?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objectives
To perform a multi-institutional investigation of incidence and outcomes of urethral trauma sustained during attempted catheterization.
Patients & Methods
A prospective, multi-center study was conducted over a designated 3-4 month period, incorporating seven academic hospitals across the UK and Ireland. Cases of urethral trauma arising from attempted catheterization were recorded. Variables included sites of injury, management strategies and short-term clinical outcomes. The catheterization injury rate was calculated based on the estimated total number of catheterizations occurring in each center per month. Anonymised data were collated, evaluated and described.
Results
Sixty-six urethral catheterization injuries were identified (7 centers; mean 3.43 months). The mean injury rate was 6.2 ± 3.8 per 1000 catheterizations (3.18–14.42/1000). All injured patients were male, mean age 76.1 ± 13.1 years. Urethral catheterization injuries occurred in multiple hospital/community settings, most commonly Emergency Departments (36%) and medical/surgical wards (30%). Urological intervention was required in 94.7% (54/57), with suprapubic catheterization required in 12.3% (n = 7). More than half of patients (55.56%) were discharged with an urethral catheter, fully or partially attributable to the urethral catheter injury. At least one further healthcare encounter on account of the injury was required for 90% of patients post-discharge.
Conclusions
This is the largest study of its kind and confirms that iatrogenic urethral trauma is a recurring medical error seen universally across institutions, healthcare systems and countries. In addition, urethral catheter injury results in significant patient morbidity with a substantial financial burden to healthcare services. Future innovation to improve the safety of urinary catheterization is warranted.
Keywords:
Introduction
Transurethral catheter insertion is a routine medical procedure, frequently performed in inpatient, outpatient and community settings. A 2017 UK study of >9 million patients identified a urinary catheter prevalence of 14% in patients aged 18-70 years accessing National Health Service (NHS) care facilities [Citation1]. In hospital inpatient settings, UK and USA data demonstrate that urinary catheterization rates increase to 18.6 − 25% [Citation1, Citation2], and are as high as 76% in critical care units [Citation1].
Whilst catheter-associated urinary tract infection (CAUTI) is a well-reported complication of urinary catheter use, catheterization-related urethral trauma has received far less scrutiny, despite its propensity to cause even greater morbidity [Citation3, Citation4].
A previous study across two Irish academic teaching hospitals identified an incidence of urethral trauma of 6.7 per 1000 catheters inserted [Citation5]. Significantly, 81% of the 37 patients who sustained iatrogenic urethral trauma suffered morbidity classified as Clavien-Dindo grade 2 or greater. Monetarily, a cumulative total cost of £283,913 (€335,377) was ascribed to the clinical management of these injuries alone, highlighting marked relevance from a healthcare economics perspective [Citation5].
A compelling need to investigate this issue on a larger scale was apparent. We aimed to prospectively study the incidence and clinical consequence of catheterization-related trauma in a multi-institutional setting across two national healthcare systems – the National Health Service UK and the Health Service Executive of Ireland.
Materials & methods
Overview of Study Design
A multi-center, prospective, descriptive cross-sectional study was designed to identify the incidence of urethral catheterization injury occurring with standard catheterization practice, using the primary institution of three UK Hospital Trusts and four Irish Hospital Groups. Participating institutions were as follows: Manchester Royal Infirmary (Manchester University NHS Foundation Trust), Hereford County Hospital (Wye Valley NHS Trust), Norfolk and Norwich University Hospital (Norfolk and Norwich University Hospitals NHS Foundation Trust), Beaumont Hospital (Royal College of Surgeons Ireland Hospital Group), University Hospital Limerick (The University of Limerick Hospital Group), Tallaght University Hospital (Dublin Midlands Hospital Group) and Galway University Hospital (Saolta University Healthcare Group). An overall six-month study timeframe was designated (October – March inclusive), within which each participating institution was requested to identify and complete a consecutive 3-4 month period of data collection. This timeframe was selected based on previous work showing relative consistency of catheter injuries over a six-month period [Citation5], with in-built flexibility to permit centers to select the period in which they could guarantee the highest quality of data collection based on local variables such as staffing. Data saturation was anticipated after this period given the multi-center design. Institutional ethics or audit committee approval was obtained at each site.
Outcome Measures
The primary outcome was the incidence of urethral catheter injuries occurring over the local study period. Secondary outcome measures were circumstances in which UC injury occurred, the nature of the urethral trauma, the acute urological management required and short-term clinical outcomes.
Identification of Urethral Catheter (UC) Injuries
All members of the urology team at each hospital site were educated with respect to the study protocol prior to commencement of the data collection period. Over the local study period, all cases of urethral catheter (UC) trauma referred to the on-call Urology team were identified and recorded. Data was prospectively logged in a central database at each institution.
Inclusion and Exclusion Criteria
A UC injury was determined to have occurred if the following criteria were met:
A urological consult was sought in the aftermath of a difficult and/or unsuccessful urethral catheterization attempt
One or more of the following symptoms or signs were observed:
Visible hematuria
The presence of blood at the urethral meatus
Urethral or perineal pain persisting post-catheterization attempt
A visible urethral injury at cystoscopy
Evidence of urethral trauma on urethrogram
and
The consulting urologist determined that a urethral injury had occurred
Cases of non-iatrogenic urethral trauma were excluded, including instances incurred from the use of self-intermittent catheters or from traumatic catheter dislodgement due to patient accident or agitation.
Data Recording
Data variables were recorded by the consulting urology team member, and included patient age and gender, the indication for catheterization, the hospital location at which UC injury occurred, the grade of staff member who performed/attempted catheterization and clinical sequelae of the UC injury.
Calculation of Incidence of Urethral Catheter Injuries
The incidence of UC injury was calculated using the hospital bed number as a proxy marker of the number of inpatient catheterizations performed per month, based on previous research deducing this figure from hospital procurement figures [Citation5]. Accordingly, the following formula was used:
with the injury incidence ultimately expressed per 1000 catheterizations.
Results
A study period of mean 3.43 (3-4) months was completed across seven institutions, during which a total of 66 urethral catheterization injuries were identified.
Patient Demographics
Patient demographics are presented in . All patients sustaining UC injury were male. The original indication for urinary catheter insertion was most commonly urinary retention (40.3%; 25/62).
Table 1. Population demographics.
Incidence of Urethral Catheter Injuries
The 66 injuries were interpreted in the context of the cumulative inpatient bed number across the participating sites, which was 3836 beds during the study timeframe. The UC injury incidence was calculated independently for each hospital site, based on local bed number and duration of data collection period and pooled, identifying an overall mean incidence of 6.2 injuries per 1000 catheterizations (6.2 ± 3.8 injuries; range 3.18-14.42/1000). As all urethral catheter injuries occurred in males, who account for 52.5% of catheterized patients [Citation1], an injury incidence of 6.2/525 or 11.81/1000 male catheterizations can be deduced.
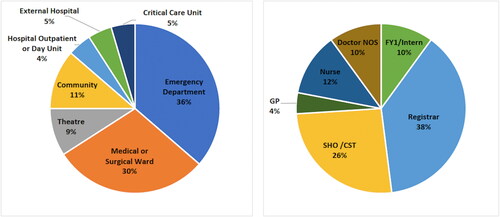
Circumstances of Injury
The healthcare location in which UC injury was sustained, and the role of the healthcare provider who made the initial catheterization attempt are presented in . In 8 instances, catheter attempts were made by more than one grade of doctor (Senior House Officer (SHO) followed by Registrar x 3; General Practitioner followed by Emergency Department SHO x 2; Foundation Year 1 doctor followed by SHO or Registrar x 2; Doctor of unspecified grade followed by Registrar x 1). In each of these instances, the role/grade of the first individual to attempt catheterization was reported in , based on the likely sequence of an initial UC injury resulting in subsequent failed catheterization attempts, although it is possible that trauma occurred during any one of these attempts. The number of catheterization attempts performed prior to consulting the urology service was recorded in 40 cases of UC injury: 1 attempt was made in 20% (n = 8); 2 attempts were made in 12.5% (n = 5); more than 2 attempts were made in 67.5% (n = 27) including 5 or more attempts in one-third of these (n = 9).
Acute Urological Management
The acute management approach enacted by the consulting urology team member upon diagnosis of a UC injury is presented in . Most patients (94.7%; 54/57) underwent further catheterization attempts, with use of a guidewire required in 22.8%, flexible or rigid cystoscopy required in 28.1% and placement of a suprapubic catheter required in 12.3% (via open cystotomy in 1).
Table 2. Acute management of UC injury.
Acute Clinical Outcomes
Free-text data responses regarding acute patient implications were sparse (referenced in 10/66 injuries). Of these, three patients were treated for infection, one of whom required transfer to the intensive care unit for management of urosepsis.
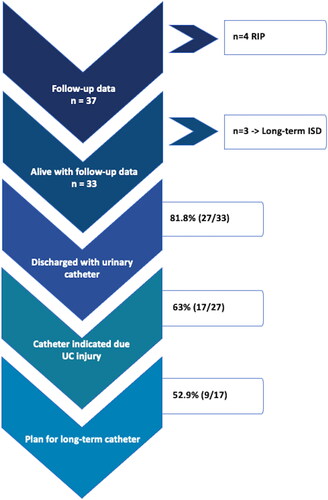
Short-Term Follow-Up
Short-term follow up data was available on 37/66 patients with UC injury (). Of these, 4 had died; it was not possible to confirm whether sequelae of the UC injury contributed to cause of death. Three patients were discharged with instruction to perform regular intermittent self-dilation (ISD). Twenty-seven patients (81.8%) were discharged with a urethral catheter in situ. Whilst a proportion of patients studied had long-term urethral catheters prior to UC injury, in 17/27 patients (63%) the decision to discharge with UC in situ was partly or fully attributable to the occurrence of urethral trauma. Of these 17 patients, a long-term plan for the patient to remain with an indwelling urethral or suprapubic catheter was made for 52.9% (n = 9).
Additional Healthcare Encounters
Of 30 patients for whom a plan was reported for clinical follow-up upon discharge, 90% (n = 27) were scheduled for a further healthcare encounter (such as interval trial without catheter, intermittent self-dilation education or interval cystoscopy) that may not have been required in the absence of the urethral injury.
Discussion
These results confirm that the previously identified UC injury rate of 6.7/1000 catheterizations [Citation5] is maintained across a multi-institutional setting, spanning UK and Irish national healthcare systems.
One previous US study reports a UC injury incidence of 3.2 per 1000 patient admissions [Citation4]; using a catheter prevalence of ∼20% in hospital inpatients [Citation1, Citation2], this can be translated to a higher approximate estimate of 16 injuries per 1000 catheterizations, or 1.6%. This is similar to the upper end of our incidence range (3.18-14.42/1000 catheterizations). We feel that the variability in our reported incidence range is likely underpinned by heterogeneity in local data collection methods and the vigilance of participating data collectors. Furthermore, both of the aforementioned studies, and our own, captured injury data from consultation requests directed to the local urology service alone. We chose this methodology for reasons of feasibility, however we do acknowledge the likelihood of associated underreporting, in that all patients sustaining catheter trauma may not have been referred to the urology service, and more ‘minor’ occurrences of trauma may not have been easily apparent to the consulting urologist. Therefore, whilst our figures highlight the significance and frequency of UC injury within healthcare systems, the true incidence may in fact be higher still.
An overall prediction of the volume of UC injury occurring in UK and Irish inpatient settings per annum can be estimated from this data. Based on NHS and HSE published figures (2020/2021), approximately 170,000 public inpatient beds exist across the UK, and 13,500 in Ireland [Citation6–10]. By interpreting the bed number as equal to the monthly catheterization figure, as explained in the methodology section, an approximate cumulative annual UC injury figure of 12,648 across UK and 1,004 across Irish public hospitals can be extrapolated.
Urological management of UC injuries was well-documented in this study, and it is evident that the majority of patients required some degree of specialist intervention. Seven patients (10.6%) required suprapubic catheter (SPC) placement, an intervention that imparts its own significant risks, particularly when necessitated in an emergency setting [Citation11, Citation12]. A limitation of our study was a lack of standardized data collection regarding the full spectrum of short-term morbidity. Previous work by Davis et al. identified a further complication of Clavien-Dindo grade 2 or above occurring in 81% of patients who sustained UC injury [Citation5]. In the current study, of 10 patients with available free-text data reporting their inpatient course, 30% (3/10) were treated for urinary tract infection, and 10% (1/10) required level 3 care due to urosepsis. Although this is a small data subset, findings do mirror the 32% (12/37) urosepsis rate in the aforementioned earlier study [Citation5]. This is unsurprising, given that 40% of patients studied required catheterization due to urinary retention. High residual urinary volumes are associated with bacteriuria with high bacterial titers, making patients vulnerable to sepsis in the instance of any breach of the urothelium [Citation13]. Prolonged hematuria, pain and extended length of stay are additional recognized complications that were not comprehensively explored [Citation5].
Whilst this study obtained short-term follow-up data only, long-term sequelae of catheterization-related urethral injuries have previously been studied. In one study, a cohort of patients identified as having sustained iatrogenic trauma during a catheterization attempt (n = 37), were analyzed at mean follow-up of 37 ± 3.7 months post-injury [Citation14]. The authors found 78% of these patients (29/37) to have developed urethral stricture disease with 27% of the cohort (10/37) remaining with an indwelling urethral or suprapubic catheter. Eight patients had died, with one death directly attributable to urosepsis secondary to a urethral catheterization injury [Citation14].
The results of our study highlight the propensity for UC injury to occur in a vulnerable patient cohort of older age groups (mean age 76.1, maximum 101 years). A significant proportion (25%) of injured patients had a long-term catheter, often a marker of co-morbidity, prior to the injury. These factors make patients particularly susceptible to complications such as sepsis and at increased risk from potentially necessary interventions requiring general anesthesia. Similarly, the ability to propose urethral reconstructive options to this cohort may be limited.
Alongside significant patient morbidity and potential mortality, the fiscal cost of catheterization-related trauma is substantial. Two Irish studies have quantified the financial output required to cover the acute patient management of UC injury, with estimates of short-term costs to the health service of €3,846–€9064 (USD $4,030-$9498; Pound Sterling £3261-£7685) per injury [Citation5, Citation15]. Using the median value of €6455 ($6764; £5473) per injury, and the predicted annual occurrences of UC injury calculated above, to estimate the cumulative national cost per annum of managing these injuries results in predictions in excess of €81.6 million ($85.51 million; £69.35 million) per annum across the UK and €6.48 million ($6.7million, £5.5 million) per annum in Ireland. It should be noted that these figures do not include costs of long-term patient management or potential medicolegal claims.
We acknowledge study limitations discussed above, including the possibility of heterogeneity in data collection methods between centers, possible variability in the identification of urethral catheterization injuries given the clinical nature of the diagnosis and the lack of standardized short and long-term complication data captured in this study. However, our data unequivocally identify a persistent problem of urethral catheterization injuries and highlight a pressing need to reflect upon transurethral catheterization practices and safety mechanisms. Despite the ubiquitous nature of urinary catheters within healthcare settings, it has previously been discovered that healthcare providers lack confidence in the procedure of catheter insertion, and perceive a lack of education and clinical supervision as barriers to gaining skills, knowledge and confidence [Citation16, Citation17]. Enhancing clinical education, therefore, emerges as a potential means to improving catheterization processes. Two previous studies have demonstrated that educational endeavors, such as catheter workshops, can effectively reduce the incidence of UC injury, but do not, however, eliminate it [Citation4, Citation18]. This prompts consideration of the issue through a broader lens. The possibility of integrating safety devices into routine catheter insertion practices is appealing, as an efficacious device could potentially nullify the risk of particular mechanisms of urethral injury, and provide reassurance and increased confidence to healthcare providers.
It is known that trauma arising from urethral catheterization arises most frequently from inadvertent intra-urethral inflation of the catheter anchoring balloon and/or false passage creation [Citation19]. Accordingly, a safety device targeting these mechanisms could be hypothesized to greatly reduce events of UC injury. Encouragingly, promising innovation in this field is beginning to emerge. The Urethral Catheterization Device (UCD)® (Urethrotech Ltd.) has been designed to integrate a hydrophilic Nitinol guidewire into a standard silicone urethral catheter, and has been proposed for use when first-line catheterization fails [Citation20]. The UCD has the potential to reduce false-passage creation and to increase success of second catheter attempts, although it does likely remain somewhat operator-dependent [Citation20]. To address the issue of intra-urethral balloon inflation, the Transurethal Catheter Safety Valve (TUCSV)TM has been designed by Class Medical. This novel safety device regulates the inflation pressure of a catheter’s anchoring balloon, and causes fluid within the catheter system to decant externally via the valve in the instance of a balloon being misplaced within the urethra, thereby preventing intra-urethral inflation. A pilot study (n = 100) has confirmed efficacy of the TUCSVTM, with 7 cases of valve venting (each suggestive of an injury avoided) and no UC injuries identified [Citation21].
A multifaceted approach, with enhanced clinical education and incorporation of safety mechanisms into standard catheterization practices on a systemic basis would almost certainly lead to a dramatic reduction in the incidence and significant consequences of UC injury highlighted by this study.
Conclusion
This multi-institutional study is the largest of its kind and spans two countries, incorporating different healthcare and clinical education systems. The results build upon earlier data to confirm that urethral catheter injury remains an under-recognized, important problem within medical practice, and recurs at an incredibly consistent rate across a variety of healthcare systems and geographical locations over time. Iatrogenic urethral injury is associated with significant patient morbidity and a large financial burden to the healthcare sector. These findings highlight a profound need to incorporate robust safety mechanisms into urinary catheterization procedures, in order to eliminate this recurrent medical error and its consequences.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Shackley DC, Whytock C, Parry G, et al. Variation in the prevalence of urinary catheters: a profile of National Health Service patients in England. BMJ Open. 2017;7(6):e013842. doi:10.1136/bmjopen-2016-013842.
- Jain P, Parada JP, David A, Smith LG. Overuse of the indwelling urinary tract catheter in hospitalized medical patients. Arch Intern Med. 1995;155(13):1425–1429.
- Leuck AM, Wright D, Ellingson L, Kraemer L, Kuskowski MA, Johnson JR. Complications of Foley catheters – Is infection the greatest risk? J Urol. 2012;187(5):1662–1666. doi:10.1016/j.juro.2011.12.113.
- Kashefi C, Messer K, Barden R, Sexton C, Parsons JK. Incidence and prevention of iatrogenic urethral injuries. J Urol. 2008;179(6):2254–2257; discussion 2257-8. doi:10.1016/j.juro.2008.01.108.
- Davis NF, Quinlan MR, Bhatt NR, et al. Incidence, cost, complications and clinical outcomes of iatrogenic urethral catheterization injuries: a prospective multi-institutional study. J Urol. 2016;196(5):1473–1477. doi:10.1016/j.juro.2016.05.114.
- Ewbank L, Thompson J, McKenna H, Anandaciva S, Ward D. NHS hospital bed numbers: past, present, future. England: The King’s Fund; 2021.
- Public Health Scotland. Acute hospital activity and NHS beds information (annual). Scotland: Public Health Scotland; 2021.
- Wales S. NHS beds summary data since 1989–90. Wales: Welsh Government; 2021.
- Michas F. Number of average available hospital beds in Northern Ireland from 2009 to 2021. Hamburg: Statista; 2021.
- DoH. Department of health open beds report for March 2021. Ireland: Department of Health; 2021.
- Hall S, Ahmed S, Reid S, et al. A national UK audit of suprapubic catheter insertion practice and rate of bowel injury with comparison to a systematic review and meta-analysis of available research. Neurourol Urodyn. 2019;38(8):2194–2199. doi:10.1002/nau.24114.
- Jane Hall S, Harrison S, Harding C, Reid S, Parkinson R. British Association of Urological Surgeons suprapubic catheter practice guidelines – revised. BJU Int. 2020;126(4):416–422. doi:10.1111/bju.15123.
- Caron F, Alexandre K, Pestel-Caron M, Chassagne P, Grise P, Etienne M. High bacterial titers in urine are predictive of abnormal postvoid residual urine in patients with urinary tract infection. Diagn Microbiol Infect Dis. 2015;83(1):63–67. doi:10.1016/j.diagmicrobio.2015.05.003.
- Davis NF, Bhatt NR, MacCraith E, et al. Long-term outcomes of urethral catheterisation injuries: a prospective multi-institutional study. World J Urol. 2020;38(2):473–480. doi:10.1007/s00345-019-02775-x.
- Bhatt NR, Davis NF, Addie D, et al. Evaluating the cost of iatrogenic urethral catheterisation injuries. Ir J Med Sci. Nov 2017;186(4):1051–1055. doi:10.1007/s11845-016-1451-5.
- Davis NF, Mooney RO, O’Brien MF, Walsh MT. Attitudes among junior doctors towards improving the transurethral catheterisation process. Ir J Med Sci. 2015;184(2):365–367. doi:10.1007/s11845-014-1120-5.
- Bhatt NR, Davis NF, Thorman H, Brierly R, Scopes J. Knowledge, skills, and confidence among healthcare staff in urinary catheterization. Can Urol Assoc J. 2021;15(9):E488–E494. doi:10.5489/cuaj.6986.
- Bhatt NR, Davis NF, Quinlan MR, et al. A prospective audit on the effect of training and educational workshops on the incidence of urethral catheterization injuries. Can Urol Assoc J. 2017;11(7):E302–E306. doi:10.5489/cuaj.4271.
- Thomas AZ, Giri SK, Meagher D, Creagh T. Avoidable iatrogenic complications of urethral catheterization and inadequate intern training in a tertiary-care teaching hospital. BJU Int. 2009;104(8):1109–1112. doi:10.1111/j.1464-410X.2009.08494.x.
- Bugeja S, Mistry K, Yim IHW, Tamimi A, Roberts N, Mundy AR. A new urethral catheterisation device (UCD) to manage difficult urethral catheterisation. World J Urol. 2019;37(4):595–600. doi:10.1007/s00345-018-2499-9.
- Davis NF, Cunnane EM, Mooney RO, Forde JC, Walsh MT. Clinical evaluation of a safety-device to prevent urinary catheter inflation related injuries. Urology. 2018;115:179–183. doi:10.1016/j.urology.2018.02.026.