Abstract
Purpose
Granulomatous lobular mastitis (GLM) is a benign inflammatory disease of the mammary gland with unknown etiology. Erythema nodosum (EN) is a rare, extramammary symptom of GLM. The purpose of this article was to investigate the clinical features of EN associated with GLM.
Methods
We recruited 102 GLM patients diagnosed between December 2018 and December 2021 at Renmin Hospital of Wuhan University. The clinical characteristics and laboratory indices of the EN group (n = 12) and the non-EN group (n = 90) were compared.
Results
The proportion of GLM patients with lesions involving ≥2 quadrants and high peripheral white blood cell count, absolute neutrophil count and neutrophil-to-lymphocyte ratio (NLR) was larger in the EN group than in the non-EN group (p = 0.002, 0.025, 0.014, 0.002, respectively). The duration of EN was longer in GLM patients with EN than in GLM patients without EN (p = 0.005). GLM patients with EN had more abscesses and sinus tracts than those without EN (p = 0.003, 0.038). Lesions involving ≥2 quadrants and the NLR were positively associated with the occurrence of EN (R = 0.304, 0.0302, p = 0.002, 0.002). Receiver operating characteristic curve analysis revealed that the area under the curve of the NLR was 0.770. When NLR > 5.73, the sensitivity and specificity of predicting EN were 66.67% and 87.78%, respectively.
Conclusion
Our findings suggest that GLM concomitant with EN suggests the presence of a more severe condition and extensive lesions.
Introduction
Granulomatous lobular mastitis (GLM) is a rare and complex pathologic breast condition with unknown etiology. Women of childbearing age are predisposed to GLM, particularly those who have given birth within the last 5 years.Citation1 Its clinical signs are diverse, including lumps, discomfort, local redness, swelling, abscess, sinus or fistula formation, and may emerge throughout the course of the disease.Citation2 Although it is a benign, inflammatory disease, its clinical and radiographical signs may mimic those of breast cancer. Pathological features of noncaseating granulomas and Langerhans giant cells around terminal mammary lobules are used to establish the diagnosis.Citation3 The three primary causes of GLM are hypothesized to be autoimmune disturbances, bacterial infections, and hormonal dysregulation (particularly elevated prolactin levels).Citation4
Erythema nodosum (EN) is a subcutaneous inflammatory disease predominantly characterized by tender erythematous nodules on the lower extremities.Citation5 Its typical pathological presentation is the infiltration of neutrophils and lymphohistiocytic cells in the subcutaneous adipose tissue of the interlobular septa.Citation5 Approximately 50% of EN cases are idiopathic, with other recognized etiologies including bacterial infections, medications, sarcoidosis, etc.Citation6 It was initially documented in 1987 as an uncommon extramammary sign of GLM by Adams et al.Citation7 In a systematic study of 3060 GLMs, the incidence of EN was 8%.Citation8 Although the coexistence is extremely unusual, it adds to the immunological explanation of GLM.
Despite recent efforts by certain researchers to define its clinical specificity,Citation9–11 the relationship between GLM and EN remains inconclusive. The purpose of this study was to increase physicians’ awareness of the clinical heterogeneity of GLM with EN by investigating and comparing the clinical aspects of GLM with and without EN.
Patients and methods
Materials
This study included 102 patients with GLM diagnosed at Renmin Hospital of Wuhan University from December 2018 to December 2021. The EN group consisted of 12 GLN patients with EN. The non-EN group consisted of 90 GLM patients without EN. Clinical characteristics, including age, reproductive history, breastfeeding history, past medical history, nipple deformity, GLM and EN disease course, lesion location and degree of involvement, ultrasound, routine blood tests, treatment methods, and treatment results, were acquired from the medical records system and the follow-up procedure. In all the patients, blood was drawn on an empty stomach for routine blood tests on the second morning following admission. The white blood cell count (WBC), absolute neutrophil count (ANC), absolute lymphocyte count (ALC), and platelet count (PLT) were obtained directly from routine blood tests. The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were obtained by calculating the ANC/ALC and PLT/ALC ratios separately. The Clinical Research Ethics Committee of Renmin Hospital of Wuhan University approved the study (WDRY2022-K067), and all patients provided informed consent.
Diagnosis
All patients were diagnosed pathologically by core needle aspiration biopsy or minimally invasive surgery with the Mammotome System. The histological results were confirmed by two pathologists. The presence of noncaseating granulomas, typical Langerhans giant cells, and epithelioid histiocytes around the terminal lobules in the mammary gland pathology led to the diagnosis of GLM. EN is diagnosed by the typical clinical presentation of erythematous, painful nodules in the lower extremities, especially in the anterior tibial region.
Treatment and follow-up
Abscess irrigation was performed in patients with apparent abscess formation. The operation was performed under ultrasound guidance with a Mammotome, a minimally invasive system for lesion biopsy. Indwelling hoses were placed in the lesion intraoperatively. The lesion was irrigated with normal saline, metronidazole, and dexamethasone through the indwelling hoses postoperatively. Patients without abscessed underwent core needle aspiration biopsy. The specific methods have been previously described. All patients received no other surgical treatment. Once the diagnosis was confirmed, all patients undertook an oral prednisone regimen with a starting dose of 15 mg/day. When the diagnosis was confirmed and local pus was completely drained, the patient was discharged and continued to receive oral medication in the outpatient clinic. The effectiveness of the medication was assessed according to symptoms, physical examination, and breast ultrasound. The dose was decreased to 10 mg/d when the mass began to shrink or soften and to 5 mg/d when the mass was significantly smaller or softer. Treatment was discontinued if: the patient’s symptoms disappeared, no palpable masses were observed, abscesses were healed, no sinus tracts or ulcers were found, and breast ultrasound showed a mass diameter < 1 cm and laboratory findings showed a WBC <7*10^9/L. Outpatient follow-up was performed every two weeks for the first 3 months after discharge and then every month thereafter for 3 months. After meeting the cure requirements, breast ultrasound should be performed at least once every six months. All patients received a breast physical examination and breast ultrasound at least once every six months after meeting the criteria for cure.
Efficacy evaluation
Clinical cure was defined as the disappearance of breast and extramammary symptoms on physical examination and imaging for more than 3 months. Clinical remission was defined as the relief of clinical symptoms and imaging showing that the lesions were more restricted than previously, but a clinical cure was not attained. The emergence of new lesions at the same location or a new site 3 months following clinical cure was regarded as recurrence.
Statistical analysis
IBM SPSS Statistics version 25.0 was used for statistical analysis. Chi-square and Fisher’s exact tests were used to compare qualitative data. Student’s t test was used to evaluate quantitative data that followed a normal distribution, and the Mann–Whitney U test was used to test data that did not follow a normal distribution. The connection of EN with clinical characteristics was determined using Spearman’s correlation analysis. Receiver operating characteristic (ROC) curve analysis was used to reveal the capacity of the NLR to predict the occurrence of EN. A P value < 0.05 was considered statistically significant.
Results
Clinical features of patients with EN
Twelve GLM patients with EN were aged 26 to 39 years (). All but one of them had given birth within 5 years. None of the patients had a history of hyperprolactinemia, autoimmune disorders, or antipsychotic medicines. Patients 2 and 5 tested negative for antinuclear antibodies, anti-extractable nuclear antigen antibodies, and anti-neutrophil cytoplasmic antibodies. Pus cultures in 11 individuals were negative during their hospitalization (91.7%). All patients continued oral prednisone therapy after discharge from the hospital and visited the outpatient clinic regularly for follow-up. The median duration of drug administration was 6.50 (2.0–13.0) months. The median follow-up time was 27.5 (11.0–30.0) months. Two patients developed ipsilateral or contralateral relapses during treatment and recovered well after retreatment with oral prednisone. All 12 patients have responded well to treatment thus far.
Table 1. Clinical characteristics of GLM with EN.
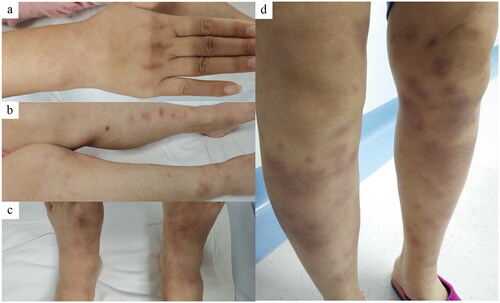
The most common site of EN involvement is the shins, followed by the knees, ankles, and forearms (). EN is most common approximately 4 wk following the onset of breast discomfort. Notably, all patients were in the abscess phase of the illness course at the time of EN presentation. On admission, Patient 4 had only a breast lump, and EN presented 12 wk after the onset of breast problems and when the lesions had become obvious abscesses. Although Patient 1 had no EN at the time of the initial onset of symptoms, it presented on the ipsilateral side and remained after 6 months of disease-free status. In Patient 6, the lesion first only affected the left breast (there was no EN at the time) and did not heal despite surgery in another institution. EN occurred 6 months later when a fresh lesion appeared in her right breast. In our study, only one patient (Patient 6) had concomitant arthritic manifestations. It presented as bilateral knee and elbow pain, which appeared almost simultaneously with erythema nodosum and disappeared subsequently after the disappearance of the erythema nodosum symptoms.
Comparison to GLM without EN
There were no statistically significant variations in baseline characteristics between the two patient groups (). The overall median follow-up time was 25.0 (8.0–43.0) months. The follow-up period did not differ statistically between the two groups (, p = 0.934). Lesions involving two or more quadrants were more common in GLM patients with EN (, p = 0.002). Furthermore, their peripheral blood indicators, including WBC, ANC, and NLR, were higher than those of the control group (p = 0.026, 0.014, 0.002, respectively, , ). The difference in PLR between the two groups was not statistically significant (p = 0.068, , ). The EN group had a lower ALC than the non-EN group (p = 0.014, , ). There was no significant difference in the relapse rate between the two groups (, p = 0.238). However, GLM patients with EN had a longer course than patients without EN (, p = 0.005), as well as a longer duration of prednisone use (, p = 0.024). In addition, patients in the EN group had a higher incidence of abscesses and sinus tracts than patients in the non-EN group (p = 0.003, 0.038, respectively, ).
Figure 2. Images of Case 7. (a-b) Breast appearance before and after treatment. Her left breast is erythematous and swollen with nipple retraction (a). There are scars of some pus drainage incisions on the surface, while the appearance is intact (b). (c–d) Ultrasound images before and after treatment. The normal glandular structure had almost disappeared, replaced by diffuse abscess formation (c). basically normal gland structure with a residual small hypoechoic area after treatment (d).
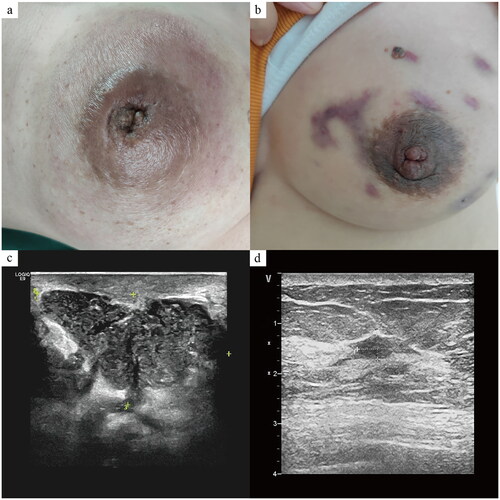
Figure 3. The comparison results of blood indicators. (a–c) WBC (white blood cell count), ANC (absolute neutrophil count), and NLR (neutrophil-to-lymphocyte ratio) of the EN group were higher than those of the non-EN group (p = 0.025, 0.014, 0.002, respectively). (d) ALC (absolute lymphocyte count) in the EN group was lower than in the non-EN group (p = 0.013). (e) The difference in PLR between the two groups was not statistically significant (p = 0.068). (f) The ROC curve analysis of NLR for the occurrence of EN. (*p < 0.05, **p < 0.01).
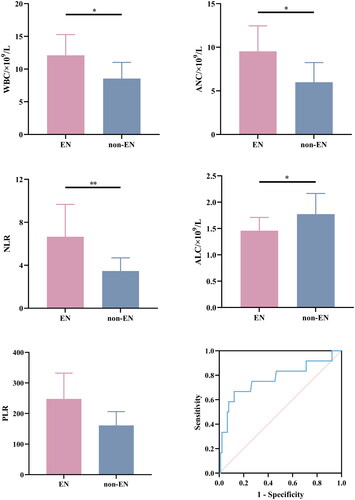
Table 2. Clinical and laboratory findings of GLM patients with and without EN.
Adverse events
The median duration of prednisone use for all participants in this study was 5.0 (1.0–13.0) months. A total of 22.5% (n = 23) of the patients experienced facial edema. Its incidence was higher in the EN group than in the non-EN group (, p = 0.025). Weight gain was observed in 42.2% (n = 43) of patients. A total of 8.8% (n = 9) of patients suffered from sleep problems, including difficulty falling asleep, early awakening, excessive dreaming, and insomnia. In addition, 5 patients complaining of hair loss during drug therapy. Apart from that, only one patient had emotional irritability while taking prednisone, which resolved after quitting the medication. There was no statistically significant difference in the prevalence of weight gain, hair loss, or sleep issues between the two groups. No more adverse events were reported.
Prediction of the occurrence of EN
To explore the potential predictors that can be used to predict EN, we performed a Spearman correlation analysis and plotted the ROC curve. Lesions involving ≥ 2 quadrants and high WBC, ANC and NLR were positively associated with the occurrence of EN (p = 0.002, 0.025, 0.014, 0.002, respectively, ). ALC was negatively correlated with the occurrence of EN (p = 0.013, ). The correlation between EN and lesions involving ≥ 2 quadrants and high NLR was stronger than with non-EN (R = 0.304, 0.0302, respectively). In the ROC curve, the AUC of the NLR was 0.770 (95%CI: 0.599–0.941, p = 0.002, ). When NLR > 5.73, the sensitivity and specificity of predicting EN were 66.67% and 87.78%, respectively.
Table 3. Spearman correlation coefficient based on EN.
Discussion
The etiology and pathogenesis of GLM have not been elucidated, thus making its clinical diagnosis and treatment difficult. In recent years, GLM has been hypothesized to be caused by autoimmunity. It has been suggested that local granulomatous inflammatory responses to antigens in luminal secretions following epithelial duct cell injury may be the pathogenesis of GLM.Citation12 Changes in cytokine levels suggest possible immune dysregulation in patients with GLM.Citation13–15 The diagnosis of EN was initially confirmed at the time that cutaneous pathological biopsy confirmed panniculitis. With increased awareness of this phenomenon, unnecessary skin biopsies can be avoided. In most recent studies, the diagnosis has been confirmed by the assessment of typical clinical symptoms, such as erythematous tender nodules on the lower extremities. The pathogenesis of EN is also unclear and thought to be mediated by hypersensitivity reactions. Therefore, it is proposed that EN may result from epitope spreading in breast tissue.Citation16
In this study, we reviewed the clinical features of 12 GLM patients with EN and compared them to 90 patients with GLM only. Despite the small sample size, we found some interesting phenomena. The interval between the occurrence of EN and the onset of breast symptoms reported in the literature varied widely. The peak of EN onset occurred approximately 4 wk after the presentation of breast symptoms. Notably, EN in all 12 patients occurred when breast lesions were in the abscess phase, although some patients may have been in the mass phase on admission. In this paper, the most common site of EN involvement was the bilateral pretibial regions and, less commonly, the ankles, knees, and forearms. Plantar EN was not observed, although it has also been reported in the literature.Citation17 More than half of the patients with EN experienced significant edema and pain in both lower extremities and were unable to walk. Nonsteroidal anti-inflammatory drugs such as indomethacin have been proven to be useful for EN, while GLM-induced EN seems to resolve with GLM-only therapy.Citation18,Citation19 It disappeared approximately 2 wk after taking prednisone based on a definitive GLM diagnosis in all 12 patients in this study. It has been reported that EN is self-limiting. However, we also observed that EN persisted for up to 6 wk in one patient with a delayed diagnosis. Therefore, improving the understanding of the correlation between GLM and EN, making an accurate and rapid diagnosis and implementing treatment measures are the keys to alleviating the suffering of patients.
There were no significant differences in baseline characteristics, including the age of onset, lesion location, reproductive history, breastfeeding, and nipple retraction, between the patients in the EN group and those in the non-EN group. Velideoğlu et alCitation11 reported that EN patients had a higher mean age of onset and a history of previous lactation, but Luo et al,Citation9 Çetin et al,Citation10 and all of our data contradicted this conclusion. We noted that most of the patients with EN in our study had given birth within 5 years, and none of the patients had a history of hyperprolactinemia or hyperprolactinemia-related psychiatric symptoms, although these findings were not significantly different from those of the control group.
Consistent with previous literature reports, EN seems closely related to the extensive involvement of breast lesions in patients with GLM. The proportion of patients with lesions involving ≥ 2 quadrants was higher than that in the control group in our study. It was positively correlated with the occurrence of EN, consistent with Luo et al’s conclusion.Citation9 Our results showed that there was no significant difference in the rate of bilateral breast lesions between the two groups, although this has been suggested by other scholars to be related to the occurrence of EN.Citation10 Laboratory findings such as WBC, ANC and NLR are easily attainable, require inexpensive noninvasive assessment, and are routinely used to evaluate systemic inflammation in clinical work. Their elevations tend to indicate more severe inflammation. WBCs were higher in the EN group than in the control group.Citation11 In this article, we also confirmed that ANC and NLR were higher in GLM patients with EN than in GLM only patients. The Spearman correlation coefficient between EN and NLR was higher than that between EN and the other indicators. By plotting the ROC curve, we found that when NLR > 5, its specificity for predicting the occurrence of EN was 80%, with a sensitivity of 87.78%, with a sensitivity of 66.67%. The results above indicate that EN is more likely to occur in patients with severe GLM.
Unlike the conclusions of retrospective studies published to date linking EN and increased NLR to the recurrence of GLM,Citation9,Citation11,Citation20 our study did not demonstrate this association. All EN-positive patients in this investigation responded well to therapy, and the recurrence rate was not significantly different from that of the control group. GLM patients with EN had a longer disease course than those without EN, which was consistent with the results found by Luo et al.Citation9 During the management of the enrolled patients, the dose of prednisone was tapered according to the efficacy of the drug. Our results also showed that the EN group used prednisone for a longer period of time than the non-EN group. Our findings further confirm that the incidence of abscesses and sinus tracts was higher in the EN group than in the non-EN group throughout the disease period.Citation9,Citation11 In 2021, Parperis et alCitation21 proposed the concept of GMENA (granulomatous mastitis, erythema nodosum, arthritis) syndrome based on the specific presentation of GLM with erythema nodosum and arthritis. Although there was only one EN-positive GLM patient in our study who had symptoms of arthritis, our findings support the inclusion of GLM with EN as a distinct clinicopathological entity.
In this study, we applied a low-dose prednisone-based treatment with a starting dose of 15 mg/d. Patients with significant abscesses on admission were treated with minimally invasive surgical cannulation and irrigation, and low-dose prednisone treatment was started postoperatively. Those who developed abscesses during the course of treatment underwent drainage procedures as appropriate. No additional medications were administered for the treatment of EN. In our study, the major adverse events related to drug use were facial edema, weight gain, sleep problems, and alopecia. There was no significant difference in the incidence of adverse events between the two groups, except for a higher proportion of patients with facial edema in the EN group than in the non-EN group. The recurrence rate for patients in this study was 7.8%, which is lower than the 15.4–24.8% reported in the literature,Citation22 suggesting that this is a safe and effective therapy.
Our study has several limitations. First, this is a retrospective study, and selection bias may exist. In addition, due to the incidence of disease, our sample size was small, thus limiting our further predictive analysis. The follow-up period despite the condition being likely to recur. A multicenter, prospective randomized clinical trial with a larger sample size is required to validate our results.
Conclusions
Our findings suggest that GLM patients with more severe inflammation and extensive lesions may be more prone to developing EN. EN is most likely to appear when a patient’s breast lesions have progressed to the abscess phase. GLM patients with EN have a longer disease course and a higher probability of developing abscesses and sinus tracts. Lesions involving more than 2 quadrants and an NLR > 5 might be potential indicators that can predict the occurrence of EN. These results suggest that early detection, early diagnosis, and early treatment of GLM may help to reduce the incidence of EN and that improving clinicians’ awareness of GLM combined with EN may shorten the duration of EN and alleviate the pain of patients. Whether EN is associated with recurrence requires further clarification through research.
Disclosure statement
The authors report there are no competing interests to declare.
References
- Otto TS, Argobi Y, Lerwill MJ, Smith GP, Fedeles F. A retrospective study of idiopathic granulomatous mastitis diagnosis and clinical presentation. J Am Acad Dermatol. 2022;86(2):1–8. doi:10.1016/j.jaad.2021.09.055.
- Shojaee L, Rahmani N, Moradi S, Motamedi A, Godazandeh G. Idiopathic granulomatous mastitis: challenges of treatment in Iranian women. BMC Surg. 2021;21(1):206. doi:10.1186/s12893-021-01210-6.
- Yin Y, Liu X, Meng Q, Han X, Zhang H, Lv Y. Idiopathic granulomatous mastitis: etiology, clinical manifestation, diagnosis and treatment. J Invest Surg. 2022;35(3):709–720. doi:10.1080/08941939.2021.1894516.
- Sheybani F, Naderi HR, Gharib M, Sarvghad M, Mirfeizi Z. Idiopathic granulomatous mastitis: long-discussed but yet-to-be-known. Autoimmunity. 2016;49(4):236–239. doi:10.3109/08916934.2016.1138221.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, Gomez-Flores M. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22(3):367–378. doi:10.1007/s40257-021-00592-w.
- Leung A, Leong KF, Lam JM. Erythema nodosum. World J Pediatr. 2018;14(6):548–554. doi:10.1007/s12519-018-0191-1.
- Adams DH, Hubscher SG, Scott DG. Granulomatous mastitis–a rare cause of erythema nodosum. Postgrad Med J. 1987;63(741):581–582. doi:10.1136/pgmj.63.741.581.
- Martinez-Ramos D, Simon-Monterde L, Suelves-Piqueres C, et al. Idiopathic granulomatous mastitis: a systematic review of 3060 patients. Breast J. 2019;25(6):1245–1250. doi:10.1111/tbj.13446.
- Luo W, Xu B, Wang L, et al. Clinical characteristics and predictive factors of erythema nodosum in granulomatous lobular mastitis. Australas J Dermatol. 2021;62(3):342–346. doi:10.1111/ajd.13640.
- Çetin K, Sıkar HE, Güllüoğlu BM. Idiopathic granulomatous mastitis with erythema nodosum: is it a variant of clinical presentation indicating treatment resistance? A retrospective cohort study. Breast J. 2020;26(9):1645–1651. doi:10.1111/tbj.13944.
- Velidedeoğlu M, Papila Kundaktepe B, Mete B, Uğurlu S. Idiopathic granulomatous mastitis associated with erythema nodosum may indicate a worse prognosis. Int J Rheum Dis. 2021;24(11):1370–1377. doi:10.1111/1756-185X.14218.
- Alungal J, Abdulla MC, Narayan R. Idiopathic granulomatous mastitis with erythema nodosum and polyarthritis. Reumatismo. 2016;68(2):97–99. doi:10.4081/reumatismo.2016.844.
- Saydam M, Yilmaz KB, Sahin M, et al. New findings on autoimmune etiology of idiopathic granulomatous mastitis: serum IL-17, IL-22 and IL-23 levels of patients. J Invest Surg. 2021;34(9):993–997. doi:10.1080/08941939.2020.1725190.
- Huang YM, Lo C, Cheng CF, Lu CH, Hsieh SC, Li KJ. Serum C-reactive protein and interleukin-6 levels as biomarkers for disease severity and clinical outcomes in patients with idiopathic granulomatous mastitis. J Clin Med. 2021;10(10):2077. doi:10.3390/jcm10102077.
- Koksal H, Vatansev H, Artac H, Kadoglou N. The clinical value of interleukins-8, -10, and -17 in idiopathic granulomatous mastitis. Clin Rheumatol. 2020;39(5):1671–1677. doi:10.1007/s10067-020-04925-8.
- Choi EC, Wong S, Ho SJ. Idiopathic granulomatous mastitis and erythema nodosum – a unifying pathophysiology. Australas J Dermatol. 2021;62(1):e149–e153. doi:10.1111/ajd.13463.
- Polat M, Kaya H. Plantar erythema nodosum associated with granulomatous mastitis. Indian J Dermatol Venereol Leprol. 2016;82(2):202–204. doi:10.4103/0378-6323.164219.
- Akın M, Karabacak H, Esendağlı G, et al. Coexistence of idiopathic granulomatous mastitis and erythemanodosum: successful treatment with corticosteroids. Turk J Med Sci. 2017;47(5):1590–1592. doi:10.3906/sag-1611-100.
- Gümüş M, Akkurt ZM, Gümüş H. Is erythema nodosum coexisting with lesions of the breast a suggestive sign for idiopathic granulomatous mastitis. Turk J Surg. 2018;34(1):71–73. doi:10.5152/turkjsurg.2017.3161.
- Çetinkaya ÖA, Çelik SU, Terzioğlu SG, Eroğlu A. The predictive value of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in patients with recurrent idiopathic granulomatous mastitis. Eur J Breast Health. 2020;16(1):61–65. doi:10.5152/ejbh.2019.5187.
- Parperis K, Achilleos S, Costi E, Vardas M. Granulomatous mastitis, erythema nodosum and arthritis syndrome: case-based review. Rheumatol Int. 2021;41(6):1175–1181. doi:10.1007/s00296-021-04820-8.
- Yuan QQ, Xiao SY, Farouk O, et al. Management of granulomatous lobular mastitis: an international multidisciplinary consensus (2021 edition). Mil Med Res. 2022;9(1):20. doi:10.1186/s40779-022-00380-5.