Abstract
Objective
To compare the clinical results of a new femoral neck system (FNS) and cannulated compression screws (CCS) for the treatment of femoral neck fractures in younger patients.
Methods
Retrospective study was performed in younger patients with femoral neck fractures that were treated with FNS or CCS from August 2017 to August 2022. The hip functional outcomes were assessed with the Harris hip score (HHS). Secondary outcomes included the surgical time, surgical blood loss, satisfaction visual analog scale (VAS), fluoroscopy frequency, fracture healing time and complications.
Results
A total of 49 patients (22 FNS and 27 CCS) with a minimum follow-up of 12 months were included. There was also no significant difference in HHSs (p = 0.27) and satisfaction VAS (p = 0.10) between them. Patients with FNS had more blood loss (50.45 ± 5.28 mL vs. 20.67 ± 4.71 ml, p < 0.01), lower fluoroscopy frequency (16.64 ± 3.32 vs. 23.59 ± 3.39, p < 0.01) and lower fracture healing time (3.76 ± 0.42 vs. 4.46 ± 0.59 months, p < 0.01). The femoral neck shortening and incidence of nail withdrawal in the FNS group was significantly lower than CCS group (2.91 ± 1.95 vs. 4.44 ± 1.52 mm, p < 0.01; 4.5% vs. 22.2%, p = 0.03).
Conclusions
The FNS and CCS get similar hip functions. The FNS can reduce fluoroscopy exposure and the complications such as femoral neck shortening and nail withdrawal. Thus, FNS can be an alternative to CCS for the fixation of femoral neck fractures in younger patients.
Introduction
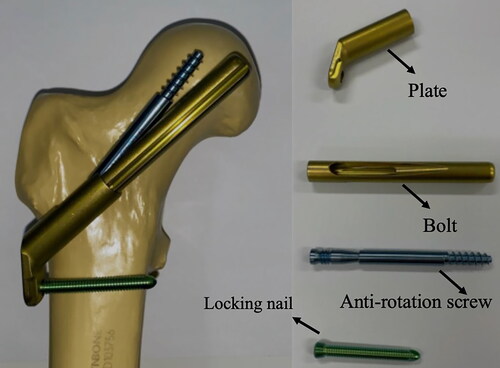
Femoral neck fracture is common in all hip fractures, and is considered as the orthopedic challenge because of the high incidence of avascular necrosis.Citation1 Femoral neck fractures (FNFs) occur mainly in elderly individuals and are attributed to low-energy violence. While for young patients (age < 65 years), femoral neck fractures are mainly caused by high-energy violence.Citation2 Surgery for young patients with femoral neck fractures aims to preserve the femoral head, achieve bone healing and avoid femoral head necrosis. The conventional treatments for preserving the femoral head include dynamic hip screws (DHS)Citation3 and cannulated compression screws (CCS).Citation4 However, there are some complications for these conventional treatments, such as nonunion, femoral head necrosis, and nail withdrawal.Citation5 A cadaveric study indicated that the inferior retinacular artery of the medial femoral artery plays an important role in the blood resource for the femoral head, and the injury of this artery following the femoral neck fracture or surgery may result in fracture nonunion or femoral head necrosis.Citation6 This situation causes huge socioeconomic burden and surgical challenges. Thus, the orthopedic doctors have to focus on reducing iatrogenic injury and complications during the operation, especially for young patients. Recently, the femoral neck system (FNS) has been developed as a new internal fixation technique for treating femoral neck fractures. Its advantages include angular stability, anti-rotation, dynamic fixation and minimal invasion.Citation7 This system has a plate with locking nail and a 10 mm bolt with anti-rotation screw. The anti-rotation screw locked into the bolt allows a relative slide between the fracture ends ().Citation8 However, it is still unknown whether FNS have advantages over CCS.
Therefore, this study compared the clinical efficacy of the FNS versus CCS for treating young patients with femoral neck fractures. This retrospective study purposes to determine whether the FNS has advantages over CCS regarding clinical efficacy.
Methods
Patients
This retrospective study were completed at Trauma Center of the First Affiliated Hospital of Anhui Medical University. Patients with femoral neck fracture between August 2017 and August 2021 was identified. The study was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University and conducted in accordance with the Helsinki Declaration of 1975 as revised in 2013.
Inclusion Criteria and Exclusion Criteria
All patients underwent surgical treatment and follow-up. Inclusion criteria were as follows: (1) age, 18–60 years; (2) unilateral closed fresh femoral neck fracture (fracture time < 3 wk); (3) fixation of the fracture with FNS or three CCSs; (4) follow-up time ≥12 months; and (5) availability of complete case data. Exclusion criteria: (1) long-term heavy alcohol use, long-term history of hormone drugs or femoral head necrosis; (2) other severe diseases; (3) pathological fractures; and (4) severe cognitive dysfunction. The xx patients were divided into two groups according to the surgical method: FNS and CS. Patients were treated with FNS or CS internal fixation. Sex, age, body mass index, fracture type and cause of injury were compared between the two groups as shown in .
Table 1. Patient demographics and characteristics [mean (SD)].
Preoperative Protocol
Before the surgery, patients were taken anteroposterior and lateral X-rays of the hip joint, and computed tomography (CT). Moreover, anticoagulant was used to prevent or treat the deep vein thrombosis. The surgical approach and decision were made by two experienced surgeons.
Surgical Technique
Patients were treated with spinal epidural or general anesthesia. The patient was placed in the supine position on an orthopedic traction table. After the C-arm X-ray machine confirmed that the fracture was in an adequate reduction position, conventional sterilization was performed. Fracture reduction quality was assessed using the Garden Index.Citation9
FNS group
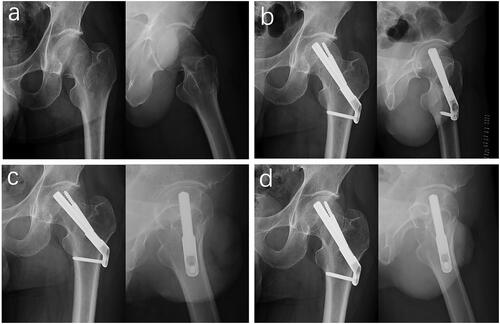
As described by Zhou et al.,Citation10 the operated limb was placed in an abducted, internally rotated position. A longitudinal incision of approximately 4 cm was made under the greater trochanter to reach the lateral femoral cortex (about 3–4 cm). First, an anti-rotation Kirschner wire was placed to maintain fracture reduction. The Kirschner wire was positioned as close to the upper margin of the femoral neck as possible, and the lateral position was far from the center of the femoral neck to avoid affecting the placement of FNS power rod. Then, a second guide wire was inserted as the central guide wire under the guidance of a localizer at 130°. The proper position of the guide wire was confirmed according to the image of the fluoroscopic C-arm machine. A measuring device was used to determine the length and the proper implant was chosen. The implant was inserted over the central guide wire into the pre-reamed hole. After satisfactory attachment of the lateral plate of the femur, 1–2 locking screws were inserted after drilling along the guide system. Finally, the anti-rotation screw channel of the guide was opened, and an anti-rotation screw of the appropriate length was inserted. Interfragmentary compression was applied by turning the insertion screw counterclockwise. The implant position was monitored during compression using the C-arm fluoroscopy guidance ().
CCS Group
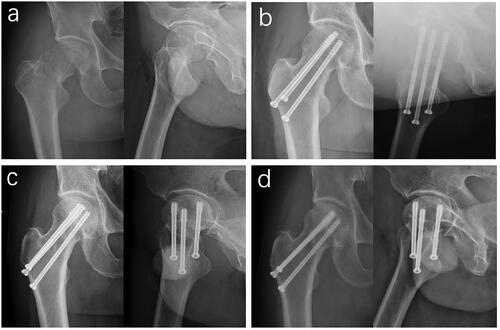
Three parallel guide pins were inserted into the femoral head along the longitudinal axis of the femoral neck in the shape of an inverted triangle under the C-arm fluoroscopy guidance. After the guide pins were in the correct position, three cannulated screws were inserted along the direction of the guide wire to fix the fracture. Notably, the position of screws should be higher than the lesser trochanter to reduce the concentration of stress and the distal thread should pass through the fracture line completely. The top of the screw should be 5–10 mm below the femoral head articular surface, and the screw should be as close to the cortex as possible ().Citation10
Postoperative Protocol
Postoperative multimodal analgesia and anti-coagulation using low molecular weight heparin were performed. The patients were encouraged to begin exercise within 24 h of the surgery. The next day, radiography and computed tomography were performed to determine reduction and internal fixation. By the second postoperative week, the patients started to exercise with the help of crutches without straight leg raises and weight-bearing activities, and mainly rest in bed. Partial weight-bearing exercise was encouraged at week 6, recovering to normal exercise based on the patient’s condition, followed by walking without crutches. X-ray follow-up was performed at 1, 3, 6, and 12 months after surgery and every 6 months thereafter. Hip function assessment was performed 6 and 12 months after the surgery.Citation11
Clinical Outcome Measure
All clinical data for the length of hospital stay, operative time, surgical blood loss, fluoroscopy frequency, length of stay, satisfaction visual analog scale (VAS), Harris hip score (HHS), fracture healing time, and incidence of postoperative complications (infection, femoral neck shortening, nonunion, femoral neck necrosis, nail withdrawal, cut out the internal fixation) were assessed and recorded. Femoral head necrosis and nonunion were judged according to the criteria described by Slobogean et al. and Dhar et al.Citation12,Citation13 The method of Zlowodzki et al. was used to identify femoral neck shortening.Citation14 Patients were asked to fill in a visual analog scale (VAS) to describe how satisfied they were with the result of the operation. The value 0 represented very satisfied while the value 100 represented very dissatisfied.Citation8 Hip function was assessed using the HHS which includes four domains: pain, function, degree of deformity, and range of motion of the joint assessed by the physiotherapist for deciding the patient’s hip function.Citation15 At the same time, according to the HHS system, clinical efficacy was graded as follows: 90–100, excellent; 80–89, good; 70–79, moderate; and < 70, poor.
Statistical Analysis
Continuous variables were expressed as mean ± standard deviation (SD) and were analyzed by Student’s t-test. The chi-square test was used to analyze categorical variables. Ranked data was tested by the Mann-Whitney U test. All statistical analyses were performed using SPSS 25.0 (SPSS Inc., Chicago, IL, USA). p < 0.05 were considered to be statistically significant.
Results
A total of 49 patients (22 FNS and 27 CCS) were included in the present study with the follow-up for a minimum of 12 months. The patient demographics data were given in . There were no significant differences between FNS and CCS groups in age, gender, body mass index, involved side, cause of injury, Garden classification, Pauwels classification, and follow-up time (all p > 0.05). No surgical failure were found during the operation both for these two groups.
No significant differences were found between the two groups in terms of surgical time, length of hospital stay and satisfaction VAS (p > 0.05). However, Patients who underwent FNS treatment had lower fluoroscopy frequency (16.64 ± 3.32 vs. 23.59 ± 3.39, p < 0.01) and more blood loss (50.45 ± 5.28 vs. 20.67 ± 4.71 mL, p < 0.01, ). The fracture healing time of 3.76 ± 0.42 months in the FNS group was significantly shorter than that of 4.46 ± 0.59 months in the CCS group (p < 0.01, ).
Table 2. Comparisons of surgical outcomes in the two groups [mean (SD)].
No significant differences in HHSs were found between the two groups (p = 0.27), but the HHSs of the CCS group were slightly lower than those of the FNS group (90.07 ± 5.54 vs. 88.18 ± 6.19, p = 0.27, ). Regarding the hip joint function, the excellent and good rates in FNS and CCS groups were 90.9% (20/22) and 88.9% (24/27).
Regarding postoperative complications, there was no significant difference in the incidence of femoral head necrosis, fracture nonunion and screw cutout between the two groups (). The incidence of nail withdrawal in the FNS group was significantly lower than that in the CCS group (4.5% vs. 22.2%, p = 0.03). Femoral neck shortening occurred in both groups after the surgery. The degree of femoral neck shortening in the FNS group was significantly lower than that in the CCS group (2.91 ± 1.95 vs. 4.44 ± 1.52 mm, p < 0.01, ).
Discussion
This study provides the clinical rationale that the FNS and CCS can get similar hip functional outcomes in the treatment of femoral neck fracture in younger patients. The results demonstrated that FNS is comparable to CCS with regard to the HHS. However, our study showed that the FNS was superior to CCS with respect to fluoroscopy frequency, fracture healing time and postoperative complications involving femoral neck shortening, nail withdrawal and screw cutout.
Evaluation of the HSS of FNS and CCS for the treatment of femoral neck fracture in younger patients demonstrated comparable outcomes in this study. Our results are in line with the previous data reporting comparable hip functional outcomes between FNS and CCS.Citation16,Citation17 Hu et al. compare the clinical outcomes of the hip joint after FNS versus CCS in a retrospective study with 44 younger patients and at least 12 months of follow-up and reported no significant difference regarding the HHS.Citation17 He et al. similarly evaluated 33 patients who underwent FNS and 36 patients who underwent CCS after more than 12 months, and found similar results regarding the HHS.Citation16 However, a meta-analysis indicates that FNS has higher HHS than CCS.Citation18 Similarly, Zhang et al. found a higher HHS in FNS than CCS in a retrospective study with 69 patients after the 6-month follow-up period.Citation19 However, it must be noticed that the follow-up period in the previous study was different from the present study, which may generate heterogeneity.
In accordance with other studies, the present study revealed comparable surgical time between FNS and CCS, but more intraoperative blood loss and lesser fluoroscopy frequency in FNS. These findings are confirmed by Tang et al. who reported a mean surgical time of 52.4 min for FNS, showing no difference compared to CCS with surgical time of 42.0 min.Citation11 Tian et al. Citation18 and Rajnish et al. Citation20 conducted a meta-analysis and reported that there were no significant differences in the surgical time between FNS and CCS, but statistically significant differences with lesser fluoroscopy frequency and more intraoperative blood loss in FNS group than the CCS fixation group. However, Zhang et al. found comparable intraoperative blood loss between FNS and CCS, and lower surgical time in FNS than CCS in a retrospective study with 69 patients.Citation19 He et al. retrospectively evaluated 69 patients and found higher surgical time in FNS than CCS.Citation16 The difference might be explained by differing surgical techniques, especially during preparation or insertion of the internal fixations.
The fracture healing time demonstrated a statistically lesser time required for the fracture union in FNS group than the CCS group of fixations. This finding goes along with a retrospective study operated by Hu et al. Citation17 who compared the fracture healing time of FNS to CCS with 44 younger patients, and reported shorter time in FNS group. Similarly, Tian et al.Citation18 and Rajnish et al.Citation20 conducted a meta-analysis and reported that the healing time in the FNS group was shorter than that in the CCS group. However, He et al. retrospectively evaluated 69 patients and found comparable fracture healing time between FNS and CCS.Citation16
The postoperative complications demonstrated comparable incidence of femoral head necrosis, fracture nonunion and screw cutout between FNS and CCS, but lower femoral neck shortening as well as lower incidence of nail withdrawal in the FNS group than CCS. These findings are in line with the previous data reporting incidence of femoral head necrosis and fracture nonunion between FNS and CCS.Citation11,Citation17 Hu et al. compared the complications of the hip joint after FNS versus CCS in a retrospective study with at least 12 months of follow-up, and reported no significant difference regarding the incidence of femoral head necrosis and fracture nonunion, but lower femoral neck shortening and screw cutout in the FNS group.Citation17 Tang et al. similarly evaluated 69 patients after more than 12 months, and found similar results regarding femoral head necrosis and fracture nonunion, but lower femoral neck shortening in the FNS group.Citation11 However, a meta-analysis indicates that FNS has a lower incidence of femoral head necrosis than CCS.Citation18 Tang et al. found similar incidence of screw cutout between FNS and CCS.Citation11
There are some limitations in the present study. First, this was a retrospective study which compared the FNS and CCS methods for treating young patients with femoral neck fractures. Thus, a randomized controlled trial (RCT) study design might give more insights into the complications of the FNS technique. Second, the small collection and the short follow-up in this study don’t represent a complete treatment process, which might limit our conclusions. Thus, a study with a larger scare is needed. Third, there was no biomechanical evidence in this study, so further studies should be focused on the biomechanical evaluation for providing strong evidence in choosing appropriate methods for treating young patients with femoral neck fractures.
Conclusions
According to the clinical outcomes of FNS and CCS for treating young patients with femoral neck fractures, the FNS and CCS get similar hip function with regard to the HHSs. However, the FNS needs fewer frequencies of intraoperative fluoroscopies and can reduce the complications such as nail withdrawal and femoral neck shortening. Thus, the FNS technique can be considered an alternative to CCS for treating young patients with femoral neck fractures.
Ethics Approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University and conducted in accordance with the Helsinki Declaration of 1975 as revised in 2013.
Informed Consent
Written informed consent was obtained from all participants.
Authors’ Contributions
Study conception and design: YSG, YC, DL; Acquisition, analysis and/or interpretation of data: YSG, YC, FL, FS; Drafting/revision of the work for intellectual content and context: YSG, FS; Final approval and overall responsibility for the published work: YSG, XH, FS. All authors read and approved the final manuscript.
| Abbreviations | ||
| FNS | = | femoral neck system |
| CCS | = | cannulated compression screws |
| VAS | = | satisfaction visual analog scale |
| HHS | = | Harris hip score |
| FNF | = | femoral neck fracture |
| DHS | = | dynamic hip screws |
| CT | = | computed tomography |
| SD | = | standard deviation |
| RCT | = | randomized controlled trial. |
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Song HK, Choi HJ, Yang KH. Risk factors of avascular necrosis of the femoral head and fixation failure in patients with valgus angulated femoral neck fractures over the age of 50 years. Injury. 2016;47(12):1–6. doi:10.1016/j.injury.2016.10.022.PMID:27793326.
- Samsami S, Augat P, Rouhi G. Stability of femoral neck fracture fixation: a finite element analysis. Proc Inst Mech Eng H. 2019;233(9):892–900. doi:10.1177/0954411919856138.PMID:31203740.
- Zhu J, Li Y, Zhang Y, Cheng X. Clinical outcome and biomechanical analysis of dynamic hip screw combined with derotation screw in treating displaced femoral neck fractures based on different reduction qualities in young patients (≤65 years of age). Biomed Res Int. 2022;2022:9505667–9505615. doi:10.1155/2022/9505667.PMID:35036442.
- Jiang D, Zhan S, Wang L, et al. Biomechanical comparison of five cannulated screw fixation strategies for young vertical femoral neck fractures. J Orthop Res. 2021;39(8):1669–1680. doi:10.1002/jor.24881.PMID:33034914.
- Xia Y, Zhang W, Zhang Z, Wang J, Yan L. Treatment of femoral neck fractures: sliding hip screw or cannulated screws? A meta-analysis. J Orthop Surg Res. 2021;16(1):54. doi:10.1186/s13018-020-02189-1.PMID:33446230.
- Putnam SM, Collinge CA, Gardner MJ, Ricci WM, McAndrew CM. Vascular anatomy of the medial femoral neck and implications for surface plate fixation. J Orthop Trauma. 2019;33(3):111–115. doi:10.1097/bot.0000000000001377.PMID:30562252.
- Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–137. doi:10.1097/bot.0000000000000739.PMID:27755333.
- Ben Bouzid Y, Bassir RA, Boufettal M, et al. Minimally invasive technique in the management of tibial pilon fractures: new approach and promising results. Adv Orthop. 2023;2023:1272490–1272495. doi:10.1155/2023/1272490.PMID:36999045.
- Karanicolas PJ, Bhandari M, Walter SD, et al. Interobserver reliability of classification systems to rate the quality of femoral neck fracture reduction. J Orthop Trauma. 2009;23(6):408–412. doi:10.1097/BOT.0b013e31815ea017.PMID:19550226.
- Zhou XQ, Li ZQ, Xu RJ, et al. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg. 2021;13(6):1802–1809. doi:10.1111/os.13098.PMID:34351048.
- Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504. doi:10.1186/s13018-021-02659-0.PMID:34399801.
- Slobogean GP, Stockton DJ, Zeng B, Wang D, Ma BT, Pollak AN. Femoral neck fractures in adults treated with internal fixation: a prospective multicenter Chinese cohort. J Am Acad Orthop Surg. 2017;25(4):297–303. doi:10.5435/jaaos-d-15-00661.PMID:28248692.
- Dhar SA, Gani NU, Butt MF, Farooq M, Mir MR. Delayed union of an operated fracture of the femoral neck. J Orthop Traumatol. 2008;9(2):97–99. doi:10.1007/s10195-008-0012-8.PMID:19384623.
- Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163–169. doi:10.1097/01.ta.0000241143.71274.63.PMID:18188116.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. 5783851 doi:10.2106/00004623-196951040-00012.
- He C, Lu Y, Wang Q, et al. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord. 2021;22(1):994. doi:10.1186/s12891-021-04888-0.PMID:34844578.
- Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. doi:10.1186/s13018-021-02517-z.PMID:34107990.
- Tian P, Kuang L, Li ZJ, Xu GJ, Fu X. Comparison between femoral neck systems and cannulated cancellous screws in treating femoral neck fractures: a meta-analysis. Geriatr Orthop Surg Rehabil. 2022;13:21514593221113533. doi:10.1177/21514593221113533.PMID:35832467.
- Zhang YZ, Lin Y, Li C, et al. A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-Up. Orthop Surg. 2022;14(4):686–693. doi:10.1111/os.13235.PMID:35179307.
- Rajnish RK, Srivastava A, Rathod PM, et al. Does the femoral neck system provide better outcomes compared to cannulated screws fixation for the management of femoral neck fracture in young adults? A systematic review of literature and meta-analysis. J Orthop. 2022;32:52–59. doi:10.1016/j.jor.2022.05.007.PMID:35601207.