Abstract
Objective
To construct and internally validate a nomogram that predicts the likelihood of postoperative delirium in a cohort of elderly individuals undergoing hip arthroplasty.
Methods
Data for a total of 681 elderly patients underwent hip arthroplasty were retrospectively collected and divided into a model (n = 477) and a validation cohort (n = 204) according to the principle of 7:3 distribution temporally. The assessment of postoperative cognitive function was conducted through the utilization of The Confusion Assessment Method (CAM). The nomogram model for postoperative cognitive impairments was established by a combination of Lasso regression and logistic regression. The receiver operating characteristic (ROC) curve, calibration plot, and decision curve analysis (DCA) were used to evaluate the performance.
Results
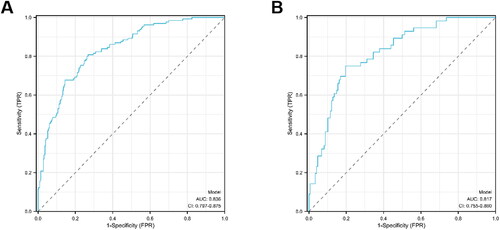
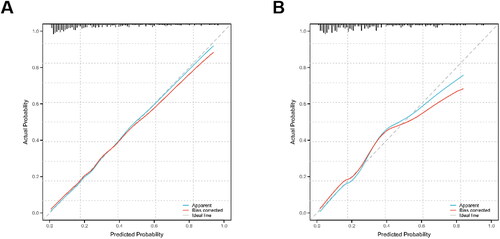
The nomogram utilized various predictors, including age, body mass index (BMI), education, preoperative Barthel Index, preoperative hemoglobin level, history of diabetes, and history of cerebrovascular disease, to forecast the likelihood of postoperative delirium in patients. The area under the ROC curves (AUC) for the nomogram, incorporating the aforementioned predictors, was 0.836 (95% CI: 0.797–0.875) for the training set and 0.817 (95% CI: 0.755–0.880) for the validation set. The calibration curves for both sets indicated a good agreement between the nomogram’s predictions and the actual probabilities.
Conclusion
The use of this novel nomogram can help clinicians predict the likelihood of delirium after hip arthroplasty in elderly patients and help prevent and manage it in advance.
Keywords:
Introduction
Postoperative delirium (POD) is a neurological complication commonly observed in elderly patients following surgery, characterized by the emergence of postoperative cognitive deficits. These deficits are manifested through fluctuating impairments in attention and disorientation, typically occurring within one week of the surgical procedure and potentially persisting for an extended duration. Furthermore, the presence of POD has been linked to the development of Alzheimer’s disease [Citation1]. Importantly, this condition is strongly associated with unfavorable outcomes, including an elevated likelihood of reoperation, prolonged hospitalization, increased healthcare expenses, temporary impairment in daily functioning, and heightened long-term mortality [Citation2]. Compared with various surgical procedures, the prevalence of POD is significantly increased in patients undergoing joint replacement [Citation3], and approximately 5-31% of patients experience POD after joint replacement [Citation4]. Postoperative delirium is influenced by multiple factors, including personal and family factors, social-related factors, disease-related factors, and trauma-related factors [Citation5–7].
Previous clinical trials have conducted preliminary investigations into the correlation between hip arthroplasty and postoperative delirium, identifying various perioperative risk factors. Xu Xiaohong et al. [Citation8] found that advanced age, long operation time, general anesthesia, resuscitation time ≥ 1 h, postoperative pain score ≥ 4 points, postoperative hypoxemia, and high CRP level at 4 h after operation were all risk factors for postoperative delirium in elderly THA patients, and thus established a prediction model that could assist clinicians in screening high-risk groups. Wang Biao et al. [Citation9] found that elevated preoperative serum PGE2 concentration was an independent risk factor for the incidence of POD after hip fracture surgery in elderly patients, and had a high predictive ability for the occurrence of POD. However, further research is necessary to elucidate the underlying causes of postoperative delirium in elderly patients undergoing hip arthroplasty [Citation10,Citation11]. The accurate prediction of postoperative delirium and timely and efficient intervention are crucial steps in mitigating this issue [Citation12]. Moreover, the Confusion Assessment Method (CAM) serves as a specific tool for diagnosing the presence of delirium in postoperative patients. According to the CAM, the construction of a predictive model has the potential to elucidate the association between hip arthroplasty and postoperative delirium, as well as facilitate the implementation of targeted preventive strategies by clinicians, thereby enabling the formulation of personalized treatment plans [Citation13]. Currently, nomograms have found extensive application in the medical field for the simultaneous diagnosis of oncological and non-oncological multicriteria, as well as for predicting the onset and progression of diseases [Citation14–16]. Nomograms transform intricate regression equations into visual graphs, thereby enhancing the readability and convenience of predictive modeling results for patient assessment [Citation17]. The utilization of nomograms in identifying high-risk patients enables the implementation of early and aggressive remedial interventions, thereby mitigating the overall risk and benefiting the patient [Citation18].
The objective of this study was to create a straightforward yet efficient predictive instrument that could offer significant clinical and nursing insights into the prevention and management of postoperative delirium among elderly patients undergoing hip arthroplasty. This was achieved through the collection and analysis of clinical data, with the aim of identifying the factors that contribute to the occurrence of postoperative delirium in this specific patient population.
Materials and methods
Study design and participants
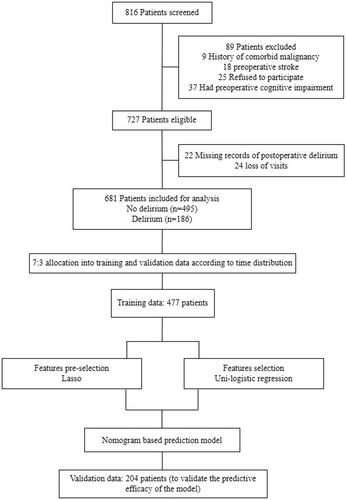
This study was approved by the Ethics Committee of our hospital and conducted in accordance with the principles outlined in the Declaration of Helsinki. Data were collected from a nationwide sample of elderly patients (≥60 years old) who underwent hip arthroplasty at our hospital between January 2017 and June 2023. Inclusion criteria encompassed patients who chose elective hip arthroplasty, and written informed consent was obtained from all patients and their family members. The study implemented specific exclusion criteria, which encompassed the following factors: (1) presence of preoperative cognitive dysfunction or a prior history of psychotropic drug utilization; (2) existence of preoperative contraindications to surgical intervention; (3) inability to actively engage in the study or evaluate patients for postoperative delirium; (4) previous occurrence of comorbid malignancy; (5) mortality during hospitalization; and (6) absence of visits or insufficient availability of patient clinical information within medical records. Modeling and validation were carried out according to the time sequence and the allocation principle of 7:3. The process of inclusion and exclusion of study subjects is shown in .
Clinical feature data collection
The retrospective clinical data encompassed various patient characteristics, such as age, sex, BMI, education, smoking and alcohol consumption, preoperative Barthel index, preoperative hemoglobin level, and preoperative cerebral bispectral index. Additionally, the medical history of patients was considered, including hypertension, diabetes mellitus, cerebrovascular disease, coronary artery disease, pulmonary disease, and renal disease. Furthermore, intraoperative conditions were taken into account, such as the duration of surgery versus anesthesia, fluid balance, intraoperative cerebral bispectral index, and administration of anesthesia medication, as well as the time required for awakening from anesthesia.
Delirium assessment
The study employed the Confusion Assessment Method (CAM) to evaluate the prevalence of postoperative psychosis among elderly individuals undergoing hip arthroplasty. The CAM comprises four elements, namely (1) Acute onset and fluctuating change in condition, encompassing the identification of abrupt deterioration in mental state relative to the patient’s baseline level, as well as the assessment of behavioral fluctuations from one day to another, with varying symptom intensity; (2) Impaired concentration: This pertains to the patient’s challenges in maintaining focus, characterized by susceptibility to distractions and an inability to sustain engagement with a discussed topic; (3) Disordered thinking: This encompasses instances where the patient’s thought processes exhibit confusion or incoherence, such as the dispersion of the conversation’s subject matter or its detachment from the ongoing discourse, unclear or illogical thinking patterns, or abrupt transitions between topics without prior indication; (4) The assessment of alterations in consciousness involves determining whether the patient’s current level of consciousness deviates from the norm, exhibiting symptoms such as hyper-vigilance, somnolence, or lethargy. The diagnosis of delirium is based on the presence of feature 1, along with the presence of features 2 and either 3 or 4, resulting in a positive Confusion Assessment Method (CAM) score. A qualified clinical neuropsychologist completed the evaluation process for all patients within 24 h after the surgical procedure and subsequently generated the appropriate outcome report [Citation19].
Statistical analysis
Statistical analyses and data processing were performed using SPSS 21.0 and R (version 4.2.1). Measurement data were first analyzed by K-S test, measurement data with normal distribution were expressed as mean ± standard deviation, and t-test was used for comparison between groups. Those not following a normal distribution were presented as medians (interquartile range), and comparisons between groups were performed using the Mann-Whitney-U test. Enumeration data were expressed as n (%) and compared between groups using the chi-square test. The least absolute shrinkage and selection operator (LASSO) regression model was used to identify the optimal predictive risk factors associated with postoperative delirium in patients. According to the results of Lasso regression, the multivariate logistic regression model was used to identify risk factors and establish a nomogram model for the risk of postoperative delirium. The discriminative performance of the nomogram was assessed using the area under the receiver operating characteristic curve (AUC). Calibration curves were plotted to assess the calibration of the model. Calibration was assessed using the Hosmer-Lemeshow Goodness of Fit test, and a non-significant result (p > 0.05) indicated a satisfactory model fit. Statistical significance was defined as a two-tailed p-value < 0.05.
Results
Patients and clinical characteristics
Between January 2017 and June 2023, a cohort of 818 patients was recruited for participation in this study. Subsequently, 681 patients were subjected to data analysis after undergoing screening based on the predetermined inclusion/exclusion criteria (). Among the analyzed patients, 53.5% were identified as female, with a mean age of 69.6 years (ranging from 60 to 94 years). In the training set, the overall rate of postoperative delirium was 27.3% (130 of 477 patients). In the validation set, this rate was slightly higher at 27.5% (56 of 204 patients). Demographic information and clinical characteristics of patients showed significant differences between groups in age, BMI, education, diabetes, cerebrovascular disease, preoperative Barthel index, and preoperative hemoglobin (p < 0.05) ().
Table 1. Demographics and clinical characteristics.
Feature selection
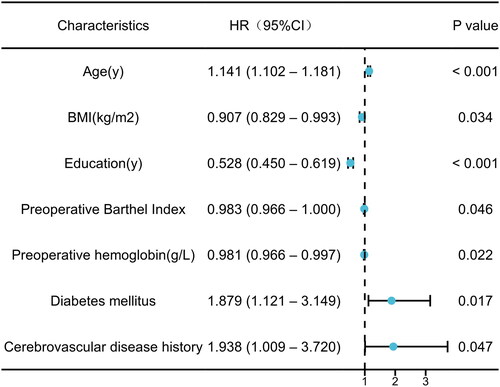
Lasso regression was used to screen all these variables. A total of 27 characteristics were narrowed down to 7 potential predictors through the examination of demographics, preoperative comorbidities, intraoperative situations, and the utilization of nonzero coefficients. These predictors, namely age, BMI, education, preoperative Barthel index, preoperative hemoglobin level, history of diabetes mellitus, and cerebrovascular disease ( and ).
Figure 2. Demographic and clinical feature selection using the lasso binary logistic regression model.
Note: Lasso, least absolute shrinkage and selection operator; SE, standard error.
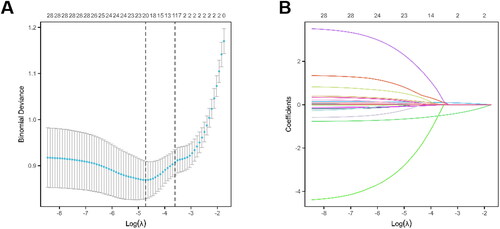
Table 2. Prediction factors for postoperative delirium in elderly patients undergoing hip arthroplasty.
Construction of nomogram model for postoperative delirium
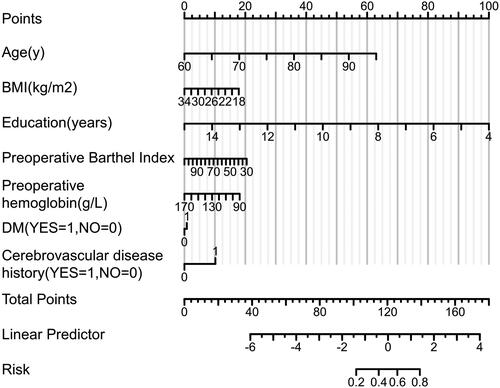
The variables screened by Lasso regression were used for multivariable logistic regression analysis. Univariate Lologistic regression analysis showed that age, BMI, education, preoperative Barthel index, preoperative hemoglobin level, history of diabetes mellitus, and cerebrovascular disease were independent risk factors for postoperative delirium (p < 0.05, ). Multivariate Lologistic regression analysis showed that age, BMI, education, and preoperative hemoglobin levels were statistically significant (p < 0.05, and ). Additionally, a nomogram prediction model was developed to illustrate the relationship between these risk factors ().
Evaluation and validation of the postoperative delirium nomogram model
As shown in the ROC curve in , the AUC for the nomogram was 0.836 (95% CI: 0.797–0.875) for the training set (). The total point value (-1.096) with the highest Youden index was selected as the cutoff point of the ROC curve, with the corresponding specificity of 73.2% and sensitivity of 80.8%. The AUCs of the nomogram model were 0.817 (95% CI: 0.755–0.880) in the validation set, with the corresponding specificity of 80.4% and sensitivity of 75.0% (). The calibration curves generated by the nomogram exhibited strong concordance between observed outcome frequencies and predicted probabilities in both training and validation sets ().
Discussion
In this study, a total of seven variables were employed to forecast the likelihood of postoperative delirium in patients. It was observed that over 27% of the patients experienced postoperative delirium. To further investigate this phenomenon, a nomogram was constructed through risk factor analysis. The results of this analysis indicated that age, BMI, education, preoperative Barthel index, preoperative hemoglobin level, history of diabetes mellitus, and cerebrovascular disease may play significant roles as potential factors in the development of postoperative delirium.
Several prior studies have demonstrated that age is a significant risk factor for postoperative delirium in patients. This particular study indicates that advancing age is associated with an increased likelihood of developing delirium following major surgeries, particularly traumatic orthopedic procedures like hip fracture surgeries or hip arthroplasties. The occurrence of delirium in these elderly patients often leads to unfavorable outcomes, including prolonged hospitalization, escalated healthcare expenses, and elevated rates of readmission subsequent to discharge [Citation20].
A potential association exists between a lower body mass index (BMI) and the onset of delirium. In the case of older individuals requiring long-term care for hip disease, those who exhibited emaciation and low defatted body weight had a higher likelihood of developing delirium. This correlation may be attributed to the protective influence of a higher BMI on postoperative delirium (POD), potentially mediated through cerebrospinal fluid biomarkers (T-tau and P-tau) [Citation21].
Surprisingly, the level of patient education emerged as the most influential factor impacting the occurrence of postoperative delirium. This finding suggests that individuals with lower educational attainment may experience a higher incidence and greater severity of postoperative delirium, potentially due to social disadvantages. The lack of access to quality educational resources among the majority of individuals born in the 1960s in China resulted in a limited number of highly educated individuals who demonstrated cognitive abilities surpassing their age. This prevailing circumstance persisted until the implementation of compulsory education, which did not witness significant enhancements [Citation22,Citation23].
The preoperative Barthel index serves as an indicator of an elderly patient’s self-care proficiency in their daily activities, thereby reflecting their level of frailty. Our findings indicate a negative correlation between lower scores and the likelihood of developing delirium following hip arthroplasty. Moreover, the presence of delirium exacerbates the decline in a patient’s self-care abilities, thereby impacting their prognosis. In light of these results, we propose that elderly patients scheduled for elective hip arthroplasty should focus on conditioning their physical strength during the preoperative period as a preventive measure against delirium [Citation24,Citation25].
A noteworthy finding emerged, indicating a correlation between preoperative hemoglobin levels of patients and the occurrence of postoperative delirium. Specifically, lower hemoglobin levels exhibited a higher likelihood of being associated with postoperative delirium. A recent retrospective cohort study provided evidence that a preoperative hemoglobin level below 10 g/dl was associated with a higher likelihood of major adverse cardiac events following hip fracture surgery in patients aged 80 years and older. Additionally, a prospective multicenter observational study indicated that postoperative anemia might contribute to the risk of both postoperative delirium and an extended hospital stay [Citation26,Citation27]. Our analysis of anesthesia records revealed a potential correlation between low preoperative hemoglobin levels and the occurrence of intraoperative and postoperative hypotension, whether transient or persistent. Additionally, we found that perioperative hypotension was closely linked to the development of postoperative delirium, emphasizing the importance of maintaining hemodynamic stability to prevent this condition [Citation28,Citation29].
Numerous studies, including large-sample database analyses and clinical trials, have consistently reported a connection between diabetes and cognitive decline over the years [Citation30,Citation31]. Additionally, diabetes is known to induce vascular damage, modify signaling in inflammatory vesicles, disturb neuronal mitochondrial homeostasis, and impact the microbiota-metabolite-brain axis, among other mechanisms [Citation32–34]. The likelihood of postoperative delirium in elderly patients undergoing hip arthroplasty is comparable between those with a history of cerebrovascular disease and those with a history of diabetes mellitus. Research has shown that previous episodes of transient ischemia independently increase the risk of postoperative delirium, and even asymptomatic ischemia can predict its occurrence. These findings emphasize the significance of prioritizing prevention and treatment of postoperative delirium in patients with cerebrovascular disease [Citation35,Citation36].
This study is subject to several limitations. Firstly, the sample consisted exclusively of elderly patients, and there was a lack of data regarding the patients’ social attribute characteristics. However, previous research has demonstrated that disparities in income and subjective social status can also impact cognitive functioning, potentially leading to the development of delirium following hip arthroplasty in elderly patients with lower incomes and subjective social identities [Citation37–39]. Additionally, the inclusion of single-center studies in our research allows for a narrower focus on specific risk factors for postoperative delirium in patients. However, to broaden the scope of our findings, we plan to conduct multicenter trials in the future. Moreover, while the nomogram’s robustness was confirmed through validation, it is crucial to validate its effectiveness in a larger population of elderly patients undergoing hip arthroplasty to ensure its applicability on a broader scale.
Conclusion
This study presents a valuable nomogram that enables clinicians to promptly identify risk factors associated with postoperative delirium in elderly patients undergoing hip arthroplasty. By accurately predicting individual patients’ risk, both physicians and patients’ families can implement appropriate measures during the perioperative period to mitigate the occurrence of postoperative delirium and ultimately improve patients’ prognosis.
Authors’ contribution
ZY and XLJ contributed to the supervision of data collection, data analysis, manuscript drafting, and manuscript review. WRJ and ZQ were responsible for manuscript preparation. ZCL designed the manuscript, provided expertise in surgical content, supervised data collection, and conducted data analysis. DWT and ZMX assisted in the supervision of data collection and contributed to the final manuscript editing. LXH designed the manuscript, provided expertise in anesthesiologic content, supervised data collection, conducted data analysis, and contributed to manuscript drafting and review. All authors approved the final version of the manuscript.
Ethics approval
The Ethics Committee of the First Affiliated Hospital of Bengbu Medical College approved this study (approval number: 2022KY108). All research methods were conducted by the Declaration of Helsinki.
Acknowledgements
Not applicable.
Disclosure statement
The Authors declare that there is no conflict of interest.
Additional information
Funding
References
- Thiele RH, Theodore DJ, Gan TJ. Outcome of organ dysfunction in the perioperative period. Anesth Analg. 2021;133(2):393–405. doi:10.1213/ANE.0000000000005603.
- Evered L, Atkins K, Silbert B, et al. Acute peri-operative neurocognitive disorders: a narrative review. Anaesthesia. 2022;77 Suppl 1:34–42. doi:10.1111/anae.15613.
- Kitsis P, Zisimou T, Gkiatas I, et al. Postoperative delirium and postoperative cognitive dysfunction in patients with elective hip or knee arthroplasty: a narrative review of the literature. Life (Basel). 20220;12(2):314. doi:10.3390/life12020314.
- Chen JR, Chen JQ, Hu JC, et al. Cigarette smoking is linked to an increased risk of delirium following arthroplasty in patients suffering from osteoarthritic pain. CNS Neurosci Ther. 2023;29(12):3854–3862. doi:10.1111/cns.14306.
- Wang YY, Yue JR, Xie DM, et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on Postoperative Delirium and Function in Older Adults: A Randomized Clinical Trial. JAMA Intern Med. 2020;180(1):17–25. doi:10.1001/jamainternmed.2019.4446.
- O’Hanlon S, Baxter M, Hosie A. Postoperative delirium in older patients with cancer: the role of psychological distress and social support. Curr Opin Support Palliat Care. 2022;16(1):38–47. doi:10.1097/SPC.0000000000000588.
- Pedemonte JC, Sun H, Franco-Garcia E, et al. Postoperative delirium mediates 180-day mortality in orthopaedic trauma patients. Br J Anaesth. 2021;127(1):102–109. doi:10.1016/j.bja.2021.03.033.
- Xu XH, Xu Q, Xu BL, et al. Construction and validation of false risk prediction model after hip arthroplasty in elderly patients. J Wannan Medical College. 2022;41(06):588–591. doi:10.3969/j.issn.1002-0217.2022.06.021.
- Wang B, Wang LY, Ji MH. Risk factors for delirium after hip replacement in elderly patients. J Clinic Anesthesiol. 2022;38(07):688–692. doi:10.12089/jca.2022.07.003.
- Chen D, Li Y, Li Q, et al. Risk factors and a nomogram model establishment for postoperative delirium in elderly patients undergoing arthroplasty surgery: a single-center retrospective study. Biomed Res Int. 2021;2021:6607386–6607389. doi:10.1155/2021/6607386.
- Rong X, Ding ZC, Yu HD, et al. Risk factors of postoperative delirium in the knee and hip replacement patients: a systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):76. doi:10.1186/s13018-020-02127-1.
- Viramontes O, Luan Erfe BM, Erfe JM, et al. Cognitive impairment and postoperative outcomes in patients undergoing primary total hip arthroplasty: a systematic review. J Clin Anesth. 2019;56:65–76. doi:10.1016/j.jclinane.2019.01.024.
- Kong H, Xu LM, Wang DX. Perioperative neurocognitive disorders: a narrative review focusing on diagnosis, prevention, and treatment. CNS Neurosci Ther. 2022;28(8):1147–1167. doi:10.1111/cns.13873.
- Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–1174. doi:10.1001/jama.2017.12067.
- Wu J, Zhang H, Li L, et al. A nomogram for predicting overall survival in patients with low-grade endometrial stromal sarcoma: a population-based analysis. Cancer Commun (Lond). 2020;40(7):301–312. doi:10.1002/cac2.12067.
- Zhang W, Ji L, Wang X, et al. Nomogram predicts risk and prognostic factors for bone metastasis of pancreatic cancer: a population-based analysis. Front Endocrinol (Lausanne). 2021;12:752176. doi:10.3389/fendo.2021.752176.
- Hu M, Shu X, Yu G, et al. A risk prediction model based on machine learning for cognitive impairment among chinese community-dwelling elderly people with normal cognition: development and validation study. J Med Internet Res. 2021;23(2):e20298. doi:10.2196/20298.
- Wang X, Lu J, Song Z, et al. From past to future: bibliometric analysis of global research productivity on nomogram (2000–2021). Front Public Health. 2022;10:997713. doi:10.3389/fpubh.2022.997713.
- van der Wulp K, van Wely MH, Rooijakkers MJP, et al. Delirium after TAVR: crosspassing the limit of resilience. JACC Cardiovasc Interv. 2020;13(21):2453–2466. doi:10.1016/j.jcin.2020.07.044.
- Hughes CG, Boncyk CS, Culley DJ, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative delirium prevention. Anesth Analg. 2020;130(6):1572–1590. doi:10.1213/ANE.0000000000004641.
- Deng X, Qin P, Lin Y, et al. The relationship between body mass index and postoperative delirium. Brain Behav. 2022;12(4):e2534. doi:10.1002/brb3.2534.
- Arias F, Chen F, Fong TG, et al. Neighborhood-level social disadvantage and risk of delirium following major surgery. J Am Geriatr Soc. 2020;68(12):2863–2871. doi:10.1111/jgs.16782.
- Ye X, Zhu D, Ding R, et al. The effect of China’s compulsory education reforms on physiological health in adulthood: a natural experiment. Health Policy Plan. 2022;37(3):376–384. doi:10.1093/heapol/czab147.
- Gracie TJ, Caufield-Noll C, Wang NY, et al. The association of preoperative frailty and postoperative delirium: a meta-analysis. Anesth Analg. 2021;133(2):314–323. doi:10.1213/ANE.0000000000005609.
- Sieber F, Gearhart S, Bettick D, et al. Edmonton frailty scale score predicts postoperative delirium: a retrospective cohort analysis. BMC Geriatr. 2022;22(1):585. doi:10.1186/s12877-022-03252-8.
- Li M, Chen C, Shen J, et al. Preoperative hemoglobin <10 g/DL predicts an increase in major adverse cardiac events in patients with hip fracture over 80 years: a retrospective cohort study. Geriatr Orthop Surg Rehabil. 2023;14:215145932311836. doi:10.1177/21514593231183611.
- Kunz JV, Spies CD, Bichmann A, et al. Postoperative anaemia might be a risk factor for postoperative delirium and prolonged hospital stay: a secondary analysis of a prospective cohort study. PLoS One. 2020;15(2):e0229325. doi:10.1371/journal.pone.0229325.
- Wachtendorf LJ, Azimaraghi O, Santer P, et al. Association between intraoperative arterial hypotension and postoperative delirium after noncardiac surgery: a retrospective multicenter cohort study. Anesth Analg. 2022;134(4):822–833. doi:10.1213/ANE.0000000000005739.
- Maheshwari K, Ahuja S, Khanna AK, et al. Association between perioperative hypotension and delirium in postoperative critically ill patients: a retrospective cohort analysis. Anesth Analg. 2020;130(3):636–643. doi:10.1213/ANE.0000000000004517.
- Casagrande SS, Lee C, Stoeckel LE, et al. Cognitive function among older adults with diabetes and prediabetes, NHANES 2011–2014. Diabetes Res Clin Pract. 2021;178:108939. doi:10.1016/j.diabres.2021.108939.
- Callisaya ML, Beare R, Moran C, et al. Type 2 diabetes mellitus, brain atrophy and cognitive decline in older people: a longitudinal study. Diabetologia. 2019;62(3):448–458. doi:10.1007/s00125-018-4778-9.
- Liu Z, Dai X, Zhang H, et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat Commun. 2020;11(1):855. doi:10.1038/s41467-020-14676-4.
- Tang W, Li Y, He S, et al. Caveolin-1 alleviates diabetes-associated cognitive dysfunction through modulating neuronal ferroptosis-mediated mitochondrial homeostasis. Antioxid Redox Signal. 2022;37(13-15):867–886. doi:10.1089/ars.2021.0233.
- Ward R, Li W, Abdul Y, et al. NLRP3 inflammasome inhibition with MCC950 improves diabetes-mediated cognitive impairment and vasoneuronal remodeling after ischemia. Pharmacol Res. 2019;142:237–250. doi:10.1016/j.phrs.2019.01.035.
- Ma X, Chu H, Han K, et al. Postoperative delirium after transcatheter aortic valve replacement: An updated systematic review and meta-analysis. J Am Geriatr Soc. 2023;71(2):646–660. doi:10.1111/jgs.18104.
- Shibagaki K, Shirasaka T, Sawada J, et al. Silent cerebral ischemia detected by magnetic resonance imaging can predict postoperative delirium after total arch replacement for aneurysm. JTCVS Open. 2022;10:87–96. doi:10.1016/j.xjon.2022.02.026.
- Rodriguez TM, Sheffler P, Ferguson LE, et al. Cognitive and functional improvement via novel skill learning for low-income minoritized middle-aged and older adults. Prev Sci. 2023;24(5):926–935. doi:10.1007/s11121-022-01413-0.
- Zhang F, Fung H, Kwok T. Spouse’s subjective social status predicts older adults’ prospective cognitive functioning. Aging Ment Health. 2019;23(2):277–285. doi:10.1080/13607863.2017.1406449.
- Liu Y, Liu Z, Liang R, et al. The association between com′munity-level socioeconomic status and cognitive function among Chinese middle-aged and older adults: a study based on the China Health and Retirement Longitudinal Study (CHARLS). BMC Geriatr. 2022;22(1):239. doi:10.1186/s12877-022-02946-3.