Abstract
Background
One cause of anastomotic leakage after radical esophagectomy is blood flow insufficiency at the cervical anastomosis site. .
Methods
Eighteen patients, who underwent radical esophagectomy with gastric tube reconstruction, were studied. The regional tissue oxygen saturation (rSO2) was measured at the tip (point pre 0) and 2, 4, and 6 cm on the distal side of the tip (point pre 1, pre 2, and pre 3, respectively) before the gastric tube was raised to the cervical site through the retrosternal route. After that, rSO2 was measured at the tip, 2 and 4 cm on the distal side of the tip (points post 0, post 1, and post 2), the actual anastomotic site (point AN), and the chest skin as an indicator of whole-body oxygenation. The relationship between rSO2 scores and the rate of anastomotic leakage was determined.
Results
The mean rSO2 at pre 0, pre 1, pre 2, and pre 3 were 48.9%, 52.3%, 54.8%, and 56.9%, respectively (p < 0.05). The mean rSO2 at post 0, post 1, and post 2 were 47.8%, 50.5%, and 52.3%, respectively, and the rSO2 at point AN was 52.1%.
Anastomotic leakage was found in 6 patients. The rSO2 at points pre 0, pre 1, and pre 2, post 0 and point AN were significantly lower in patients with anastomosis leakage than those without (p < 0.05).
Conclusion
Tissue oxygen saturation monitoring was a useful indicator of blood flow insufficiency in the gastric tube during radical esophagectomy.
Introduction
Radical esophagectomy for esophageal carcinoma is a highly invasive gastrointestinal surgery [Citation1]. Recently, surgical techniques and postoperative management have improved; hence, esophagectomy is becoming more acceptable even for elderly people. However, the rate of postoperative complications is high; in particular, anastomotic leakage is an important cause of patient morbidity [Citation2, Citation3]. One cause of anastomotic leakage is impaired blood flow in the gastric tube [Citation4]. Therefore, evaluation of blood flow in the gastric tube is important in preventing anastomotic leakage.
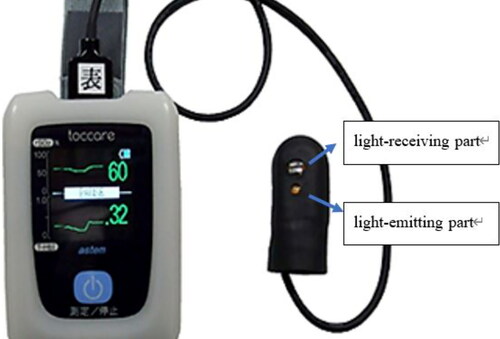
Although indocyanine green (ICG) fluorescence imaging is useful in visualizing blood supply to the gastric tube after esophagectomy [Citation5, Citation6], near-infrared spectroscopy (NIRS) is a recently developed alternative that allows the easy, noninvasive measurement of tissue oxygen saturation (rSO2; 0–%–99%) [Citation7, Citation8]. In Japan, a noninvasive blood flow evaluation device called “toccare” (Astem Co, Kanagawa, Japan) with NIRS was developed to measure oxygen saturation in the fetus during labor (). This device has also proven to be useful for evaluating limb ischemia in patients with peripheral arterial disease [Citation9]. In terms of gastric tube reconstruction, one study showed that tissue oxygen saturation was maintained after gastric tube reconstruction [Citation10]; no significant differences in rSO2 were detected before versus after gastric tube formation.
Figure 1. “Toccare” is a noninvasive device for evaluating blood flow that utilizes near-infrared spectroscopy to measure tissue oxygen saturation and total hemoglobin index with the sensor probe.
To the best of our knowledge, no study has investigated tissue oxygen saturation in the gastric tube after raising it to the cervical area. Therefore, in this study, we focused on the repeated measurement of blood supply in the gastric tube and measured rSO2 before and after raising the gastric tube to the cervical area and also at the actual anastomotic site. The study findings suggest that NIRS might be very useful for this purpose.
Patients and methods
This study was approved by the local ethics committee and all patients gave informed consent for the use of their data.
This was a retrospective study performed at the in the study hospital between November 2020 and March 2021 and included 18 patients who underwent esophagectomy with gastric tube reconstruction .
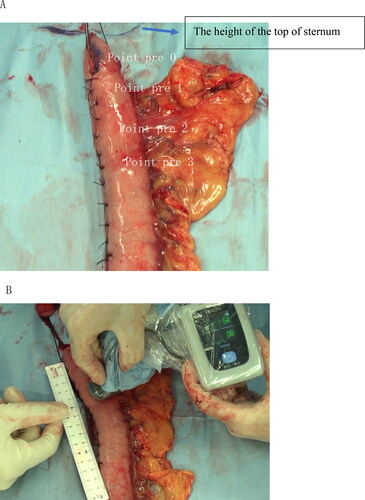
After esophagectomy, the greater omentum was incised about 3–4 cm outside the right gastroepiploic artery. After left gastric vessel ligation and lymph node dissections, gastric tube formation was performed outside the body. Usually, a small-diameter gastric tube was made with an automatic suturing device. Phlebotomy was performed to relieve congestion by cutting the small vein at the tip of the gastric tube. The seromuscular cut surface was sutured. The gastric tube was moved toward the cervical site on the chest wall, and rSO2 was measured with the “toccare” at the tip (point pre 0), and 2, 4, and 6 cm on the distal side of the tip of the gastric tube (points pre 1, pre 2, and pre 3, respectively) ().
Figure 2. A: Point pre 0, pre 1, pre 2, and pre 3 are shown at the tip, 2 cm to the anal side, 4 cm to the anal side, and 6 cm to the anal side of the tip, respectively, are shown. B: The rSO2 was measured with a “toccare” wrapped in a sterilized plastic bag.
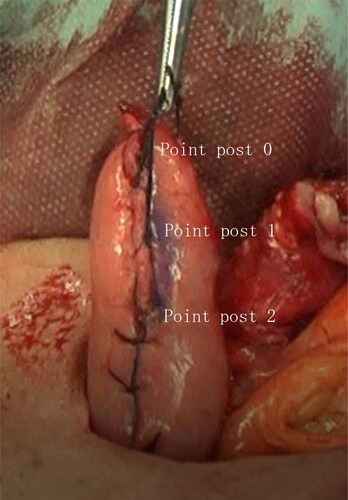
The gastric tube was raised to the cervical site via the retrosternal route. At this point, rSO2 was measured at the tip (point post 0) and 2 and 4 cm to the distal side of the tip (points post 1, and post 2). A triangular anastomosis was made using an automatic suture device in all 18 patients [Citation11, Citation12]. Then, rSO2 was measured at the anastomotic site, which was nearly equidistant between points post 1 and post 2 (point AN). As an indicator of whole-body oxygenation, rSO2 at the chest skin (point CH) was measured. The gastric tube was pulled slightly to the distal side to straighten the anastomosis site ().
Statistical analysis
Preoperative and postoperative patient characteristics were collected. The rSO2 scores between patients with or without postoperative anastomotic leakage (Clavien–Dindo grade 1 or more) were compared. Data were reported as medians or means ± standard deviation. Statistical significance was considered p-value < 0.05. A univariate analysis was performed using Pearson’s chi-square test. Fisher’s exact test, Mann–Whitney U test, and repeated-measure analysis of variance were applied as appropriate. All statistical analyses were performed using SPSS (version 27.0, IBM Corporation, NY, USA).
Results
The study included 11 men and 7 women (median age, 73; range, 58–81 years). The average body mass index was 20.4 kg/m2. shows patient characteristics potentially associated with anastomotic leakage, including tumor location, presence of diabetes mellitus (n = 2), respiratory dysfunction (%VC < 80% or FEV1.0% < 70%, n = 5), smoking history (within 6 months, n = 7), vessel disease (n = 0), and history of radiation therapy (n = 2).
Table 1. Patient characteristics.
The average rSO2 at points pre 0, pre 1, pre 2, and pre 3 were 48.9%, 52.3%, 54.8%, and 56.9% (). The rSO2 gradually increased toward the distal side (df = 4, F = 5.6, p < 0.05). The average rSO2 at points post 0, post 1, and post 2 were 47.8, 50.5, and 52.3. These rSO2 also gradually increased toward the distal side, but the changes were not statistically significant (df = 2, F = 1.8, p = 0.18). The average rSO2 at points pre 0, pre 1, and pre 2 tended to decrease compared to post 0, post 1, and post 2, though the differences were not statistically significant. The rSO2 of the chest skin (57.3% at point CH) was the highest among all rSO2 (p < 0.05).
Table 2. The rSO2 scores at each measurement point.
Postoperative anastomotic leakage (Clavien–Dindo grade 1 or more) was found in six patients. There was no gastric tube necrosis. No significant differences in preoperative characteristics (age, BMI, diabetes mellitus, vessel disease, respiratory dysfunction, smoking history, or radiation therapy history) between patients with or without anastomotic leakage were detected (). The rSO2 measurements at points pre 0, pre 1, pre 2, post 0, and point AN were significantly lower in patients with anastomosis leakage than ones without it (non-leakage vs. leakage: pre 0: 52.3% vs. 42.0%; pre 1: 54.5% vs. 47.8%; pre 2: 56.5% vs. 51.3%; post 0: 50.3% vs. 42.8%; and AN: 54.9% vs. 46.3%, p < 0.05). No significant difference in chest skin rSO2 between patients with and without anastomosis leakage was detected ().
Table 3. Comparison of patient characteristics according to the presence of anastomotic leakage.
Table 4. Comparison of rSO2 between patients with or without anastomotic leakage.
Discussion
An important step in radical esophagectomy surgery is the use of the stomach for the reconstruction. We usually use a narrow gastric tube because of the good elevation and blood flow [Citation13]. The blood flow of the formed gastric tube is an important factor in successful anastomoses [Citation4, Citation14–16]. The rate of anastomotic leakage critically impacts the safe and stable reconstruction. Many factors contribute to leakages, including insufficient blood flow.
ICG fluorescence imaging method can evaluate blood flow in free short bowel flaps and gastric tubes [Citation6, Citation17, Citation18]. The recently developed NIRS device “toccare” can measure tissue oxygen saturation easily, noninvasively, and repeatedly. The gastric tube needs to be raised to the cervical site through the postmediastinum, retrosternal, or subcutaneous routes to anastomose the remnant esophagus to the gastric tube. During this step of the reconstruction, blood flow might be compromised by the pressure and the tension required to raise the gastric tube to the cervical site through the retrosternal route. Therefore, repetitive examinations of blood flow before and after elevation of the gastric tube to the cervical site are important and the “toccare” is well-suited for repetitive measurements.
In terms of blood supply to the gastric tube, the right gastroepiploic artery is the exclusive conduit of blood to the pedicle and the blood supply of the cranial 20% of the greater curvature of the stomach is supplied by a microscopic network of capillaries and arterioles [Citation19]. Therefore, it is conceivable that the blood flow to the cranial side of the gastric tube gradually decreases toward the tip as it is raised to the cervical site.
The usefulness of NIRS for the evaluation of ischemia was reported in the construction of free flaps [Citation20]. NIRS has been used in flap reconstruction in plastic surgery [Citation21] and limb ischemia in vascular surgery [Citation9]. In these reports, the cutoff score for limb ischemia was 45%. The use of the “toccare” for measuring blood flow in the gastric tube was previously reported. The rSO2 at several points of the gastric tube and the gradients before and after gastric tube formation were investigated. No significant differences in rSO2 values before and after gastric tube formation (ligation of vessels and cutting near the lesser curvature using linear staplers) were detected. Given that only 1 patient developed anastomotic leakage in that study, the relationship between anastomotic leakage and tissue oxygen saturation could not be determined [Citation10].
In our study, we took advantage of the ability of the “toccare” to repeatedly measure rSO2. Therefore, we investigated changes in rSO2 of the gastric tube before and after raising the gastric tube to the cervical site. Furthermore, we measured rSO2 at the actual esophagogastric anastomotic site. The rSO2 scores along the gastric tube gradually increased toward the distal side, confirming the mechanism of blood supply in the small-diameter gastric tube. Thus, the “toccare” could likely measure the appropriate blood flow. No significant differences were detected in rSO2 scores before and after raising the gastric tube through the retrosternal route, indicating that the pressure and tension required for moving the gastric tube through the poststernal route might not remarkably influence blood flow in the gastric tube.
The rSO2 values at the actual anastomotic site were significantly lower in patients with anastomotic leakage than those without anastomotic leakage. Although the sample size and the number of anastomotic leakage events were too small to definitively show the relationship between rSO2 and anastomotic leakage, this result suggests that decreased blood flow might be one of the causes of anastomotic leakage. The rSO2 values at the tip before and after raising the gastric tube were also lower in patients with anastomotic leakage. If a cutoff rSO2 score was determined, additional manipulations (ex. Kocher mobilization) at the anastomotic site to a more distal site of the gastric tube might improve the rSO2 score at that site. This improvement in rSO2 might contribute toward better blood supply to the anastomotic site. Moreover, rSO2 values for several points across the gastric tube in patients with anastomotic leakage significantly decreased before raising the gastric tube further up the cervical area and there were no significant differences between the values before and after raising the gastric tube, indicating that the risk of anastomotic leakage could be predicted before raising the gastric tube through the retrosternal route.
There are several limitations to the current study. First, the sample size was very small to conclude the relationship between rSO2 and anastomotic leakage. However, our findings illustrate that it is feasible to perform the rSO2 measurement of gastric tube. Regardless, results of the current study suggest that rSO2 could be considered a useful indicator of anastomotic leakage in the gastric tube. Second, this was a retrospective analysis conducted in a single center limited to an Asian population. Moreover, we did not investigate the total hemoglobin index as an indication of congestion.
Therefore, a prospective study using the “toccare” during narrow gastric tube reconstruction with a larger number of patients is currently underway at the study institution.
In conclusion, this study demonstrated that the tissue oxygen saturation monitor “toccare” is useful for measuring blood flow insufficiency in the gastric tube during radical esophagectomy.
Acknowledgments
No specific funding from agencies in the public, commercial, or not-for-profit sectors supported this research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Lucas DJ, Pawlik TM. Quality improvement in gastrointestinal surgical oncology with American College of Surgeons National Surgical Quality Improvement Program. Surgery. 2014;155(4):593–601. doi:https://doi.org/10.1016/j.surg.2013.12.001.
- Schuchert MJ, Abbas G, Nason KS, et al. Impact of anastomotic leak on outcomes after transhiatal esophagectomy. Surgery. 2010;148(4):831–838. doi:https://doi.org/10.1016/j.surg.2010.07.034.
- Kassis ES, Kosinski AS, Ross P, Koppes KE, Donahue JM, Daniel VC. Predictors of anastomotic leak after esophagectomy: an analysis of the Society of Thoracic Surgeons general thoracic database. Ann Thorac Surg. 2013;96(6):1919–1926. doi:https://doi.org/10.1016/j.athoracsur.2013.07.119.
- Pacheco PE, Hill SM, Henriques SM, Paulsen JK, Andersonet RC. The novel use of intraoperative laser-induced fluorescence of indocyanine green tissue angiography for evaluation of the gastric conduit in esophageal reconstructive surgery. Am J Surg. 2013;205(3):349–352. doi:https://doi.org/10.1016/j.amjsurg.2012.11.005.
- Zehetner J, DeMeester SR, Alicuben ET, et al. Intraoperative assessment of perfusion of the gastric graft and correlation with anastomotic leaks after esophagectomy. Ann Surg. 2015;262(1):74–78. doi:https://doi.org/10.1097/SLA.0000000000000811.
- Takafumi Y, Hiroshi S, Yuta K, et al. Indocyanine green fluorescence angiography for quantitative evaluation of gastric tube perfusion in patients undergoing esophagectomy. J Am Coll Surg. 2015;221:e37–e42.
- Boezeman RPE, Moll FL, Unlu C, Jean-Paul PM, de Vries JPPM. Systematic review of clinical applications of monitoring muscle tissue oxygenation with near-infrared spectroscopy in vascular disease. Microvasc Res. 2016;104:11–22. doi:https://doi.org/10.1016/j.mvr.2015.11.004.
- Uchida T, Kanayama N, Kawai K, et al. Craniofacial tissue oxygen saturation is associated with blood pH using an examiner’s finger-mounted tissue oximetry in mice. J Biomed Opt. 2016;21:40502.
- Tatsuro Y, Masaki S, Hiroya T, et al. Utility of a finger-mounted tissue oximeter with near-infrared spectroscopy to evaluate limb ischemia in patients with peripheral arterial disease. Ann Vasc Dis. 2019;12:36–43.
- Kazuya Y, Yasuaki N, Toshihiro M, Niwayama M. The evaluation of the hemodynamics of a gastric tube in esophagectomy using a new noninvasive blood flow evaluation device utilizing near-infrared spectroscopy. Gen Thorac Cardiovasc Surg. 2020;68:841–847.
- Collard JM, Romagnoli R, Goncette L, Otte JB, Kestens PJ. Terminalized semimechanical side-to-side suture technique for cervical esophagogastrostomy. Ann Thorac Surg. 1998;65(3):814–817. doi:https://doi.org/10.1016/s0003-4975(97)01384-2.
- Sugimura K, Miyata H, Matsunaga T, et al. Comparison of the modified Collard and hand-sewn anastomosis for cervical esophagogastric anastomosis after esophagectomy in esophageal cancer patients: A propensity score-matched analysis. Ann Gastroenterol Surg. 2019;3(1):104–113. doi:https://doi.org/10.1002/ags3.12220.
- Sugimachi K, Ikeda M, Kai H, Ueo H, Okudaira Y, Inokuchi K. Assessment of the bloodflow in various gastric tubes for esophageal substitutes. J Surg Res. 1982;33(6):463–468. doi:https://doi.org/10.1016/0022-4804(82)90063-4.
- Allaix ME, Herbella FA, Patti MG. Hybrid trans-thoracic esophagectomy with side-to-side stapled intra-thoracic esophagogastric anastomosis for esophageal cancer. J Gastrointest Surg. 2013;17(11):1972–1979. doi:https://doi.org/10.1007/s11605-013-2281-7.
- Aminian A, Panahi N, Mirsharifi R, et al. Predictors and outcome of cervical anastomotic leakage after esophageal cancer surgery. J Can Res Ther. 2011;7(4):448–453. doi:https://doi.org/10.4103/0973-1482.92016.
- Alanezi K, Urschel JD. Mortality secondary to esophageal anastomotic leak. Ann Thorac Cardiovasc Surg. 2004;10:71–75.
- Kamiya K, Unno N, Konno H, et al. Quantitative assessment of the free jejunal graft perfusion. J Surg Res. 2015;194(2):394–399. doi:https://doi.org/10.1016/j.jss.2014.10.049.
- Kumagai Y, Ishiguro T, Ishida H, Kuwabara K, Kawano T, Ishida H. Hemodynamics of the reconstructed gastric tube during esophagectomy: assessment of outcomes with indocyanine green fluorescence. World J Surg. 2014;38(1):138–143. doi:https://doi.org/10.1007/s00268-013-2237-9.
- Liebermann-Meffert DM, Meier R, Siewert JR. Vascular anatomy of the gastric tube used for esophageal reconstruction. Ann Thorac Surg. 1992;54(6):1110–1115. doi:https://doi.org/10.1016/0003-4975(92)90077-h.
- Steele MH. Three-year experience using near infrared spectroscopy tissue oximetry monitoring of free tissue transfers. Ann Plast Surg. 2011;66(5):540–545. doi:https://doi.org/10.1097/SAP.0b013e31820909f9.
- Tsuge I, Enoshiri T, Saito S, Suzuki S. A quick evaluation of TRAM flap viability using fingerstall-type tissue oximetry. Plast Reconstr Surg Glob Open. 2017;5(9):e1494. doi:https://doi.org/10.1097/GOX.0000000000001494.