 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: To investigate the efficacy of two different surgical procedures in combined hysteroscopic and laparoscopic surgery—the “folding suture method” and the “muscle flap filling suture method"—in the treatment of cesarean scar diverticulum (CSD).
Methods: The clinical data of 24 patients with CSD who underwent surgery in the Peking University First Hospital from August 2016 to December 2018 were retrospectively analyzed.
Results: There was no difference in age, vaginal bleeding time, thickness of the lower uterine segment, operative time and intraoperative bleeding between the two groups. At three months after the operation, the patients of the folding suture and muscle flap groups had an average menstrual period of 6.9 ± 1.8 days and 7.5 ± 3.0 days, respectively, which was 5.8 ± 4.2 days and 4.4 ± 3.8 days, respectively, shorter than that before the operation, as well as a lower segment thickness of the uterus of 6.7 ± 1.8 mm and 6.3 ± 1.7 mm, respectively. Among the patients in the folding suture and muscle flap groups, 8 and 6 cases were cured, and 3 and 6 cases were improved, respectively, resulting in an effective rate of 100%. There was no significant difference in any indicator between the two groups.
Conclusion: As two new surgical methods that preserve uterine integrity, the laparoscopic "muscle flap filling suture method" and “folding suture method” combined with hysteroscopic incision are safe and effective treatments for repairing CSD.
Introduction
Previous cesarean scar diverticulum (PCSD) refers to the occurrence of a pouch-like defect that is connected with the uterine cavity in the anterior wall isthmus of the uterus after cesarean section, possibly leading to a series of symptoms such as abnormal uterine bleeding, chronic pelvic pain, infertility, and asymptomatic [Citation1]. Transvaginal ultrasound, magnetic resonance imaging, contrast-enhanced ultrasound imaging of the uterine cavity, hysterosalpingography, hysteroscopy, and ultrasound combined with hysteroscopy can be used for the auxiliary diagnosis of CSD [Citation2, Citation3]. The incidence of CSD after cesarean section detected by ultrasound has been reported to reach 56-84%. The prevalence of cesarean section scar dehiscence appears to be high in a population of patients who have had at least one cesarean section, but varies widely, between 24% and 84%, depending on the diagnostic tools used; the intraoperative single layer suture of the myometrium during cesarean section, a history of multiple cesarean sections, and retroflexion of the uterus are high risk factors for its onset [Citation3]. Recent research suggests that that the use of synthetic absorbable monofilament sutures for uterine closure was associated with increased residual myometrial thickness, with respect to synthetic absorbable multifilament sutures. The increased residual myometrial thickness may be associated with a reduced incidence of isthmocele [Citation4]. As the cesarean section rate has increased in recent years, CSD after cesarean section has attracted increasing attention by clinicians as a long-term complication.
PCSD treatments are divided into conservative observation, medical treatment, and surgical treatment. The patients with small diverticula, mild or no symptoms, and no fertility requirements usually undergo conservative observation or medical treatment [Citation5]. The formation of scar diverticulum is an anatomical change, and surgical treatment may fundamentally solve the problem. Common surgical procedures include hysteroscopic electroresection of diverticular scars and electrocoagulation of the intima inside the diverticulum [Citation6–8], laparoscopic or combined hysteroscopic and laparoscopic surgical resection of diverticular scar and uterus repair [Citation9–11], and transvaginal surgical resection of scar and uterus repair [Citation12, Citation13]. Among these procedures, the combined hysteroscopic and laparoscopic surgical resection of scar and uterus repair method has been widely used in recent years.
A consensus statement from the Global Congress on Hysteroscopy Scientific Committee recommended that in cases where myometrial thickness is greater than 3 mm, hysteroscopic treatment represents a feasible and safe approach; conversely, when myometrial thickness is less than 3 mm, the laparoscopic approach should be favored because of the risk of uterine perforation and bladder injury [Citation14, Citation15]. Uterine scar repair through vaginal surgical resection has the advantages of being minimally invasive, having a short recovery time, and having a low cost [Citation16–18]. However, the usual resection of local scar tissue to resuture the lower segment of the uterus has a long postoperative recovery time, and the diverticulum may reform during the healing process. Our hospital adopted two new combined hysteroscopic and laparoscopic surgical procedures—the muscle flap filling suture method and the folding suture method—which do not need to remove the scar tissue while repairing the scar diverticulum to preserve the integrity of the uterus. Good results have been achieved and are reported below.
Materials and methods
General information
The clinical data of 24 patients with cesarean scar diverticulum who underwent surgical treatment in the Peking University First Hospital from August 2016 to December 2018 were retrospectively analyzed. Among them, 11 patients received combined hysteroscopic and laparoscopic muscle flap filling suture (from February 2018 to December 2018), and 13 patients received combined hysteroscopic and laparoscopic folding suture (from August 2016 to January 2018). The medical history, symptoms, auxiliary examination, and intraoperative conditions of the patients were collected, and postoperative recovery was followed up by outpatient visit and phone calls with a follow-up range from 3 months to 30 months. One patient who received folding suture was lost to follow-up after operation.
Inclusion and exclusion criteria
Inclusion criteria: (1) medical history and ultrasound examination suggested a diagnosis of CSD, and the remaining myometrial thickness at the PCSD site was < 3 mm based on previous literature reports [Citation19–21]; (2) the patient had fertility requirement; and (3) this was their first surgical treatment. Exclusion criteria: (1) CSD presented with other diseases leading to abnormal uterine bleeding, such as endometrial lesions, submucosal fibroids, and coagulation disorders, or (2) CSD was combined with systemic diseases such as severe heart and lung diseases, as well as hepatic and renal insufficiency ().
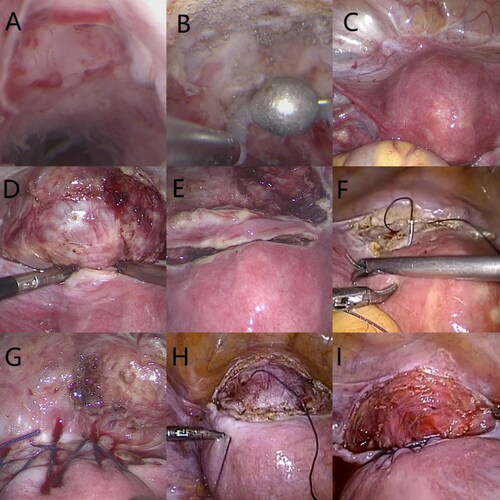
Figure 1. (A) Hysteroscopy of the cesarean scar defect (CSD). (B) Hysteroscopy after electrical resection of the scar (canal opening) and electrocoagulation of the diverticular endometrium. (C) Laparoscopy of the CSD. (D) Laparoscopic visualization of the diverticulum with guidance from the light source of the hysteroscope after opening and deflecting the vesicouterine pouch. (E) The muscle flap filling suture method: a monopolar electrical probe was used to make a transverse incision in the myometrium 1 cm above the diverticulum to a depth of approximately 0.5 cm. (F) The muscle flap filling suture method. (G) After muscle flap filling suture. (H) The folding suture method. (I) After folding suture.
Surgical methods
For both procedures, hysteroscopy was performed first to observe the size of the diverticulum and the scar condition. If the scar formed an obvious protuberance and there was intimal vascular proliferation in the diverticulum, then electroresection of the scar and electrocoagulation of the diverticular intima were performed. The pelvic cavity conditions were explored laparoscopically to separate the adhesions and open vesicoperitoneal reflection. Under the guidance of the hysteroscopic light source, the location and range of the diverticulum of the cesarean section were observed. The adhesion between the bladder and the cesarean scar at the lower segment of the uterus was separated. The bladder was pushed down 2 cm below the scar diverticulum. At the same time, the serosal surface of the lower uterine segment formed a rough surface. At this time, the folding suture method used 2-0 absorbable sutures to continuously suture the upper and lower poles of the diverticulum to form a fold and increase the myometrial thickness at the diverticulum. The muscle flap filling suture method used a monopolar electric hook to transversely incise the muscular layer with at a depth of approximately 0.5 cm and approximately 1 cm above the diverticulum, and the length reached both sides of the uterus so that it was folded down to form a muscle flap. A 2-0 absorbable suture was used to bypass the muscle flap and continuously suture the muscle tissue above and below the diverticulum, and the muscle flap was used to fill the diverticulum. After being sutured with both methods, the uterus was in anteversion and anteflexion positions, and no obvious diverticulum was observed when hysteroscopy was performed again.
Observation indicators
The observation indicators were divided into three groups: (1) basic clinical data including age, the time between the surgery and the last cesarean section, the number of cesarean sections, the date and duration of menstrual period before cesarean section and after cesarean section, the myometrial thickness at the diverticulum, and the preoperative hemoglobin concentration; (2) perioperative conditions including intraoperative blood loss, operation time, postoperative indwelling time of the urinary catheter, postoperative exhaust time, maximal postoperative body temperature, postoperative decrease in hemoglobin concentration, and surgical complications; and (3) postoperative efficacy data such as postoperative menstrual period, time reduction in menstrual period, postoperative lower myometrial thickness, cure rate, and effective rate. The efficacy evaluation status and criteria were as follows: (1) cured, in which the patient's menstrual cycle returned to normal, and the ultrasound examination of the lower segment scar of the uterus showed the disappearance of the liquid dark area; (2) improved, in which the vaginal bleeding time was significantly shorter than that before the surgery but still > 7 days, and the ultrasound examination of the lower segment scar of the uterus showed that the liquid dark area was smaller than that before the surgery or disappeared; and (3) ineffective, in which the menstrual cycle was not significantly shorter than before, and the ultrasound examination of the lower segment scar of the uterus showed that the liquid dark area did not change significantly. The effective rate was the sum of the cure rate and the improvement rate.
Statistical methods
SPSS software version 19.0(SPSS Inc., Chicago, IL, USA) was used for the statistical analysis of the data. The differences between the two groups were analyzed using the two independent samples t-test, paired samples t-test, or Fisher exact test. P values < 0.05 were considered statistically significant.
Results
Comparison of basic clinical data
There were no significant differences in age, the time between the surgery and the last cesarean section, the number of cesarean sections, vaginal bleeding time during menstruation, myometrial thickness at the diverticulum, and preoperative hemoglobin concentration between the patients in the two groups, as shown in .
Table 1. Analysis of the basic clinical data of the patients in the two groups
Comparison of perioperative conditions
In the muscle flap filling suture group, one patient had perforation at the diverticulum during hysteroscopy, and no significant bleeding at the perforation was observed under a laparoscope. There was no significant difference in intraoperative blood loss, decrease in hemoglobin concentration, operation time, indwelling time of urinary catheter, postoperative exhaust time, maximal body temperature and hospital stay between the patients in the two groups, as shown in . In the folding suture group, two patients had abdominal drainage tube indwelling, which was removed on the third postoperative day. In the muscle flap filling suture group, one patient had abdominal drainage tube indwelling, which was removed on the second postoperative day. The patients in the two groups recovered smoothly without postoperative complications.
Table 2. Analysis of perioperative clinical data of the patients in the two groups (x ± s).
Comparison of efficacy
The postoperative menstrual cycle in the two groups was significantly shorter than that before the operation (paired sample t-test, p = 0.000). In the muscle flap filling suture group, the average myometrial thickness of lower uterine segment increased from 2.1 mm before the operation to 6.7 mm at 3 months after operation (paired sample t-test, p = 0.000). In the folding suture group, it increased from 1.8 mm before the operation to 6.3 mm after the operation (paired sample t-test, p = 0.000). The effective rate of both groups was 100%(The effective rate was the sum of the cure rate and the improvement rate). There was no significant difference in surgical effect (menstrual period, myometrial thickness of lower uterine segment, healing rate, or effective rate) (shown in ). All patients underwent ultrasound examination at 3 months after the surgery, while 7 of them underwent ultrasound examination again at 6 months after the surgery. The results showed no significant change in the thickness of the lower uterine segment compared with that at 3 months (paired sample t-test, p = 0.296).
Table 3. Comparison of surgical efficacy between the patients in the two groups (x ± s).
Pregnancy after operation
Seven patients in the folding suture group had pregnant intention after six months of surgery, including four successful pregnancy, with an average time of 17.75 months after surgery (81,12,428 months respectively). Ultrasound examination showed that the myometrial of the lower uterine segment was continuous during pregnancy. Scheduled cesarean sections were performed at 37-39 weeks of pregnancy. The operation was smooth without surgical complications. One patient was pregnant 11 months postoperatively, underwent a midterm induction at 13 weeks of gestation due to fetal malformation. One got pregnant at 18 months performing an induced abortion due to early embryonic death. A cesarean scar pregnancy occurred after 14 months of the surgery, uterine artery embolization was performed and no pregnancy was attempted after induced abortion.
Four patients in the muscle flap filling suture group attempted to be pregnant 6 months after operation, including one pregnancy after 7 months of surgery, myometrial of the lower uterine segment was continuous during pregnancy, with a scheduled cesarean section at 37 + 4 weeks with no complication. Two patients got pregnant at 9 and 16 months postoperatively, induced abortions were performed due to family reasons and early embryonic death. One patient did not have a successful pregnancy at the time of publication.
Discussion
Improved vaginal bleeding and blood spotting symptoms after surgery
Postmenstrual vaginal blood spotting is the most common symptom of CSD. When women with a history of cesarean section experience prolonged menstrual periods, CSD should be suspected. The occurrence of symptoms such as inexhaustible bleeding, chronic pelvic pain, and infertility seriously affects the physical and mental health of women and should be actively treated [Citation5]. The symptoms of vaginal blood spotting can be improved in 82%-100% of patients with laparoscopic surgical repair [Citation9, Citation11, Citation22, Citation23] . The study by Li et al. showed that the average time of vaginal bleeding at 1 month after the combined hysteroscopic and laparoscopic excision and suture of uterine scar was 10.5 days, which was 2.5 days less than that before surgery; by three months after surgery, it was 7.5 days, a reduction 5.5 days [Citation22]. In this study, the total effective rate of the two laparoscopic surgical methods in relieving vaginal bleeding was 100%, and the duration of vaginal bleeding was reduced by 5.8 days and 4.4 days. The symptoms were improved at the time of the first postoperative menstruation, and there was no significant change in the symptoms and ultrasonography at 6 months after surgery compared with those at 3 months. These two surgical methods did not require incision of the uterus, and the integrity of the uterine wall was preserved. Thus the lower segment of the anterior wall of the uterine cavity did not need to undergo a trauma repair process again, and the symptoms were relieved immediately after surgery.
Surgical improvement of scar thickness
Laparoscopic uterine scar repair has been widely used in recent years. The operative field is clear under laparoscopy, enabling definitive scar removal and resuturing of the uterus to restore the anatomical structure. The aim is to radically eliminate the diverticulum and improve symptoms [Citation10, Citation11]. The study by Dosedla et al. showed that the symptoms of vaginal bleeding were relieved in 82% of patients after surgery, and the average thickness of the lower segment of the uterus increased from 0.3 mm before surgery to 1.3 mm after surgery. However, 81.8% of patients still had severe scar diverticula postoperation, which was thought to be related to the greater tension on the newly formed scar. [Citation11]. Moreover, the margins of the resutured incision after resection of the diverticulum were difficult to align, so there was uncertainty in scar healing and possibility for the diverticulum to form again. Donnez et al. used nuclear magnetic resonance to measure the average thickness of the lower uterine segment before and after the surgery, which increased from 1.4 mm to 9.6 mm [Citation9]. In this study, the two suture methods did not penetrate the intima, and the inflammatory reaction was small. The raised "dyke" around the diverticulum was eliminated from the uterine cavity side, and the suturing was done from the serosal surface to increase the thickness of the diverticulum. The efficacy was certain. Ultrasonography showed that only 3 patients in each group had residual diverticulum, but the size of the diverticulum was significantly reduced compared with that before surgery, and the myometrial thickness was significantly increased.
Necessity of combined hysteroscopic and laparoscopic surgery
It is necessary to perform combined hysteroscopic surgery. First, these two surgical procedures do not remove the local scar. Under hysteroscopy, we often find that there is protruding scar tissue around the diverticulum, which cannot be eliminated by simple plication suture or muscle flap filling suture. Therefore, the suturing approach needs to be combined with hysteroscopic electroresection to achieve a good shaping effect. Second, even if ultrasound or hysteroscopy suggests that the diverticulum is large, no obvious diverticulum can be seen laparoscopically, and the size and location of the diverticulum cannot be determined [Citation11]. Hysteroscopy can guide laparoscopic surgery through light transmission tests, so that the diverticulum is more accurately localized [Citation9, Citation22]. Third, after completing surgical suturing, hysteroscopy can be used to examine the surgical effect the postoperative reduction of the diverticulum.
These two surgical methods have small surgical trauma, less operation difficulty, less bleeding, short operation time, and fast postoperative recovery. Because the suture methods preserve the integrity of the uterus, the time required for contraception after operation is short. However, at present, the follow-up time for patients is short. Future studies need to further track the patients’ pregnancy status.
Taken together, as two new surgical methods that preserve the integrity of the uterus, the combined hysteroscopic and laparoscopic "muscle flap filling suture method" and "folding suture method" for repairing CSD shorten the duration of contraception for patients with urgent fertility requirements. They also have the advantages of being minimally invasive, safe, and effective.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Api M, Boza A, Gorgen H, et al. Should cesarean scar defect be treated laparoscopically? A case report and review of the literature. J Minim Invasive Gynecol. 2015;22(7):1145–1152. doi:https://doi.org/10.1016/j.jmig.2015.06.013.
- Yao M, Wang W, Zhou J, et al. Cesarean section scar diverticulum evaluation by saline contrast-enhanced magnetic resonance imaging: the relationship between variable parameters and longer menstrual bleeding. J Obstet Gynaecol Res. 2017;43(4):696–704. doi:https://doi.org/10.1111/jog.13255.
- Bij De Vaate AJM, van der Voet LF, Naji O, et al. Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol. 2014;43(4):372–382. doi:https://doi.org/10.1002/uog.13199.
- Laganà AS, Cromi A, Tozzi R, et al. Uterine scar healing after cesarean section: managing an old surgery in an evidence-based environment. J Invest Surg. 2019;32(8):770–772. doi:https://doi.org/10.1080/08941939.2018.1465145.
- Setubal A, Alves J, Osorio F, et al. Treatment for uterine isthmocele, a pouchlike defect at the site of a cesarean section scar. J Minim Invasive Gynecol. 2018;25(1):38–46. doi:https://doi.org/10.1016/j.jmig.2017.09.022.
- Vervoort A, van der Voet LF, Hehenkamp W, et al. Hysteroscopic resection of a uterine caesarean scar defect (niche) in women with postmenstrual spotting: a randomised controlled trial. BJOG. 2018;125(3):326–334. doi:https://doi.org/10.1111/1471-0528.14733.
- Tsuji S, Kimura F, Yamanaka A, et al. Impact of hysteroscopic surgery for isthmocele associated with cesarean scar syndrome. J Obstet Gynaecol Res. 2018;44(1):43–48. doi:https://doi.org/10.1111/jog.13464.
- Abacjew-Chmylko A, Wydra DG, Olszewska H. Hysteroscopy in the treatment of uterine cesarean section scar diverticulum: a systematic review. Adv Med Sci. 2017;62(2):230–239. doi:https://doi.org/10.1016/j.advms.2017.01.004.
- Donnez O, Donnez J, Orellana R, et al. Gynecological and obstetrical outcomes after laparoscopic repair of a cesarean scar defect in a series of 38 women. Fertil Steril. 2017;107(1):289–296. doi:https://doi.org/10.1016/j.fertnstert.2016.09.033.
- Zhao W, Liu G, Yang Q, et al. A new method using a Foley Catheter to locate the diverticulum in laparoscopic repair of uterine cesarean scar defects. Eur J Obstet Gynecol Reprod Biol. 2018;223:14–17. doi:https://doi.org/10.1016/j.ejogrb.2018.01.033.
- Dosedla E, Calda P. Outcomes of laparoscopic treatment in women with cesarean scar syndrome. Med Sci Monit. 2017;23:4061–4066. doi:https://doi.org/10.12659/MSM.902720.
- Yao S. Transvaginal management of cesarean scar section diverticulum: a novel surgical treatment. Med Sci Monit. 2014;20:1395–1399. doi:https://doi.org/10.12659/MSM.890642.
- Chen H, Wang H, Zhou J, et al. Vaginal repair of cesarean section scar diverticula diagnosed in non-pregnant women. J Minim Invasive Gynecol. 2019;26(3):526–534. doi:https://doi.org/10.1016/j.jmig.2018.06.012.
- Laganà AS, Pacheco LA, Tinelli A, Global Congress on Hysteroscopy Scientific Committee, et al. Optimal timing and recommended route of delivery after hysteroscopic management of isthmocele? A consensus statement from the global congress on hysteroscopy scientific committee. J Minim Invasive Gynecol. 2018;25(4):558. doi:https://doi.org/10.1016/j.jmig.2018.01.018.
- Lagana AS, Alonso PL, Tinelli A, et al. Authors' reply. J Minim Invasive Gynecol. 2018;25(6):1112–1113. doi:https://doi.org/10.1016/j.jmig.2018.04.009.
- Luo L, Niu G, Wang Q, et al. Vaginal repair of cesarean section scar diverticula. J Minim Invasive Gynecol. 2012;19(4):454–458. doi:https://doi.org/10.1016/j.jmig.2012.03.012.
- Zhang Y. A Comparative study of transvaginal repair and laparoscopic repair in the management of patients with previous cesarean scar defect. J Minim Invasive Gynecol. 2016;23(4):535–541. doi:https://doi.org/10.1016/j.jmig.2016.01.007.
- Zhou J, Yao M, Wang H, et al. Vaginal repair of cesarean section scar diverticula that resulted in improved postoperative menstruation. J Minim Invasive Gynecol. 2016;23(6):969–978. doi:https://doi.org/10.1016/j.jmig.2016.06.013.
- Ofili-Yebovi D, Ben-Nagi J, Sawyer E, et al. Deficient lower-segment Cesarean section scars: prevalence and risk factors. Ultrasound Obstet Gynecol. 2008;31(1):72–77. doi:https://doi.org/10.1002/uog.5200.
- Vikhareva Osser O, Valentin L. Risk factors for incomplete healing of the uterine incision after caesarean section. BJOG: An International Journal of Obstetrics & Gynaecology. 2010;117(9):1119–1126. doi:https://doi.org/10.1111/j.1471-0528.2010.02631.x.
- Jeremy B, Bonneau C, Guillo E, et al. Hernie transmurale isthmique de l’utérus: résultats de l’isthmorraphie sur la symptomatologie et la fertilité. Gynécologie Obstétrique & Fertilité. 2013;41(10):588–596. doi:https://doi.org/10.1016/j.gyobfe.2013.08.005.
- Li C, Tang S, Gao X, et al. Efficacy of combined laparoscopic and hysteroscopic repair of post-cesarean section uterine diverticulum: a retrospective analysis. Biomed Res Int. 2016;2016:1–6. doi:https://doi.org/10.1155/2016/1765624.
- Schepker N, Garcia-Rocha GJ, von Versen HF, et al. Clinical diagnosis and therapy of uterine scar defects after caesarean section in non-pregnant women. Arch Gynecol Obstet. 2015;291(6):1417–1423. doi:https://doi.org/10.1007/s00404-014-3582-0.
