Background
Over the last decade we have witnessed a rapid development and significant new enhancements in the field of minimally invasive mitral valve surgery (MIMVS), which has become a rather popular alternative to median sternotomy. In fact, MIMVS with the right lateral thoracoscopic approach, which is its major representative, has become the standard approach in many cardiac surgery centers worldwide. MIMVS is perceived to cause less pain to the patient and to lead to shorter hospitalization, accelerated recovery as well as superior cosmetic results. However, many surgeons remain concerned that the potential benefits of this technique come at the cost of vascular injuries, high rates of stroke and increased cardiopulmonary bypass (CPB) and cross clamp times. The debate between these two approaches is still ongoing as we anticipate the initial results of the UK “mini mitral trial” [Citation1]. With this brief review we will attempt to provide an answer to the question whether there is a clinical equipoise about these two operations by critically reviewing some of the available publications on the subject.
Before we refer to the current literature though, the study by Jiang et al, in the last issue of the journal [Citation2] which refers to a comparison of the 2 aforementioned techniques is truly noticeable and worthy of discussion. This was a retrospective analysis of 504 patients submitted to mitral valve surgery either with the minimally invasive or with conventional/sternotomy technique. The comparison did not yield any statistically significant results in terms of mortality, major complications and overall procedure times. Nevertheless, the minimally invasive method was associated with increased CPB and cross clamp times, less ICU length of stay and less chest tube drainage. Moreover, the authors measured inflammation indices like high sensitivity C-reactive protein, neutrophil-lymphocyte ratio, cardiac Troponin and lactate in an effort to determine the inflammatory response caused by the two different procedures. Although the levels of all the analyzed indices were lower in the minimally invasive method, this was not translated into superior clinical outcomes. Despite the fact that the study has some major limitations i.e. lack of propensity matching, it has clearly demonstrated that minimally invasive mitral surgery is a safe and efficient alternative as shown by the high repair rates, low conversion rates and the few reported complications.
Improvement in the outcomes of MIMVS
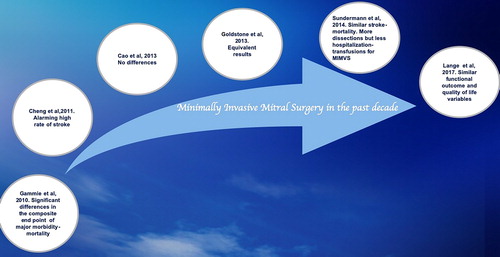
Undisputedly, in order to establish any innovative surgical method, there is one and only prerequisite; the outcomes of the new method need to be equal or even better to the reference standard one. Although the initial experience with thoracoscopic mitral valve surgery documented mortality rates near 10% [Citation3], all recent studies demonstrate equal operative mortality and perioperative outcomes between the two procedures [4]. The right minithoracotomy MIMVS facilitates excellent visualization of the diseased mitral valve and the repair rates are often reported better than its alternative in recent papers. The evolution of MIMVS through some cornerstone papers is depicted in . The propensity-matched analysis of Gammie and colleagues back in 2010 [Citation5], raised serious concerns about the safety of MIMVS, as it reported statistically significant differences in the composite end point of major hospital morbidity (defined as the need for reoperation, deep sternal wound infection, stroke, renal failure and prolonged ventilation) and mortality against the minimally invasive procedures. The next hallmark paper comes from Cheng et al in 2011 [Citation6]. In this systematic review and meta-analysis which included thirty-five studies, the authors reported significantly increased comorbidities and an alarming high risk of stroke for the MIMVS versus the full sternotomy group. Notably, the 30-day risk of stroke was 2.1% vs 1.2%, the aortic dissection was reported 0.2% vs 0%, groin infections were 2% vs 0% and phrenic nerve palsy 3% vs 0%. Nevertheless, the mortality was comparable between the 2 groups and a number of clinical outcomes such as atrial fibrillation (AF) rates, chest tube drainage, need for transfusion, sternal infection, time to return to normal activity and patient scar satisfaction were improved in the minimally invasive group. The meta-analysis by Cao and colleagues in 2013 identified seven relevant studies including one randomized controlled trial and six retrospective studies [Citation7]. The authors did not identify any statistically significant differences between MIMVS and conventional mitral valve surgery. In the same year, Goldstone et al, in their propensity matched analysis reported comparable outcomes for the two procedures, with the only exception being the exploration for hemorrhage rate, which was 5-fold higher of in the MIMVS group (2.5% vs 0.5%), (1 patient vs 5 patients in the overall cohort) [Citation8]. Sundermann and his group in their paper included more than 20.000 patients and forty-five studies. They exhibited similar perioperative outcomes for the two methods [Citation4]. They reported similar stroke rates and all-cause mortality, but less ICU and hospital stay, fewer blood transfusions and postoperative AF for the MIMVS. In contrast more aortic dissections occurred in the MIMVS group.
In view of the encouraging reported results the application of the MIMVS has increased over the last years. More specifically, in the United States, the percentage of patients undergoing a MIMVS procedure increased from 11.9% in 2004 to 20.1% in 2008 [Citation5], whereas in Germany, according to the German Society for Thoracic and Cardiovascular Surgery Annual Registry survey report in 2013 the percentage has gone from 13.1% in 2004 to 45.2% in 2013.
Concerns about MIMVS
Despite the shift in the evidence that we have witnessed throughout the last decade, still the minimally invasive approach for mitral valve surgery is not unanimously accepted. Most surgeons are concerned that the limited exposure renders the procedure technically more demanding and therefore time consuming. Indeed, the common denominator in all trials referenced here as well as in current literature is the increased cross clamp and cardiopulmonary bypass times. In line with these papers Jiang et al, reported statistically significant prolonged times for the MIMVS (52 vs 45 min and 87 vs 76 min) [Citation2]. The well-known deleterious effects of CPB may not have been mirrored in the outcomes of the reported meta-analyses as well as in the most of the current papers on this topic, hence the equivalency. Is this because the CPB techniques are continuously evolving and getting better? Or it is just because there is a pre-selection of patients allocated to receive the minimally invasive operation i.e. a surgeon will only select a suitable patient with good LV function for example to undergo minimally invasive surgery? This is well depicted in the paper by Lange et al, [Citation9] in which we recognize that if we concentrate in the matched patients’ analysis only CPB and cross clamp times are reported statistically significant in favor of the conventional operation, as opposed to the unmatched patients’ cohort which clearly favors the MIMVS. Moreover, the survival and freedom from reoperation in the matched group is worse for the MIMVS group but this did not reach statistical significance.
The applicability of the MIMVS is confined by some absolute and relative contraindications (). Potential restrictions include concomitant procedures for example aortic valve replacement or coronary artery bypass grafting. Other potential limitations include visualization difficulties in patients with challenging anatomy (morbid obesity) and difficult pathology of mitral valve disease.
Table 1. Relative and absolute contraindications of MIMVS.
Another important concern is the rate of stroke which was always a challenge for MIMVS. Increased rates were attributed to suboptimal deairing techniques, retrograde perfusion, prolonged CPB times and aortic occlusion techniques (endoballoon). To be fair though, it seems that the rates are significantly improving in the current era.
Additionally, we ought to mention that a true learning curve exists for minimally invasive surgery of the mitral valve. A keystone paper from Friedrich Mohr’s group back in 2013 has methodically examined the learning curve of MIMVS [Citation10]. The authors conclude that MIMVS has a prolonged learning curve, even in a center performing a large volume of minimally invasive operations. Notably, according to authors 75-125 surgeries are required to overcome the learning curve. Moreover, they stress that it is imperative for a surgeon in order to maintain competence, to perform more than one MIMVS per week, which corresponds almost to fifty a year. Furthermore, they state that before a surgeon starts practicing on minimally invasive mitral surgeries, he/she needs to be confident with the conventional technique (at least 40 open mitral repairs) and the initial minimally invasive operations should be restricted to preferably male patients who are non-obese and have a simple pathology [Citation10]. These results have been echoed by other contemporary papers investigating the experience required in order to produce good outcomes in mitral valve surgery [Citation11]. A mitral surgeon needs to possess a certain skill set and a minimum average volume of 25 mitral operations/year represents a good threshold in order to maintain and further develop expertise [Citation11]. Therefore, case volume is absolutely essential for mitral valve surgery and especially for MIMVS.
Finally, some studies claim that MIMVS is beneficial with regards to postoperative pain and quick recovery, however there seems to be a relative paucity of robust data to support this. Postoperative pain and scar are presumably improved by smaller incisions but little evidence exists so far to consider these endpoints. To the best of our knowledge, there is one systematic evaluation of pain-related outcomes in the randomized trial by Speciale et al, which reports significantly lower pain scores for MIMVS [Citation12].
Conclusions
One of the biggest proponents of the MIMVS quoted “If two treatment options produce equal outcomes the lesser-invasive one will prevail” [Citation13]. There is enough evidence that MIMVS is a safe procedure with comparable mortality and adverse events with standard sternotomy [Citation9], and currently the most frequently used minimally invasive cardiac valve operation worldwide [Citation5]. Nevertheless, we find that the classic sternotomy approach will not be supplanted for all the concerns described above.
The retrospective analysis by Jiang et al, in the current issue of the journal has shown that MIMVS is an efficient technique as shown by the high repair rates (51 out of 58). Moreover, the authors have shown that MIMVS and conventional mitral valve surgery have comparable perioperative outcomes while MIMVS also exhibited a lower inflammation impact as shown by the respective measured indices.
At present, there is a paucity of prospective randomized controlled trials on this subject and the expert clinical community still has no definitive answer as to which operation is better. This clinical equipoise will be addressed once we possess good quality randomized controlled trials (RCTs). On this direction, there is a RCT underway, namely the UK “mini mitral trial”. Although this will not primarily investigate mortality endpoints, (only physical functioning and cost-effectiveness), it will be the largest trial in this field worldwide.
MIMVS is certainly attractive due to small scars and cosmetic results, however it should not be driven only by patient perceived benefits. In view of the steep learning curves, the challenging procedural technicalities and the volume of cases needed for a surgeon to maintain skills, these procedures should, for the time being, be limited to specialist centers.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Minimally invasive thoracoscopically-guided right minithoracotomy versus conventional sternotomy for mitral valve repair. doi:10.1186/ISRCTN13930454.
- Jiang Q, et al. Retrospective comparison of endoscopic versus open procedure for mitral valve disease. J Invest. Surg. 2021;34(9):1000–1006.
- Mohr FW, Falk V, Diegeler A, et al. Minimally invasive port-access mitral valve surgery. J Thorac Cardiovasc Surg. 1998;115(3):567–574. doi:10.1016/S0022-5223(98)70320-4.
- Sündermann SH, Sromicki J, Rodriguez Cetina Biefer H, et al. Mitral valve surgery: right lateral minithoracotomy or sternotomy? A systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2014;148(5):1989–1995.e4. doi:10.1016/j.jtcvs.2014.01.046.
- Gammie JS, Zhao Y, Peterson ED, O'Brien SM, Rankin JS, Griffith BP. Less-invasive mitral valve operations: trends and outcomes from the society of thoracic surgeons adult cardiac surgery database. Ann Thorac Surg. 2010;90(5):1401–1408. doi:10.1016/j.athoracsur.2010.05.055.
- Cheng DCH, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations. 2011;6(2):84–103. doi:10.1097/imi.0b013e3182167feb.
- Cao C, Gupta S, Chandrakumar D, et al. A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral disease. Ann Cardiothorac Surg. 2013;2(6):693–703. doi:10.3978/j.issn.2225-319X.2013.11.08.
- Goldstone AB, Atluri P, Szeto W, et al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: a propensity-matched comparison. J Thorac Cardiovasc Surg. 2013;145(3):748–756. doi:10.1016/j.jtcvs.2012.09.093.
- Lange R, Voss B, Kehl V, Mazzitelli D, Tassani-Prell P, Günther T. Right minithoracotomy versus full sternotomy for mitral valve repair: a propensity matched comparison. Ann Thorac Surg. 2017;103(2):573–579. doi:10.1016/j.athoracsur.2016.06.055.
- Holzhey DM, Seeburger J, Misfeld M, Borger MA, Mohr FW. Learning minimally invasive mitral valve surgery:a cumulative sum sequential probability analysis of 3895 operations from a single high-volume center. Circulation. 2013;128(5):483–491. doi:10.1161/CIRCULATIONAHA.112.001402.
- Chikwe J, Toyoda N, Anyanwu AC, et al. Relation of mitral valve surgery volume to repair rate, durability, and survival. J Am Coll Cardiol. 2017.
- Speziale G, Nasso G, Esposito G, et al. Results of mitral valve repair for Barlow disease (bileaflet prolapse) via right minithoracotomy versus conventional median sternotomy: a randomized trial. J Thorac Cardiovasc Surg. 2011;142(1):77–83. doi:10.1016/j.jtcvs.2010.08.033.
- Modi P, Hassan A, Chitwood WR. Jr. Minimally invasive mitral valve surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg. 2008;34(5):943–952. doi:10.1016/j.ejcts.2008.07.057.