surgery. Moreover, CT is a better imaging approach for diagnosis than ultrasound. Furthermore, baseline CA125, CA19-9, and CEA are important prognostic factors to predict patients’ prognosis. Our study provides a better perspective regarding diagnosing LAMN and avoiding its relapse.
Disclosure statement
This is no financial interest or benefit that has arisen from the direct applications of our research.
References
- Carr NJ, Cecil TD, Mohamed F, et al. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am J Surg Pathol. 2016;40(1):14–26. doi:10.1097/PAS.0000000000000535.
- Misdraji J. Mucinous epithelial neoplasms of the appendix and pseudomyxoma peritonei. Mod Pathol. 2015;28(S1):S67–S79. doi:10.1038/modpathol.2014.129.
- Li X, Zhou J, Dong M, et al. Management and prognosis of low-grade appendiceal mucinous neoplasms: a clinicopathologic analysis of 50 cases. Eur J Surg Oncol. 2018;44(10):1640–1645. doi:10.1016/j.ejso.2018.06.037.
- Guaglio M, Sinukumar S, Kusamura S, et al. Clinical surveillance after macroscopically complete surgery for Low-Grade Appendiceal Mucinous Neoplasms (LAMN) with or without limited peritoneal spread: long-term results in a prospective series. Ann Surg Oncol. 2018;25(4):878–884. doi:10.1245/s10434-017-6305-5.
- Tiselius C, Kindler C, Shetye J, et al. Computed tomography follow-up assessment of patients with low-grade appendiceal mucinous neoplasms: evaluation of risk for pseudomyxoma peritonei. Ann Surg Oncol. 2017;24(7):1778–1782. doi:10.1245/s10434-016-5623-3.
- Arnason T, Kamionek M, Yang M, et al. Significance of proximal margin involvement in low-grade appendiceal mucinous neoplasms. Arch Pathol Lab Med. 2015;139(4):518–521. doi:10.5858/arpa.2014-0246-OA.
- Sugarbaker PH. Epithelial appendiceal neoplasms. Cancer J. 2009;15(3):225–235. doi:10.1097/PPO.0b013e3181a9c781.
- Carr NJ, Bibeau F, Bradley RF, et al. The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei. Histopathology. 2017;71(6):847–858. doi:10.1111/his.13324.
- Gonzalez-Moreno S, Sugarbaker PH. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg. 2004;91(3):304–311. doi:10.1002/bjs.4393.
- Murphy EM, Farquharson SM, Moran BJ. Management of an unexpected appendiceal neoplasm. Br J Surg. 2006;93(7):783–792. doi:10.1002/bjs.5385.
- Moran B, Baratti D, Yan TD, et al. Consensus statement on the loco-regional treatment of appendiceal mucinous neoplasms with peritoneal dissemination (pseudomyxoma peritonei). J Surg Oncol. 2008;98(4):277–282. doi:10.1002/jso.21054.
- Asenov Y, Korukov B, Penkov N, et al. Appendiceal mucocele - case report and review of the literature. Chirurgia (Bucur). 2015;110(6):565–569.
- Dhage-Ivatury S, Sugarbaker PH. Update on the surgical approach to mucocele of the appendix. J Am Coll Surg. 2006;202(4):680–684. doi:10.1016/j.jamcollsurg.2005.12.003.
- Saylam B, Güldoğan CE, Coşkun F, et al. Distinguishing between acute appendicitis and appendiceal mucocele: is this possible preoperatively? Eur J Trauma Emerg Surg. 2013;39(5):523–529. doi:10.1007/s00068-013-0321-3.
- Lorenzon L, De Dominicis C, Virgilio E, et al. The appropriate management of an appendiceal mucocele. BMJ Case Rep. 2015;2015. doi:10.1136/bcr-2014-209045.
- Zhang W, Tan C, Xu M, et al. Appendiceal mucinous neoplasm mimics ovarian tumors: challenges for preoperative and intraoperative diagnosis and clinical implication. Eur J Surg Oncol. 2019;45(11):2120–2125. doi:10.1016/j.ejso.2019.08.004.
- Shaib WL, Assi R, Shamseddine A, et al. Appendiceal mucinous neoplasms: diagnosis and management. Oncologist. 2017;22(9):1107–1116. doi:10.1634/theoncologist.2017-0081.
- Fournier K, Rafeeq S, Taggart M, et al. Low-grade Appendiceal Mucinous Neoplasm of Uncertain Malignant Potential (LAMN-UMP): prognostic factors and implications for treatment and follow-up. Ann Surg Oncol. 2017;24(1):187–193. doi:10.1245/s10434-016-5588-2.
- Caspi B, Cassif E, Auslender R, et al. The onion skin sign: a specific sonographic marker of appendiceal mucocele. J Ultrasound Med. 2004;23(1):117–123 doi:10.7863/jum.2004.23.1.117.
- Karakaya K, Barut F, Emre AU, et al. Appendiceal mucocele: case reports and review of current literature. WJG. 2008;14(14):2280–2283. doi:10.3748/wjg.14.2280.
- Pitiakoudis M, Tsaroucha AK, Mimidis K, et al. Mucocele of the appendix: a report of five cases. Tech Coloproctol. 2004;8(2):109–112. doi:10.1007/s10151-004-0067-3.
- Puvaneswary M, Proietto A. Mucocele of the appendix with magnetic resonance imaging findings. Australas Radiol. 2006;50(1):71–74. doi:10.1111/j.1440-1673.2005.01530.x.
- Yu XR, Mao J, Tang W, et al. Low-grade appendiceal mucinous neoplasms confined to the appendix: clinical manifestations and CT findings. J Investig Med. 2019. doi:10.1136/jim-2018-000975.
- Demetrashvili Z, Chkhaidze M, Khutsishvili K, et al. Mucocele of the appendix: case report and review of literature. Int Surg. 2012;97(3):266–269. doi:10.9738/CC139.1.
- Cristian DA, Grama FA, Becheanu G, et al. Low-grade appendiceal mucinous neoplasm mimicking an adnexal mass. Rom J Morphol Embryol. 2015;56(2 Suppl):837–842.
- Malya FU, Hasbahceci M, Serter A, et al. Appendiceal mucocele: clinical and imaging features of 14 cases. Chirurgia (Bucur). 2014;109(6):788–793.
