 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Social care is an integral part of the UK welfare system and plays an imperative role in promoting the well-being of older people. This study investigates the impacts of receiving informal social care on formal social care use among community-dwelling older people in England before and after the implementation of the Care Act 2014. Data came from the Health Survey for England for the years 2011 to 2018 (N = 17,292). Bivariate probit models were used to address the endogeneity issue. The analysis shows that receipt of informal care substitutes for formal care. Informal care had a strong substitution effect on formal personal care before 2015, which was significantly weakened after 2015. While the receipt of formal personal care has been increasingly “carer-blind,” that of formal domestic care depends on the availability of informal carers and personal affordability, which may result in unmet care needs.
Introduction
Social care provides hands-on assistance to people experiencing a decline in their capability to perform daily activities and is crucial to the well-being of older people. In most advanced welfare states, older people receive formal social care provided by professional caregivers, informal care (also known as unpaid care) provided by family, friends and neighbors, or both. Nearly 18,000 organizations across England provide formal social care (Skills for Care, Citation2022). It is estimated that 5.0 million unpaid caregivers provide care for older people (Brimblecombe et al., Citation2018).
In the context of population aging, the number of older people receiving social care is likely to experience unprecedented growth. Demand for formal social care in England is projected to increase by 55%, from 0.7 million people to 1.0 million people, and demand for informal care is projected to increase by 46%, from an estimated 2.1 million people to 3.0 million people in the next two decades (Hu et al., Citation2020). Meanwhile, the rise in the supply of informal care may not keep up with that of demand for informal care (Brimblecombe et al., Citation2018). To make sure that care resources for people with care needs are sufficient, it is important to understand how demand for formal social care responds to changes in informal care.
This study investigates the relationships between formal and informal social care in community-dwelling older people in England. We focus on the period between 2011 and 2018 and aim to answer two research questions: First, does the receipt of informal social care substitute for that of formal social care? Second, has this relationship changed since the implementation of the Care Act 2014? So far, little research has been done to examine these issues in the English context in this period. Moreover, the Care Act 2014 has introduced major reforms to the social care system, aiming to rebalance the demand for and supply of social care for older people (see below). An investigation into the second research question will provide useful information about whether policy intentions have translated into real changes in care patterns.
Policy context
In England, formal social care for older people is not free-of-charge at the point of use. Financial support from the government, funded through tax and managed by local authorities, is available only to people who are assessed as having eligible care needs. In addition, like some advanced welfare states such as Italy and Spain, eligibility for government support is subject to a financial assessment (i.e., means test) of incomes and savings. In the case of England, community-dwelling older people with capital above the upper threshold of £23,250 meet all their care costs. People with capital between the upper threshold and a lower limit of £14,250 are qualified to receive financial support from the government. They contribute toward care costs based on an assessment of income, and every £250 of capital are assumed to generate £1 of notional income. People with capital below the lower limit still contribute from their income, but the assumption of notational income does not apply (Hancock et al., Citation2022). The government recently announced plans to substantially increase the capital thresholds and introduce a lifetime cap on care users’ liability to contribute toward their care costs (HM Government, Citation2021).
People who do not meet the eligibility criteria in the needs-based and financial assessments have to purchase care out of pocket from private providers on the care market or rely on unpaid care. Those who purchase care privately are known as “self-funders”. There are no official statistics on the number of self-funders in England, and the sparse figures reported in the academic literature vary. An estimated 33% to 50% of all home care recipients are entirely self-funded (Forder, Citation2007; Hu et al., Citation2020; Institute of Public Care, Citation2012).
The Care Act 2014 introduced substantial changes to the social care system from April 2015, placing particular emphasis on equity, quality, and timeliness of care and support. Before the Care Act 2014, the assessment of care needs followed the Fair Access to Care Services (FACS) guidelines, which classified older people’s care needs into four categories: critical, severe, moderate, and low care needs. The levels of care needs that were eligible for financial support were determined at the discretion of local authorities, which resulted in great variations across England (Fernandez et al., Citation2013). Most importantly, some local authorities took into consideration whether people were receiving care from informal caregivers at the time of needs assessment. This meant that people with similar levels of functional capability might be considered as having different levels of care needs. As a result, some people living with a family carer or receiving informal care might not receive any publicly funded care and support at all (Comas-Herrera et al., Citation2010). This was known as a “carer sighted” system.
One of the main objectives of the Care Act 2014 was to amend the carer-sighted nature of the system on the grounds of distributive fairness (Comas-Herrera et al., Citation2010). In the process of needs assessment, eligibility determination is stipulated to be independent of the receipt of informal care and to depend exclusively on a set of quality-of-life outcomes such as managing nutrition and personal hygiene and maintaining a habitable home environment (Social Care Institute for Excellence, Citation2015). Guidance issued by the Department of Health and Social Care (Citation2022) states that:
During the assessment, local authorities must consider all of the adult’s care and support needs, regardless of any support being provided by a carer. Where the adult has a carer, information on the care that they are providing can be captured during the assessment, but it must not influence the eligibility determination.
The Care Act 2014, therefore, aims to guide the system to move in a more “carer-blind” direction, so that the input of unpaid care is disregarded during the assessment process. It is only after the needs assessment and for those who are judged to be eligible for public support that the availability of informal care comes into the equation: the amount of support provided to care recipients can be influenced by the level of care received from informal carers.
Literature review
An important issue in the literature on the relationship between informal and formal social care is the two-way interaction between these two forms of care. On the one hand, the receipt of informal care may affect the willingness of older people to receive, and the decision of local authorities to provide, formal care (Van Houtven & Norton, Citation2004). On the other hand, informal carers may change their decision to provide informal care if the people they care for are eligible for publicly funded care or prefer to receive formal support (Kim & Lim, Citation2015; Moussa, Citation2019; Saloniki et al., Citation2019; Stabile et al., Citation2006; Zigante et al., Citation2021). In empirical research, steps are taken to address this issue of endogeneity and disentangle the potentially two-way causal relationships between formal and informal care.
Empirical studies have shown that informal care substitutes formal care. Van Houtven and Norton (Citation2004) found that receipt of informal care reduces home health care use and delays nursing home entry in older people in the USA. This substitution effect has also been found in later studies conducted in England (Urwin et al., Citation2019), Continental Europe (Bolin et al., Citation2008; Bonsang, Citation2009), Japan (Hanaoka & Norton, Citation2008), and Canada (Sun et al., Citation2019; Zhang et al., Citation2021).
However, the relationship between formal and informal social care may vary once the focus shifts to subgroups of the older population. Drawing on longitudinal data collected in England between 1991 and 2009, Urwin et al. (Citation2019) found that the substitution effect was stronger among state-funded than privately funded home care recipients. Bonsang (Citation2009) reported that the substitution effect tends to be stronger in older people with a lower level of care needs or if the formal care provided is unskilled. Bolin et al. (Citation2008) found that the substitution effect tends to be more salient in Southern than Central and Northern Europe. They argued that such a cross-country variation can be explained by the stronger family ties in Southern Europe. A study conducted by Hanaoka and Norton (Citation2008) shows that the (potential) supply of informal care has a strong substitution effect on formal care among older people living with unmarried children with a lower level of education because this group of caregivers has a lower opportunity cost of time. Lemmon (Citation2020) reported that informal care for Scottish older people complements personal care services. Personal care in Scotland is free of charge.
Based on the existing literature and policy context in England, this study tests two hypotheses. First, we expect that receipt of informal care substitutes for formal care in the older population in England. Second, the Care Act 2014 aims to attenuate the carer-sighted nature of public support in England. A large proportion of formal home care recipients are state-funded and thus are directly affected by the Care Act 2014. Therefore, our second hypothesis is that the substitution effect of formal care on informal care in the older population is weaker after than before 2015.
Methods
Dataset
The data in this study came from the Health Survey for England (HSE), an annually recurring national survey carried out by the team of the Health and Social Survey Research Group and the Department of Epidemiology at University College London with NatCen Social Research since 1991 (NHS Digital, Citation2022). The survey consists of core questions that are asked every year and specific modules of questions that vary from year to year. The response rates in different years ranged from 56% to 64%. A module focusing on social care for older people aged 65 and over has been included since 2011. We used data collected between 2011 and 2018, and the total sample size was 17,292. It should be noted that the HSE did not follow the same cohort but collected a new nationally representative sample each year. Therefore, the analysis was based on pooled cross-sectional data rather than panel data.
Key variables of interest
The dependent variables in our study were the receipt of formal social care. The HSE asked survey participants whether they were able to perform seven activities of daily living (ADLs) and five Instrumental Activities of Daily Living (IADLs). The former relates to personal care tasks, while the latter concerns domestic care tasks. The ADL tasks included getting in and out of bed, bathing, dressing, using the toilet, eating, getting around indoors, and using the stairs. The IADL tasks included taking medication, getting out of the house, shopping for food, doing housework, and managing finance. For each task, survey participants chose from four options: “I can do this without help”, “I have difficulty doing it but can manage on my own”, “I can only do this with help”, and “I cannot do this”. People with difficulties in performing an ADL or IADL task were asked whether they received help with that task from formal caregivers. Based on these questions, we created three variables relating to formal care receipt: receiving formal care for IADLs tasks only, receiving formal care for any ADL tasks, and receiving formal care for any IADL or ADL tasks. They are all dichotomized variables (0 = no formal social care; 1 = receiving formal social care).
In the literature, formal ADL care is also known as formal personal care, and formal IADL care is also called formal domestic care or formal practical care (Kröger, Citation2022). We will use these terms interchangeably in this paper. The HSE asked different questions concerning the sources of funding for formal care between 2011 and 2018. The information collected in different years was neither comparable nor consistent, so we were not able to break down our sample into state-funded users and self-funders.
Two key independent variables were of interest. First, the HSE questionnaire asked survey participants whether they received help from informal caregivers with each of the ADL or IADL tasks. People receiving informal help with any ADL or IADL tasks were coded as “1.” Otherwise, they were coded as “0.” Second, we included a time dummy variable in the analysis. People who took part in the survey between 2011 and 2014 were coded as “0,” and those taking part between 2015 and 2018 were coded as “1.”
Control variables
Following the behavioral model of care utilization, we controlled for need, predisposing, and enabling factors in the analysis (Andersen & Newman, Citation2005). We investigated three need factors: functional capability, long-term illness, and self-reported health. The functional capability variable had four categories: no functional disabilities (independent), needing help with IADL tasks or having difficulties in performing ADL tasks (mild disability), needing help with one or two ADL tasks (moderate disability), and needing help with three or more ADL tasks (severe disability). The survey asked whether the respondents had longstanding physical or mental illnesses such as problems with vision, hearing, mobility, mental health, and learning. We created a binary variable: 0 = no and 1 = yes. Survey participants were asked to evaluate their health on a five-point Likert scale: “very good,” “good,” “fair,” “bad,” or “very bad.” We created an ordinal variable with three categories: very good or good health, fair health, and bad or very bad health.
In terms of socio-demographic variables, we looked at age, gender, marital status, living arrangement, and ethnicity. Age is a categorical variable with five-year age bands. Marital status has two categories: single (never married, widowed, separated, or divorced) and married. The living arrangement variable was dichotomized: 0 = living alone and 1 = living with others. The ethnicity variable was dichotomized: 0 = white ethnicity and 1 = minority ethnicity.
We looked into three enabling factors: educational qualifications, housing tenure, and receipt of pension credit. The education variable has three categories: no educational qualification, secondary education or lower, and higher education degree or equivalent. Housing tenure is a binary variable: 0 = owned housing and 1 = rented housing. In England, pension credit provides financial support to people over the state pension age and on a low income. The receipt of pension credit, therefore, indicates the economic status of older people and their potential eligibility for publicly funded formal social care. We created a dichotomized variable: 0 = no and 1 = yes.
Statistical analysis
We conducted regression analyses to test the two hypotheses of our study. We built the bivariate probit model to investigate the impacts of informal care receipt on formal care receipt. Such a model has frequently been used when both the outcome and the potentially endogenous regressor are binary variables (Carrieri et al., Citation2017; Elgazzar, Citation2009; Lo Sasso & Johnson, Citation2002). The full model was specified as follows:
is an index function: if the event in the bracket is true,
; otherwise
.
indicates the receipt of formal social care for an older person i. We investigated formal care for IADL tasks only and formal care for any ADL tasks, respectively.
denotes the receipt of informal care and
denotes the time dummy. We included an interaction term between the receipt of informal care and the time dummy to examine whether the impacts of informal care on formal care vary over time (Hypothesis 2).
denotes a vector of exogenous independent variables that appear in both equations.
, βk, and
are the coefficients of the independent variables, and
and
are the latent error terms that are assumed to be jointly normal:
We conducted the Wald χ2 test of the covariance of the two latent errors . If
is significantly different from 0, this indicates that
is an endogenous variable that should be accounted for by a bivariate probit model. It is worth mentioning that a bivariate probit model can rely only on functional form for model identification. A series of studies have shown that the identification of the bivariate probit model can be achieved even without including instrumental variables in the reduced form equation (Greene, Citation2011, pp. 785–787; Monfardini & Radice, Citation2008; Wilde, Citation2000). This is different from the linear regression models that rely on the inclusion of instrumental variables in a two-stage least-square procedure to achieve identification. Coefficient, robust standard error, and two-tailed significance level of the z-statistic for each independent variable (*p < .05, **p < .01, ***p < .001) in the first equation are presented in the main text. Estimates in the second equation are less relevant to our research questions and thus are reported in the appendix (Tables A1 and A2). The proportion of missing values is 2.8% (n = 492) in the pension credit variable and is less than 0.4% in all other variables. We conducted regression analyses on the completed cases. Details about the missing values are reported in the appendix (Table A5).
Results
Among the 17,292 people aged 65 and over in the HSE 2011–2018, 2% (n = 377) received formal social care only, 16% (n = 2,815) received informal care only, and 4% (n = 721) received both formal and informal care (). Among the 1,098 people receiving formal social care, 55% (n = 599) received care for IADLs only and 45% (n = 499) received care for ADLs. Of the 3,536 people receiving informal care, 46% (n = 1,636) received care for IADLs only and 54% (n = 1,900) received care for ADLs. Around 49% (n = 8,515) of the sample participated in the survey before 2015 (i.e., HSE 2011–2014), and 51% (n = 8,777) were after 2015 (i.e., HSE 2015–2018).
Table 1. Characteristics of the HSE sample aged 65 years old and over.
shows that 54% of the sample were females and 44% were aged 75 and over. Among the 17,292 people, 35% were living alone and 60% were married. More than two-thirds of the sample (69%) did not report any ADL or IADL limitations, 18% had a mild disability (needing help with IADLs or having ADL difficulties), 9% had a moderate disability (needing help with one or two ADLs), and 4% had a severe disability (needing help with three or more ADLs). In addition, 67% of the people reported at least one type of longstanding illness and 13% thought that their health was bad or very bad. One-fifth of the sample lived in rented housing. One-tenth of the sample received pension credit. About half of the sample (46%) had no educational qualifications, and 13% had higher education degrees or equivalent.
Column 3 shows the factors associated with the receipt of formal social care. The coefficient of informal care receipt was negative and statistically significant, which means that the receipt of informal care reduced the likelihood of receiving formal social care. For people receiving formal care for IADLs only, the coefficient of informal care was also negative and significant ( Column 4). For people receiving formal care for ADLs, the coefficient was negative but showed no statistical significance ( Column 5). The time dummy was not statistically significant in any of the three models. We conducted analyses on different subgroups of the sample and found that the negative association between formal and informal social care remained (Table A4 in the appendix).
Table 2. Factors associated with receipt of formal social care (bivariate probit models without the interaction term).
Most of the control variables were strongly associated with the receipt of formal social care (). Age was positively associated with the likelihood of receiving formal care. Married people and those living with other people in the same household were less likely to receive formal care. All three need variables were significantly associated with the receipt of formal care. People with a higher level of functional disability, longstanding illness, or poor self-reported health were more likely to receive formal care. People with a higher level of education were more likely than those without educational qualifications to receive formal domestic care. People living in owner-occupied housing were more likely than those in rented housing to receive formal domestic care (i.e., formal care for IADLs). The receipt of pension credit was the only variable that had no statistical significance in any of the three models. In all three models, the Wald test shows that was significantly different from zero, indicating that the receipt of informal care is an endogenous variable (). Thus, coefficients should be estimated in a bivariate probit model.
shows the results of regression analyses where an interaction term between the receipt of informal care and the time dummy was included in the bivariate probit models. The coefficient of the informal care variable was negative and statistically significant in all three models. This suggests that the receipt of informal care significantly reduced the probability of receiving formal social care before 2015. The time dummy was negative and statistically significant in the model focusing on formal personal care (i.e., formal care for ADLs), which indicates that the probability of receiving this type of formal care was significantly lower after 2015 than before 2015. The interaction term was positive and significant in the model focusing on formal care for ADLs. This indicates that the negative association between informal care and formal care for ADLs was significantly weaker after 2015 than before 2015. These results are highly robust when we confined our analyses to different time periods before and after 2015 (Table A4 in the appendix). The coefficients of control variables in changed very little in comparison to those in . Like , the results of the Wald test were significant in all three models, indicating the importance of accounting for an endogenous informal care variable in the bivariate probit models.
Table 3. Factors associated with receipt of formal social care (bivariate probit models with interaction term).
The bivariate probit models enabled us to calculate the predicted probability of receiving formal social care based on whether or not people received informal care, which is shown in . The average predicted probability of receiving formal care was 0.085 in older people who did not receive informal care and 0.054 in those who received informal care between 2011 and 2018. Such a difference is statistically significant (panel 1a). A similar pattern can be noted if we look at people in the HSE sample before and after 2015, respectively.
Figure 1. Probability of receiving formal social care according to whether or not receiving informal care.
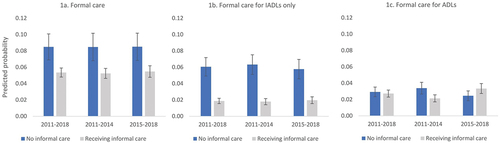
The average predicted probability of receiving formal care for IADLs was 0.061 in people who did not receive informal care, which was significantly higher than the probability of 0.019 in recipients of informal care. Such a pattern remains for people in the survey before and after 2015, respectively (panel 1b). The average probability of receiving formal care for ADLs was 0.029 in people who did not receive informal care, which is slightly higher than the probability of 0.027 in informal care recipients. The difference is not statistically significant. For people in the survey between 2011 and 2014, the probability of receiving formal care was 0.34 (95% CI: 0.027–0.041) among people not receiving informal care, which is significantly higher than the probability of 0.21 (95% CI: 0.017–0.026) among recipients of informal care. For people in the survey between 2015 and 2018, the average probability of receiving formal care for ADLs was higher in recipients of informal care than in people who did not receive it, but the difference is not statistically significant (panel 1c).
Discussion
Drawing on a large sample of 17,292 people from a nationally representative survey collected between 2011 and 2018, this study investigated the impact of informal social care on receiving formal social care in England. We built bivariate probit models to address the endogeneity issue in the analysis. We found an overall substitutive relationship between formal and informal care. All other things being equal, people receiving informal care are less likely to receive formal social care, which confirms our first hypothesis. We distinguished between formal personal and domestic care. When we investigated the receipt of formal social care according to the type of daily tasks, we found that the receipt of informal care has an especially strong substitution effect on formal domestic care.
Our second hypothesis was partially confirmed. We did not observe significant changes in the relationships between formal domestic care and informal care over time. However, the substitution between formal personal care and informal care was significantly weakened after 2015. Such a finding can be explained by the fact that people receiving formal personal care and those receiving only domestic care relied on different sources to pay for their care. The eligibility criteria for state-funded care in England are closely linked to the levels of care needs of older people, with the provision of government support prioritized for those with greater care needs. This remains the case after the National Minimum Eligibility Criteria were introduced in the Care Act 2014 (Fernandez et al., Citation2015). Older people receiving personal care have a higher level of care needs than those receiving only domestic care and thus are more likely to pass the thresholds for government support in the need assessments. The introduction of the National Minimum Eligibility Criteria means that the former group will receive state-funded formal social care irrespective of the receipt of informal care. As a result, the substitutive relationships after 2015 were not as strong as before 2015. In contrast, many people who received only domestic care were self-funders. The reforms in the Care Act 2014 do not directly affect their purchase of formal social care from the market, so the substitution between formal and informal care remains salient.
The substitutive relationships between informal and formal social care found in our study are broadly consistent with those reported in the international literature (Van Houtven & Norton, Citation2004; Bolin et al., Citation2008; Bonsang, Citation2009, Sun et al., Citation2019; Urwin et al., Citation2019). Like previous studies, ours confirmed the importance of correcting for endogeneity in the regression modeling to avoid biased estimates. The previous studies show that the substitution effects of informal care on formal care tend to be stronger in older people with a lower level of care needs or requiring low-skill care (Bonsang, Citation2009) and in countries with a strong expectation of receiving care from family (Bolin et al., Citation2008), pointing to the heterogeneity of the substitutive relationships in sub-populations. We have observed such heterogeneous effects in our data. Indeed, the low-skill nature of performing domestic tasks may contribute to the strong substitutive relationships between formal domestic care and informal care. Furthermore, our study shows that policy change is another reason for heterogeneity. In the context of England, the attenuation of the substitution effects took place after a system-wide reform to sever the link between formal and informal care on the grounds of care equity and distributive fairness.
The strong association between a wide range of control variables and the receipt of formal social care indicates great variations in the propensity to receive formal care in the older population. All other things being equal, people with a higher level of education and living in owned housing are more likely to receive formal care. This is especially the case when we focus on people receiving domestic care who are often self-funders. In the absence of financial support from the government, the distribution of care is strongly in favor of older people with a higher socioeconomic status, confirming the existing findings in the English context (Hu et al., Citation2022a).
Long-term care services help older people compensate for declines in functional capabilities and meet their care needs (Hu et al., Citation2022b). Our analyses show that functional disabilities are not the only indicators of care needs. Despite their collinearity with functional capabilities, two other health-related factors including long-term illness and self-reported health are directly associated with formal care receipt. These results are important because they point to the risk of missing important predictors of care receipt in research that relies exclusively on functional capabilities as a measurement of care needs. In practice, this implies that comorbidities are important factors to be considered in the process of needs assessment.
Limitations and future research
Limitations of the study should be acknowledged. First, due to data limitations, we were not able to distinguish between state-funded care recipients and self-funders in the analysis. We had to base the interpretation of some research findings on the strong correlation between the sources of funding and the types of care (namely personal care vs. domestic care) shown in the literature. Second, we relied on the functional form to account for the endogeneity in our models. Characteristics of caregivers such as birth order or gender composition of children have been identified as valid instrumental variables to address the issue of endogeneity (Bolin et al., Citation2008; Bonsang, Citation2009; Sun et al., Citation2019; Urwin et al., Citation2019; Van Houtven & Norton, Citation2004). But such information was not collected in the HSE. In the absence of instrumental variables, our models can still be identified but they may be vulnerable to misspecifications. We have taken great care to address this limitation in the analyses. Following the guidance of well-established theoretical frameworks, we took advantage of the rich information in the HSE surveys to include a wide range of control variables in the models, which should help us reduce the risks of model misspecification. Third, long-term illness is a binary variable pooling diverse conditions such as visual, hearing, or mobility problems. Our results do not show their individual impacts on formal care receipt. Finally, our study assumes that the reforms introduced in the Care Act 2014 regarding the eligibility criteria have been effectively implemented by local authorities. Future qualitative research focusing on policy implementation will provide further insight into the relationships between formal and informal care.
Conclusion
The substitution between formal and informal care highlights the importance of government support to older people with care needs. Formal social care is valuable because the supply of informal care alone may not keep up with care demand in the current context of population aging. Since the announcement of the Care Act 2014 in England, the impacts of informal care on receiving personal care have been weakened. This seems to be a sign of increasing commitments by the state to sharing caregiving responsibilities with informal caregivers, which should help protect the well-being and health of informal caregivers in the long run. However, access to domestic or practical care still depends on the availability of informal caregivers and the affordability of services on the private market. Older people without informal caregivers and with lower financial means may have limited access to help, which can lead to unmet needs or care poverty. Looking ahead, the government may consider stepping up support for people with domestic care needs and promoting equal access to domestic care.
Key points
The overall relationship between formal and informal social care in England is substitutive.
Formal social care for older people has been increasingly “carer-blind” since the implementation of the Care Act 2014.
Substitution between formal personal care and informal care was significantly weakened after 2015.
Supplemental Material
Download MS Word (39.2 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/08959420.2023.2226308
Additional information
Funding
References
- Andersen, R., & Newman, J. F. (2005). Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly, 83(4), 1–28. https://doi.org/10.1111/j.1468-0009.2005.00428.x
- Bolin, K., Lindgren, B., & Lundborg, P. (2008). Informal and formal care among single-living elderly in Europe. Health Economics, 17(3), 393–409. https://doi.org/10.1002/hec.1275
- Bonsang, E. (2009). Does informal care from children to their elder parent substitute for formal care in Europe. Journal of Health Economics, 28(1), 143–154. https://doi.org/10.1016/j.jhealeco.2008.09.002
- Brimblecombe, N., Fernandez, J.-L., Knapp, M., Rehill, A., & Wittenberg, R. (2018). Unpaid care in England: Future patterns and potential support strategies. Personal Social Services Research Unit. https://eprints.lse.ac.uk/90215/1/Brimblecombe_Fernandez_Knapp%20et%20al._Unpaid%20care%20in%20England_Author%20_%202018.pdf
- Carrieri, V., DiNovi, C., & Orso, C. E. (2017). Home sweet home? Public financing and inequalities in the use of home care services in Europe. Fiscal Studies, 38(3), 445–468. https://doi.org/10.1111/j.1475-5890.2017.12138
- Comas-Herrera, A., Wittenberg, R., & Pickard, L. (2010). The long road to universalism? Recent developments in the financing of long-term care in England. Social Policy & Administration, 44(4), 375–391. https://doi.org/10.1111/j.1467-9515.2010.00719.x
- Department of Health and Social Care. (2022). Care and support statutory guidance. https://www.gov.uk/government/publications/care-act-statutory-guidance/care-and-support-statutory-guidance
- Elgazzar, H. (2009). Income and the use of health care: An empirical study of Egypt and Lebanon. Health Economics, Policy, and Law, 4(4), 445–478. https://doi.org/10.1017/S1744133109004939
- Fernandez, J.-L., Snell, T., Forder, J., & Wittenberg, R. (2013). Implications of setting eligibility criteria for adult social care services in England at the moderate needs level. Personal Social Services Research Unit. https://www.pssru.ac.uk/pub/dp2851.pdf
- Fernandez, J.-L., Snell, T., & Marczak, J. (2015). An assessment of the impact of the care act 2014 eligibility regulations. Personal Social Services Research Unit. https://eprints.lse.ac.uk/64773/1/__lse.ac.uk_storage_LIBRARY_Secondary_libfile_shared_repository_Content_PSSRU_Discussion%20Papers_DP2905.pdf
- Forder, J. (2007). Self-funded social care for older people: An analysis of eligibility, variations and future projections. PSSRU.
- Greene, W. H. (2011). Econometric analysis (7th ed ed.). Pearson Education Limited.
- Hanaoka, C., & Norton, E. C. (2008). Informal and formal care for elderly persons: How adult children’s characteristics affect the use of formal care in Japan. Social Science & Medicine, 67(6), 1002–1008. https://doi.org/10.1016/j.socscimed.2008.05.006
- Hancock, R., Hu, B., Wittenberg, R., King, D., & Morciano, M. (2022). Reforming the funding of adult social care: Costs and impacts of the government’s proposal. Care Policy and Evaluation Centre. https://www.lse.ac.uk/cpec/assets/documents/ASCRU-CPEC-WP11-Hancock.pdf
- HM Government. (2021). Build Back better. our plan for health and social care.
- Hu, B., Cartagena-Farias, J., & Brimblecombe, N. (2022b). Functional disability and utilisation of long-term care in the older population in England: a dual trajectory analysis. European Journal of Ageing, 19(4), 1363–1373. https://doi.org/10.1007/s10433-022-00723-0
- Hu, B., Hancock, R., & Wittenberg, R. (2020). Projections of adult social care demand and expenditure 2018 to 2038. Care Policy and Evaluation Centre. https://www.lse.ac.uk/cpec/assets/documents/cpec-working-paper-7.pdf
- Hu, B., Read, S., Wittenberg, R., Brimblecombe, N., Rodrigues, R., Banerjee, S., & Fernandez, J. L. (2022a). Socioeconomic inequality of long-term care for older people with and without dementia in England. Ageing & Society, 1–21. https://doi.org/10.1017/S0144686X22000885
- Institute of Public Care. (2012). Where the heart is: A review of the older people’s home care market in England. Oxford Brookes University. https://ipc.brookes.ac.uk/files/publications/Where_the_heart_is_IPC_MAC_Review_of_Home_Care.pdf
- Kim, H. B., & Lim, W. (2015). Long-term care insurance, informal care, and medical expenditures. Journal of Public Economics, 125, 128–142. https://doi.org/10.1016/j.jpubeco.2014.12.004
- Kröger, T. (2022). Care poverty: When older people’s needs remain unmet. Palgrave Macmillan Cham. https://doi.org/10.1007/978-3-030-97243-1
- Lemmon, E. (2020). Utilisation of personal care services in Scotland: The influence of unpaid carers. The Journal of Long-Term Care, 2020(2020), 54–69. https://doi.org/10.31389/jltc.23
- Lo Sasso, A. T., & Johnson, R. W. (2002). Does informal care from adult children reduce nursing home admissions for the elderly? INQUIRY: The Journal of Health Care Organization, Provision, & Financing, 39(3), 279–297. https://doi.org/10.5034/inquiryjrnl_39.3.279
- Monfardini, C., & Radice, R. (2008). Testing exogeneity in the bivariate probit model: A Monte Carlo study. Oxford Bulletin of Economics and Statistics, 70(2), 271–282. https://doi.org/10.1111/j.1468-0084.2007.00486.x
- Moussa, M. M. (2019). The relationship between elder care-giving and labour force participation in the context of policies addressing population ageing: A review of empirical studies published between 2006 and 2016. Ageing and Society, 39(6), 1281–1310. https://doi.org/10.1017/S0144686X18000053
- NHS Digital. (2022). Health Survey for England: Health, social care, and lifestyles. https://digital.nhs.uk/data-and-information/areas-of-interest/public-health/health-survey-for-england---health-social-care-and-lifestyles
- Saloniki, E., Nizalova, O., Malisauskaite, G., & Forder, J. (2019). The impact of formal care on informal care for people over 75 in England. Personal Social Services Research Unit.
- Skills for Care. (2022). The state of the adult social care sector and workforce in England.
- Social Care Institute for Excellence. (2015). Eligibility determination for the Care Act 2014. https://www.scie.org.uk/care-act-2014/assessment-and-eligibility/determination-eligibility
- Stabile, M., Laporte, A., & Coyte, P. C. (2006). Household responses to public home care programs. Journal of Health Economics, 25(4), 674–701. https://doi.org/10.1016/j.jhealeco.2005.03.009
- Sun, Z., Guerriere, D. N., de Oliveira, C., & Coyte, P. C. (2019). Does informal care impact utilisation of home‐based formal care services among end‐of‐life patients? A decade of evidence from Ontario, Canada. Health & Social Care in the Community, 27(2), 437–448. https://doi.org/10.1111/hsc.12664
- Urwin, S., Lau, Y. S., & Mason, T. (2019). Investigating the relationship between formal and informal care: An application using panel data for people living together. Health Economics, 28(8), 984–997. https://doi.org/10.1002/hec.3887
- Van Houtven, C., & Norton, E. (2004). Informal care and health care use of older adults. Journal of Health Economics, 23(6). https://doi.org/10.1016/j.jhealeco.2004.04.008
- Wilde, J. (2000). Identification of multiple equation probit models with endogenous dummy regressors. Economics Letters, 69(3), 309–312. https://doi.org/10.1016/S0165-1765(00)00320-7
- Zhang, W., Sun, H., & L’Heureux, J. (2021). Substitutes or complements between informal and formal home care in the Canadian longitudinal study on aging: functional impairment as an effect modifier. Health Policy, 125(9), 1267–1275. https://doi.org/10.1016/j.healthpol.2021.07.004
- Zigante, V., Fernandez, J.-L., & Mazzotta, F. (2021). Changes in the balance between formal and informal care supply in England between 2001 and 2011: Evidence from census data. Health Economics, Policy, and Law, 16(2), 232–249. https://doi.org/10.1017/S1744133120000146
