Abstract
Acute and subacute stent thromboses are rare but life-threatening complications of primary coronary intervention and stenting. We present a case of a patient with COVID-19 infection who presented with pneumonia, acute respiratory failure, and non–ST elevation myocardial infarction. Reperfusion was achieved with coronary angioplasty and drug-eluting stent placement, and the patient was started on aspirin and clopidogrel. However, 72 hours later, the patient experienced an episode of subacute stent thrombosis. This raises concerns about a possible association between stent thrombosis and increased thrombogenicity and platelet aggregability triggered by COVID-19 infection.
Acute and subacute stent thrombosis is a rare but serious complication of primary coronary intervention (PCI) with stenting and is associated with an extremely poor outcome if left untreated.Citation1,Citation2 COVID-19 infection is associated with a hypercoagulable state with a high incidence of thrombotic complications.Citation3,Citation4 We present a case of subacute stent thrombosis in a patient with COVID-19 pneumonia.
CASE PRESENTATION
A 64-year-old black man with chronic hepatitis C, hypertension, and treated pulmonary tuberculosis presented with dyspnea and cough that had worsened over 2 weeks. His temperature was 97.7°F; heart rate, 89 beats per minute; blood pressure, 147/97 mm Hg; respiratory rate, 23 breaths per minute; and oxygen saturation 83%. A SARS-CoV2 (COVID-19) reverse transcription polymerase chain reaction assay was positive. Chest radiography showed bilateral lung infiltrates, and the patient was admitted to the intensive care unit for acute respiratory distress syndrome due to SARS-CoV2 pneumonia. The admission electrocardiogram showed normal sinus rhythm with T wave inversion in anteroseptal leads (). Troponin I on admission was 1.39 ng/mL (normal <0.03). The patient denied any current or prior anginal symptoms. He was diagnosed with non–ST elevation myocardial infarction.
Figure 1. Electrocardiograms (a) on admission with T wave inversions in anteroseptal leads, (b) on day 2 showing polymorphic ventricular tachycardia during cardiac arrest, and (c) 72 hours after index PCI with ST segment depressions in lateral leads.
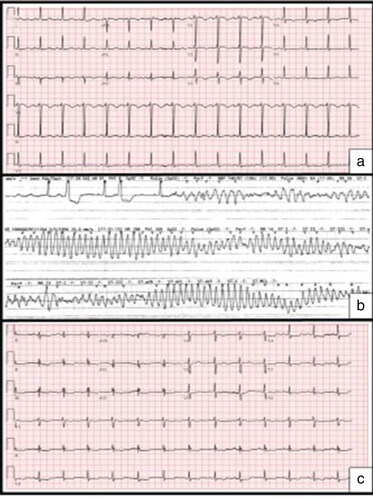
Given the hemodynamic and electrical stability and the absence of angina, and to minimize the staff’s risk of exposure to COVID-19, it was decided to manage the patient conservatively. He was started on aspirin, heparin infusion, broad-spectrum antibiotics, and remdesivir. A transthoracic echocardiogram showed a left ventricular ejection fraction of 45% to 50% with reduced peak global longitudinal strain across the inferolateral and lateral segments. On day 2, the patient had progressive respiratory failure and later he sustained cardiac arrest due to polymorphic ventricular tachycardia () and was successfully resuscitated and placed on mechanical ventilation. His troponin level increased to 11.61 ng/mL.
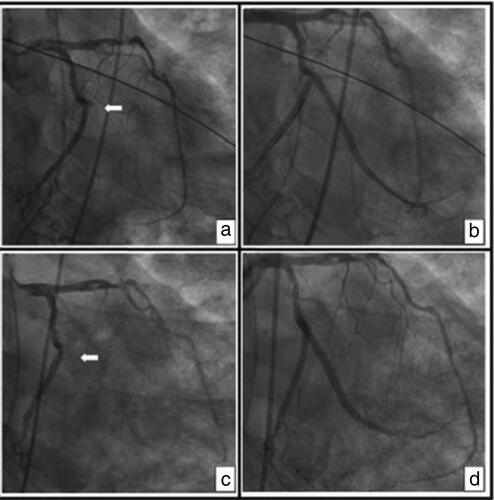
Urgent coronary angiography showed 100% thrombotic occlusion of the second obtuse marginal artery, a severe lesion in the mid left anterior descending artery, and distal occlusion of a nondominant right coronary artery (). He had successful PCI with a 3.0 × 38 mm Resolute Onyx drug-eluting stent to the second obtuse marginal artery (). He was loaded with 600 mg of clopidogrel in the catheterization lab and started on 75 mg of clopidogrel daily. Heparin infusion was restarted after PCI per intensive care unit protocol for the COVID-associated hypercoagulability state. Three days after PCI, he had worsening hemodynamics and developed ST-segment depressions in lateral leads () with a rising troponin level after it had trended down after PCI (34 ng/mL from 7 ng/mL after PCI). Urgent coronary angiography revealed complete occlusion of the second obtuse marginal artery from stent thrombosis (). Balloon angioplasty reestablished Thrombolysis in Myocardial Infarction (TIMI)–3 flow; however, a new 3.0 × 34 mm Resolute Onyx stent was placed because of significant residual filling defect ().
Figure 2. Coronary angiograms, right anterior oblique caudal views: (a) index angiogram showing 100% thrombotic occlusion of the second obtuse marginal artery (OM2) (arrow); (b) after PCI of OM2 with a drug-eluting stent with TIMI 3 flow; (c) 72 hours after PCI showing complete occlusion of OM2 from stent thrombosis (arrow); and (d) after repeat PCI of OM2 with a drug-eluting stent showing TIMI 3 flow.
The patient was switched to ticagrelor, a more potent agent than clopidogrel, and started on eptifibatide infusion. A P2Y12 reactivity unit VerifyNow test performed >48 hours after stopping eptifibatide infusion showed a value of 69 (levels <194 indicate high platelet inhibition with P2Y12 inhibitor). Heparin PF4 antibody by Latex-enhanced immunoassay was tested, as there was a 50% drop in platelets 4 days after heparin initiation, and was negative. The patient had elevated inflammatory markers, D-dimer, ferritin, and C-reactive protein. Prothrombin and partial thromboplastin time were normal. He was placed on dexamethasone and tocilizumab to treat the systemic inflammation. Ten days after the second PCI, the patient was off mechanical ventilation with normal hemodynamics and no recurrence of cardiac arrhythmia, ischemic ST changes, or release of troponin.
DISCUSSION
Coronary intervention technical failure, decreased platelet inhibition, and hypercoagulable states are the main risk factors for acute and subacute stent thrombosis. Although no intravascular imaging was done after stenting, the angiographic result in orthogonal views was satisfactory and not indicative of any technical failure of the procedure. Delayed intestinal absorption and decreased bioavailability of clopidogrel may happen in sedated patients; however, the low P2Y12 reactivity unit VerifyNow test value makes this possibility and clopidogrel resistance unlikely etiologies of stent thrombosis in this case. In addition, the possible interaction of P2Y12 inhibitors with antiviral treatment of COVID-19 was considered. The patient was treated with remdesivir, which has no known interaction with these medications. Therefore, COVID-19–triggered hypercoagulability was believed to be the more likely cause of subacute stent thrombosis in this patient.
COVID-19 may predispose to both venous and arterial thromboembolic disease due to excessive inflammation, hypoxia, and diffuse intravascular coagulation.Citation3–5 Although these patients are at risk of acute coronary events from de novo coronary thrombosis, COVID-19 may increase the incidence of stent thrombosis, as shown in this and other reports.Citation6–8 Most patients with severe COVID-19 have laboratory evidence of severe inflammatory response, similar to cytokine release syndrome, with persistent fevers, elevated inflammatory markers (e.g., D-dimer, ferritin), and elevated proinflammatory cytokines.Citation9,Citation10 This severe inflammatory response with massive release of tissue factors and interleukin-6 may promote the coagulation cascade and platelet activation. Additionally, there is evidence of direct invasion of endothelial cells by the virus, potentially leading to cell injury and promotion of a procoagulable state.Citation10
In conclusion, COVID-19 infection triggers a hypercoagulable state and raises concerns about a possible increased risk of acute coronary syndromes and stent thrombosis. New generation P2Y12 inhibitors, glycoprotein IIb/IIIa inhibitors, and drug interactions should be considered in patients with COVID-19 treated with PCI and stenting to reduce the risk of stent thrombosis.
- Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126–2130. doi:https://doi.org/10.1001/jama.293.17.2126.
- Ong AT, Hoye A, Aoki J, et al. Thirty-day incidence and six-month clinical outcome of thrombotic stent occlusion after bare-metal, sirolimus, or paclitaxel stent implantation. J Am Coll Cardiol. 2005;45(6):947–953. doi:https://doi.org/10.1016/j.jacc.2004.09.079.
- Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi:https://doi.org/10.1016/j.thromres.2020.04.013.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:https://doi.org/10.1016/S0140-6736(20)30566-3.
- Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi:https://doi.org/10.1136/bmj.m1091.
- Lacour T, Semaan C, Genet T, Ivanes F. Insights for increased risk of failed fibrinolytic therapy and stent thrombosis associated with COVID-19 in ST-segment elevation myocardial infarction patients. Catheter Cardiovasc Interv. 2020. doi:https://doi.org/10.1002/ccd.28948.
- Hinterseer M, Zens M, Wimmer RJ, et al. Acute myocardial infarction due to coronary stent thrombosis in a symptomatic COVID-19 patient [published online ahead of print, 2020 May 19]. Clin Res Cardiol. 2020;1–5. doi:https://doi.org/10.1007/s00392-020-01663-4.
- Prieto-Lobato A, Ramos-Martínez R, Vallejo-Calcerrada N, Corbí-Pascual M, Córdoba-Soriano JG. A case series of stent thrombosis during the COVID-19 pandemic. JACC Case Rep. 2020; 2(9):1291–1296. doi:https://doi.org/10.1016/j.jaccas.2020.05.024.
- Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738–1742. doi:https://doi.org/10.1111/jth.14850.
- Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18(7):1747–1751. doi:https://doi.org/10.1111/jth.14854.
