Abstract
The COVID-19 pandemic has presented new challenges to microsurgeons. The virus is highly transmissible, with increased risk during operations that involve the aerodigestive tract. It is important to be able to identify high-risk operations and scenarios to guide management decisions and selection of personal protective equipment. Preoperative testing is a key element in identifying high-risk scenarios, and preoperative testing protocols are essential to maintaining safety in the COVID-19 era. Because COVID-19 can be transmitted via the conjunctiva, adaptations to loupes and microscopes are necessary to safely perform microsurgery in high-risk scenarios. We outline a potential risk stratification algorithm, as well as precautions for each scenario. Potential areas for innovation are also discussed.
Keywords:
Health care systems worldwide have been forced to adapt to coronavirus disease 2019 (COVID-19). Presentations range from asymptomatic to acute respiratory failure, multisystem organ failure, hypercoagulable states, and death.Citation1 Despite global efforts, more than 62 million cases were reported globally as of November 3, 2020 with a case fatality rate of 2.3%.Citation2 However, traumatic and oncologic reconstructive needs persist. We discuss the known risks of COVID-19 to microsurgeons, proposed alterations in decision making, and interventions to mitigate risk.
TRANSMISSION AND SYMPTOMS
Transmission of COVID-19 occurs through droplets and contact. Droplets spread 1 to 2 meters and infect mucous membranes.Citation3,Citation4 Certain operations and techniques aerosolize the virus, potentiating transmission at greater distances.Citation5 The incubation period ranges from 1 to 14 days, with a median of 3 to 7 days, and patients are infectious during this time.Citation3,Citation4,Citation6 Viral shedding is known to have occurred from 4 to 37 days.Citation7,Citation8 The most common symptoms are fever, cough, ageusia, anosmia, expectoration, myalgia or fatigue, and shortness of breath.Citation4,Citation9,Citation10 However, 8.3% to 58.3% of patients remain asymptomatic based on two studies in Japan looking at evacuees from Wuhan and patients from the Diamond Princess cruise ship.Citation11,Citation12
Aerosolization is a significant risk to microsurgeons. Viral particles are most prevalent in the mucosa of the head and neck and become aerosolized via intubation, endoscopy, irrigation, cautery, and with reciprocating instrument use.Citation13 Supraphysiologic viral burden has been observed in aerosol clouds, when 14 operating room (OR) staff contracted the illness after endonasal pituitary resection on a presymptomatic patient.Citation14 Viral cell entry is mediated by angiotensin-converting enzyme 2 (ACE2) receptors present on the naso-oral mucosa and conjunctiva.Citation15 Thus, sealed eye protection and respirators are necessary in high-risk scenarios. This becomes problematic when performing microsurgery, as using a microscope or high-powered loupes with sealed eye protection has not been previously described. Preoperative testing and awareness of high-risk scenarios is important for guiding appropriate personal protective equipment (PPE) selection.
TESTING
We perform preoperative testing on all surgical patients. Reverse transcriptase polymerase chain reaction (RT-PCR) is used most commonly; however, false-negatives are common, with sensitivities of 70% to 80%.Citation16 Serological testing is frequently performed in conjunction with RT-PCR. In one study, 50% of patients underwent seroconversion at 7 days, and 100% at 14 days, making the test a good indicator of infection late in the disease.Citation17 We perform concurrent RT-PCR and serological testing (IgG and IgM) 48 to 72 hours prior to surgery. The patients are asked to self-isolate during the testing process. Prior to the advent of serology for COVID-19, we performed RT-PCR testing 3 to 5 days prior to surgery and again 24 to 72 hours prior. This strategy may be useful for institutions where RT-PCR is readily available but serology is not. We feel that a single RT-PCR 24 to 48 hours prior to surgery is sufficient in patients with negative screening when they are undergoing procedures that are standard risk.
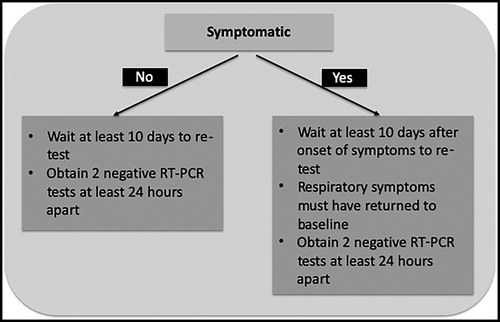
It is unknown when it is safe to perform surgery on someone who has tested positive for COVID-19. Our policies are shown in and have resulted in low transmission rates. Patients who remain asymptomatic must wait at least 10 days to be retested and must have two negative RT-PCR tests 24 hours apart prior to undergoing surgery. Symptomatic patients must wait 10 days after becoming symptomatic to be retested, and respiratory symptoms must return to baseline. It must be acknowledged that the duration of viral shedding is currently unknown and that preoperative guidelines are rapidly shifting.
PERSONAL PROTECTIVE EQUIPMENT
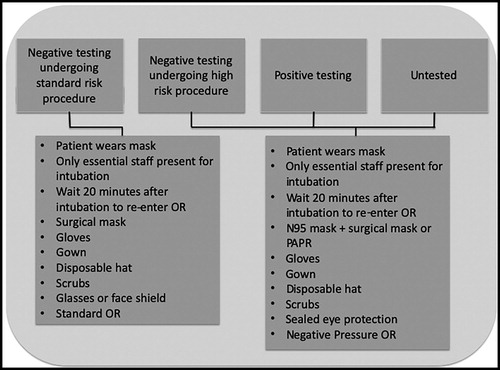
PPE protocols should address four scenarios: patients with negative testing undergoing standard-risk procedures, patients with negative testing undergoing high-risk procedures, patients with positive testing, and patients who are untested. However, the senior author has simplified PPE usage into two groups: patients with negative testing undergoing standard-risk procedures and all other operative situations. Specific recommendations are shown in .
We recommend that patients wear masks whenever possible. Only essential staff should be present during intubation. Additionally, N95 masks or a powered air purifying respirator should be worn by all staff present. The AO Foundation recommends that nonessential staff wait 20 minutes after intubation to enter the room, as standard OR air filtration systems remove 99.9% of airborne pathogens during this interval.Citation18
For patients with negative testing undergoing standard-risk operations, after intubation, operations proceed as they did prior to COVID-19. A standard OR may be used, and operating staff wear scrubs, a disposable cap, nonporous gown, standard surgical mask, sterile gloves, and glasses or a face shield. An N95 mask may be worn if preferred. Our institution has adopted an ultraviolet light N95 sterilization and conservation protocol. Masks are picked up every morning and returned at the end of the day. Sterilization requires 5 days, so five masks are rotated. They are discarded after five uses.
HIGH-RISK AND STANDARD-RISK RECONSTRUCTION
For patients undergoing high-risk reconstructions, those with positive testing, and those who are untested requiring urgent operations, operations are performed in a negative pressure or high-efficiency particulate air–filtered OR. A donning and doffing area is designated outside of the OR. An N95 mask or powered air purifying respirator is worn. We recommend wearing a standard surgical mask over an N95 mask to prevent gross soilage and allow for sterilization protocols. AO guidelines recommend a face shield or sealed eye protection; however, the senior author prefers sealed eye protection given the risk of aerosolization and transconjunctival transmission for high-risk surgeries.Citation18
High-risk scenarios include any procedure that violates the mucosa that harbors the virus in the highest titers. This includes the head and neck, as well as the bronchioles. However, viral particles have been found in stool samples, and ACE2 receptors are present on colonic mucosa. Thus, caution must be taken during perineal reconstruction as well.Citation19 Many reconstructions are elective. The risk to the patient of delaying reconstruction must be weighed against the risk to the surgical team of proceeding with high-risk reconstruction. The surgical and anesthetic risks that COVID-19 confers to patients who may have tested falsely negative is also currently unknown and should be discussed with the patient preoperatively.
Tumor extirpation and reconstruction are frequently performed in a single stage. However, packing head and neck resection defects and performing the reconstruction on the following day has been performed safely at our institution, as well as anecdotally at other institutions. We recommend this strategy in high-risk reconstructions for defects that would tolerate a staged approach, as this separates the reconstructive team from the extirpation, which tends to be the aerosolizing and higher-risk portion of the operation. Staging reconstruction from extirpation in this manner must be weighed against the potentially increased use of resources and intensive care unit beds. Use of anastomotic couplers for both venous and arterial anastomoses, if viable, may also expedite the procedure.Citation20 Additionally, the most experienced members of the operative team should perform microsurgery to decrease exposure time.
Standard-risk reconstructions are all those that do not meet high-risk criteria in patients with appropriate negative testing. Some authors have elected for conservative treatment in COVID-19–positive or untested patients where free tissue transfer would have been performed otherwise.Citation21 Many surgeons advocate for early coverage of lower-extremity wounds. However, rapid testing to achieve a reconstruction within 72 hours, as advocated by some authors, may not be achievable at all institutions.Citation22 We believe that there is sufficient evidence on the safety of delaying reconstruction in these defects until adequate testing can be performed or resolution of disease confirmed.Citation23 We believe that this should be achievable within 7 to 10 days in patients without COVID-19. Microsurgery may then proceed without additional intervention.
REVASCULARIZATION
Revascularization may necessitate operating on a patient who is COVID-19 positive or whose disease status has not yet been confirmed. A patient with active respiratory symptoms needing revascularization was recently transferred to our institution, and RT-PCR was pending when the decision was made to proceed to the OR. This raised multiple questions that microsurgeons may need to consider. We consider the potential deficits that a patient may have if not revascularized, as well as future reconstructive options prior to operating on a positive or untested patient. Devitalized fingers are common at our institution. We would proceed with multidigit, thumb, or major limb revascularization in a COVID-19–positive patient who is otherwise a candidate. Single digit amputation would be considered on a case-by-case basis.
Revascularizing the ears, nose, and scalp may be considered in appropriate COVID-19–positive or untested patients. However, this choice may vary by surgeon and may be impacted by their confidence in reconstructing a life-like replacement. Due to the significant challenges in producing a reconstructed ear that would equally restore form compared to the replanted native ear, we would consider revascularization in a suitable candidate. Revascularization of the nose or nasal segments has also been described and may be appropriate.Citation24 Banking auricular or nasal avulsion injuries may be an option, with revascularization deferred until proper testing or resolution of disease is confirmed.
For scalp reconstruction, we separate these injuries into avulsions of less than or greater than 50% of the hair-bearing scalp. Defects <50% can be reconstructed in a delayed fashion via tissue expansion with acceptable cosmetic results. In this case, reconstruction may be delayed. If >50% of the hair-bearing scalp has been injured, tissue expansion does not provide a similar aesthetic result, and we would consider revascularization in a COVID-19–positive or untested patient who strongly desired an attempt at hair-bearing scalp restoration.
Microsurgeons who are at high risk for severe manifestations of COVID-19 should seek to mitigate this risk. Surgeons who are immunocompromised, have multiple pertinent comorbid conditions, or who are >65 years of age may need to find alternatives to revascularization. One option is to identify a colleague of standard risk who would be willing to perform revascularization, should the need arise.
Vasculitis and COVID-19–associated coagulopathy are common manifestations of the disease and vary considerably in presentation and severity. Capillaries, arterioles, arteries, venules, and veins can be affected, ranging from chilblains to large vessel thrombosis and pulmonary embolism or stroke.Citation25 This is of particular concern in microsurgery, as vessel thrombosis can lead to partial or complete flap loss. Thromboembolism prophylaxis has not been sufficient to prevent high rates of thrombotic complications in patients admitted to the intensive care unit in the past (31% and 49% in two studies).Citation26,Citation27 Multiple therapies are under investigation, including activated protein C, antithrombin, immunoglobulins, steroids, and agents targeting angiopoietin 2 or vascular endothelial growth factor.Citation28,Citation29 However, we lack sufficient evidence to recommend any of these agents at this time.
INNOVATIONS in MICROSURGERY
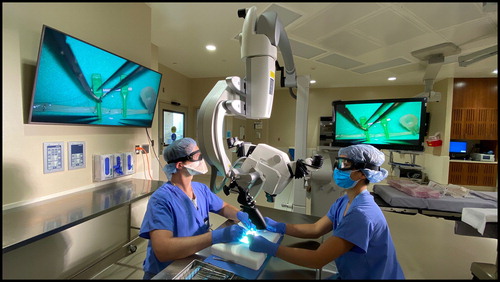
Inherent in the plastic surgeon is the ability to innovate in the face of challenges. In order to safely operate in the setting of high-risk reconstruction, adaptations to the standard microsurgery procedure may be considered. Use of sealed eye protection with the operating microscope has been feasible in our hands () with use of anti-fog solution to improve visibility. As closed eye protection can fog despite anti-fog, this limits the time available for microsurgery. This means that residents may perform less microsurgery, which ultimately may have an impact on resident education. If operating with a microscope that conveys high-definition video, one may consider use of the monitor to perform microsurgery in lieu of the eyepieces (). Before the COVID-19 pandemic, transoral robotic surgery was gaining widespread use among head and neck oncologic and reconstructive surgeons,Citation30 with outcomes comparable to those of nonrobotic anastomoses with use of a standard operating microscope.Citation31 This would allow spatial segregation of the operating surgeon from the high-risk field.
Figure 3. Successful microsurgery on a nerve tube utilizing a standard operating microscope, sealed goggles, and anti-fog solution.
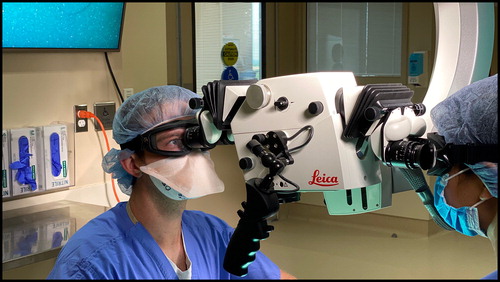
Figure 4. Microsurgery on a nerve tube utilizing high definition monitors, sealed goggles, and anti-fog solution in lieu of standard eye pieces.
Future innovations may include production of custom goggle loupes, at adequate magnification to perform microsurgery. The loupes may be built into the goggles or designed to flip down. Adjustable magnification lenses may be of use in this context, with lower magnification for vessel/nerve dissection and higher magnification for anastomoses/coaptation. This may present an opportunity for the microsurgeon to collaborate with the loupe industry in order to manufacture sealed eye protection loupes. Google Glass has gained popularity with plastic surgeons for a multitude of applications,Citation32 and future technological developments may allow for use in projected goggled microsurgery.
SUMMARY
The COVID-19 pandemic has challenged health care systems globally and affected both patients and health care providers alike. SARS-CoV-2 is highly transmissible, and the true proportion of asymptomatic carriers has not yet been elucidated. Plastic surgeons may be uniquely vulnerable, particularly microsurgeons operating on the head and neck region, as well as in emergent settings. Accurate and available testing is key to risk stratification and operating in a safe manner. High-risk scenarios, including COVID-19–positive cases, operating in high-risk regions, or operating on untested patients due to the emergent nature of their pathology warrant full precautions. Microsurgical reconstruction can be efficiently performed with adaptations to optimize safety for both the patient and surgical team. It is imperative to point out that all of the precautions and recommendations that we propose are influenced by the availability, sensitivity, and specificity of available testing. Given the rapid innovations in the COVID-19 landscape, changes to testing algorithms and safety precautions are likely. However, the principles outlined in this article are likely to remain applicable and may be useful when considering operating in the setting of other highly communicable diseases.
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi:10.15585/mmwr.mm6912e2.
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map. https://coronavirus.jhu.edu/map.html. Accessed November 30, 2020.
- Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281–286. doi:10.1007/s12098-020-03263-6.
- Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi:10.1136/bmj.m606.
- Thamboo A, Lea J, Sommer DD, et al. Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology - head and neck surgery during the COVID-19 pandemic. J Otolaryngol Head Neck Surg. 2020;49(1):28. doi:10.1186/s40463-020-00425-6.
- Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25(5). doi:10.2807/1560-7917.ES.2020.25.5.2000062.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3.
- Qian G-Q, Chen X-Q, Lv D-F, et al. Duration of SARS-CoV-2 viral shedding during COVID-19 infection. Infect Dis (Lond). 2020;52(7):511–512. doi:10.1080/23744235.2020.1748705.
- Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi:10.1016/j.ijantimicag.2020.105924.
- Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032.
- Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10). doi:10.2807/1560-7917.ES.2020.25.10.2000180.
- Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–155. doi:10.1016/j.ijid.2020.03.020.
- Jewett DL, Heinsohn P, Bennett C, Rosen A, Neuilly C. Blood-containing aerosols generated by surgical techniques: a possible infectious hazard. Am Ind Hyg Assoc J. 1992;53(4):228–231. doi:10.1080/15298669291359564.
- Workman AD, Welling DB, Carter BS, et al. Endonasal instrumentation and aerosolization risk in the era of COVID-19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol. 2020;10(7):798–805. doi:10.1002/alr.22577.
- Li J-PO, Lam DSC, Chen Y, Ting DSW. Novel coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104(3):297–298. doi:10.1136/bjophthalmol-2020-315994.
- Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020; 296(2):E32–E40. doi:10.1148/radiol.2020200642.
- Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi:10.1038/s41586-020-2196-x.
- Grant M, Schramm A, Strong B, et al. AO CMF International Task Force Recommendations on Best Practices for Maxillofacial Procedures during COVID-19 pandemic. AO Foundation; 2020. https://aocmf3.aofoundation.org/-/media/project/aocmf/aocmf/files/covid-19/ao_cmf_covid-19_task_force_guidelines.pdf?la=en&hash=C2B89E1E6E9AB72EBF386C747D3BC74CF1009C1E. Accessed May 23, 2020.
- Zhang W, Du R-H, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–389. doi:10.1080/22221751.2020.1729071.
- Sando I, Plott J, McCracken B, et al. Simplifying arterial coupling in microsurgery—a preclinical assessment of an Everter device to aid with arterial anastomosis. J Reconstr Microsurg. 2018;34(06):420–427. doi:10.1055/s-0038-1626691.
- Ramella V, Papa G, Bottosso S, Cazzato V, Arnež ZM. Microsurgical reconstruction in the time of COVID-19. Microsurgery. 2020;40(6):723. doi:10.1002/micr.30604.
- Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78(3):285–292. doi:10.1097/00006534-198609000-00001.
- Karanas YL, Nigriny J, Chang J. The timing of microsurgical reconstruction in lower extremity trauma. Microsurgery. 2008;28(8):632–634. doi:10.1002/micr.20551.
- Akyurek M, Perry D. Microsurgical replantation of completely avulsed nasal segment. J Craniofac Surg. 2019;30(1):208–210. doi:10.1097/SCS.0000000000005017.
- Becker RC. COVID-19-associated vasculitis and vasculopathy. J Thromb Thrombolysis. 2020;50(3):499–511. doi:10.1007/s11239-020-02230-4.
- Klok FA, Kruip MJHA, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. doi:10.1016/j.thromres.2020.04.041.
- Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18(5):1023–1026. doi:10.1111/jth.14810.
- Teuwen L-A, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20(7):389–391. doi:10.1038/s41577-020-0343-0.
- Iba T, Connors JM, Levy JH. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm Res. 2020;69(12):1181–1189. doi:10.1007/s00011-020-01401-6.
- Chalmers R, Schlabe J, Yeung E, Kerawala C, Cascarini L, Paleri V. Robot-assisted reconstruction in head and neck surgical oncology: the evolving role of the reconstructive microsurgeon. ORL J Otorhinolaryngol Relat Spec. 2018;80(3–4):178–185. doi:10.1159/000492787.
- Lai C-S, Lu C-T, Liu S-A, Tsai Y-C, Chen Y-W, Chen I-C. Robot-assisted microvascular anastomosis in head and neck free flap reconstruction: preliminary experiences and results. Microsurgery. 2019;39(8):715–720. doi:10.1002/micr.30458.
- Davis CR, Rosenfield LK. Looking at plastic surgery through Google Glass: part 1. Systematic review of Google Glass evidence and the first plastic surgical procedures. Plast Reconstr Surg. 2015;135(3):918–928. doi:10.1097/PRS.0000000000001056.