ABSTRACT
Half of the patients who used CL daily did not wish to switch to spectacles even with ocular-allergic symptoms and findings. Therefore, continued CL use with suppressed ocular allergy can improve productivity and quality of life for CL users. This study described the clinical courses of CL users with ocular-allergic conjunctivitis who started ARCL trials on their eyes. Diagnoses of the seven understudied cases were AKC in 3, VKC in 2, SAC in 1, and CLPC in 1 case. All seven cases had myopia. Following the use of ARCL, six patients except for case 7 were satisfied, and objective findings were judged to be well-controlled. ARCL can be a useful tool for CL users with allergic conjunctivitis. However, ARCL should be introduced after allergic conjunctivitis is controlled or becomes asymptomatic. Furthermore, ARCL should be immediately discontinued if ocular-allergic symptoms flare after introducing ARCL.
Contact-lens(CL) users often bothered by their ocular allergy disease. Kumar et alCitation1 reported over 20% of CL users complained exacerbation of seasonal ocular allergy due to CL. When daily wear contact-lens CL users experience worsened allergic conjunctivitis; ophthalmologists commonly instruct patients to stop using CLs and change to spectacles. The reasons are anti-allergic eyedrops attaching to CL can accelerate allergic inflammation,Citation2,Citation3 and CL can damage the barrier function of ocular surfaces, leading to an exacerbation of allergic conjunctivitis.
However, only about half of the patients who use CL daily switch to spectacles after the onset of allergic symptoms.Citation3,Citation4 Especially in patients with intense myopia, spectacles are refused because of visual field distortion. Furthermore, the magnification and reduction of images depend on the distance between the lens and pupil, including the absolute value of the diopter for correction. Thus, treating ocular allergy using CLs is challenging to improve daily CL users’ productivity and quality of life.
Antihistamine-releasing contact lenses (ARCLs) are soft contact lenses (SCLs) containing ketotifen. Based on the use of ARCLs by daily CL users, Pall et al.,Citation5 for the first time, investigated the effects of ARCLs. A conjunctival allergen challenge (CAC; Ora, Inc., Andover, MA) model was employed to compare mean itch scores after wearing ARCL and regular SCL. They observed that the mean itch score was significantly lower in the ARCL group. This report suggested ARCLs as an effective tool for CL users with allergic conjunctivitis. However, the criteria used in selecting the study population excluded those with allergic conjunctivitis-related findings, such as corneal staining and ocular redness.Citation5 Thus, from the report by Pall et al., it remained unclear whether ARCL is effective for patients with ocular-allergic symptoms and findings.Citation5
Therefore, to ascertain the potential of ARCLs to achieve both improvements in ocular-allergic symptoms and continued use of the CL, we prescribed ARCL to patients with allergic conjunctivitis to investigate whether the condition could be controlled without eye drop treatments.
Materials and methods
Between July 2021 and December 2021, ARCL was introduced to seven patients at our hospital.
Inclusion criteria were as follows:
Patients should have previously been using CL for vision correction in their daily lives,
Patients should be diagnosed with ocular allergy disease, judged on the basis of physical findings by an ocular allergy specialist (AF),
Patients should be willing to continue the vision correction with CL during ocular allergy treatments.
Conditions for introducing ARCL were as follows:
1) Subjective symptoms and objective findings should have been suppressed, including discontinuing steroid eye drops or tacrolimus eye drops.
2) Keratoconjunctivitis findings should have a Score lower than 2 based on The Japan Ocular Allergy Society Grading by Miyazaki et al.Citation6
If both criteria were met, patients were considered well-controlled or controlled enough.
Patients with uncontrolled keratoconjunctivitis were instructed to adhere to the dosage of prescribed eye drops strictly. Following a strict treatment regimen, all patients reached the requirements for ARCL introduction within 2 months. Furthermore, the use of eye drops, not only steroids and tacrolimus but also anti-histamine eye drops, was prohibited once ARCL wear was initiated. However, the use of artificial tear solutions was allowed.
Results
A summary of the seven understudied cases is shown in . As shown, the diagnosis was AKC in 3, VKC in 2, SAC in 1, and CLPC in 1 case. All 7 cases had myopia and preferred to use CLs to avoid image distortion caused by the spectacles. Except for case seven, consciously satisfied symptoms and objective findings were observed in the six patients who had successfully worn ARCL for several months. However, case 7 complained of exacerbated ocular-allergic symptoms a few hours after starting to wear ARCLs. Therefore, the prescription was discontinued.
Table 1. Summary of 7 cases.
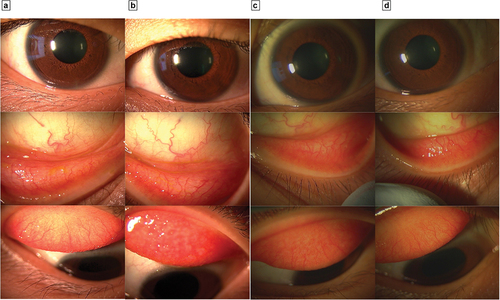
One representative case is following. A 19-year-old woman came to our clinic in September 2021 with a complaint of itching in both eyes during summer and winter. She had been using SCL for approximately 5 years before her visit, and her best-corrected visual acuity (BCVA) was R)20/16 L)20/13. Furthermore, her equivalent spherical power (ESP) was R)-5.0, L)-5.0, and conjunctival hyperemia, follicles, and punctate keratitis in both eyes and giant papillae with cobble stone appearance in her left eye were observed (). As a result of the antigen-specific IgE test in serum, it was found to be positive for Japanese ceder pollen, house dust mites and ragweed. Additionally, by Giemsa staining, many eosinophils were identified in her conjunctival scraping samples. Therefore, she was diagnosed with VKC, although it is necessary to mention CLPC for the differential diagnosis. Subsequently, her SCL use was discontinued, and tacrolimus/fluorometholone eye drops were introduced. Thus, allergic conjunctivitis findings, especially hyperemia in both eyes, improved. After discontinuing all ophthalmic treatments, the patient started wearing ARCLs in November 2021. Afterward, findings such as papillae, follicles, and hyperemia did not worsen and were maintained at the same conditions as when ARCLs were previously introduced. Since then, she has continued using ARCLs and has been doing well since February 2022.
Figure 1. a: Right eye at first visit in September 2021, b: Left eye at first visit in September 2021, c: Right eye at the second week after ARCL application, d: Left eye at the second week after ARCL application. a and b: Case four’s right and left eyes during the first admission, after which the patient was diagnosed with VKC. Subsequently, She was instructed to strictly adhere to the frequency and interval of topical tacrolimus steroid drops and started ARCL two months after. c and d: Right and left eyes two weeks after starting ARCL. Symptoms and objective findings became better without topical treatment and with CL refraction correction.
Discussion
Notably, this study diagnosed five of the seven understudied cases with AKC or VKC, a severe ocular allergy disease. Unfortunately, their conditions were poorly controlled when using tacrolimus and fluorometholone during their initial visit because they did not follow the instructed regimen. Therefore, CL wearing should be prohibited when the patient is still receiving such immunosuppressive eyedrop therapies. Consequently, we tried to control allergic conjunctivitis without administering eye drop treatments, such as tacrolimus and steroids. Subsequently, ARCLs were prescribed only when allergic conjunctivitis symptoms and findings were silenced as described in the inclusion criteria.
Six patients controlled their ocular-allergic symptoms without topical treatments after starting ARCL use. This finding proposes that ARCL can be used for CL users even with severe allergic conjunctivitis once the severity of conjunctivitis is controlled without eye drops.
The reason ARCL can control severe ocular allergy disease with ketofetin alone remains to be elucidated. However, it may be possible that ketotifen remains in the eye for a more extended period, allowing for prolonged drug exposure.Citation7 Additionally, it can also be possible that patient compliance is not needed because the patient does not have to administer the medication by himself/herself.Citation8,Citation9
Case 7 met the inclusion criteria for ARCL. However, the patient could not continue using ARCLs. The reason for this issue remains unclear. However, it is proposed that persistent inflammation in the conjunctiva resided even though slit-lamp microscopy did not detect it. Additionally, it should be noted that stopping immunosuppressive eye drop therapies in severe cases can exacerbate ocular-allergic symptoms.
Therefore, the key to the success of ARCL trials is to control ocular surface inflammation before ARCL induction. Another critical issue is the timing to discontinue ARCL when symptoms flare up. Hence, we recommend that ARCL be discontinued as immediately as possible, and the patient should be switched to receiving topical treatment. In some cases, multiple re-trials of ARCL introduction would be necessary to ensure the safety and effectiveness of ARCL.
In spite of this study’s findings, some limitations encountered include the following: The sample size was small and control participants (those with topical treatments or normal CLs) did not exist. Furthermore, the clinical value of ARCL for patients not used to CL is unknown because all patients had a history of long-term CL use.
It should be emphasized that the results of this study are not intended to actively recommend ARCL to patients with allergic conjunctivitis, especially those with severe cases of AKC and VKC. For example, AKC has a high rate of complications of bacterial and viral corneal infections, and CL should be avoided. What can be affirmed from this study is that even in patients with severe allergic conjunctivitis, it has become possible to wear CL by using ARCL if conjunctivitis can be controlled.
In conclusion, ARCL can be a useful tool for CL users with allergic conjunctivitis. However, ARCL should be introduced after allergic conjunctivitis is considered asymptomatic and controlled enough. Furthermore, ARCL should be immediately discontinued if ocular-allergic symptoms flare after introducing ARCL.
Patient consent
Consent to publish this case report has been obtained from the patients in writing.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Disclosure statement
AF received consultation fees from Santen and Johnson and Johnson, and lecture fees from Santen, Senju, Johnson and Johnson, Rohto-Nitten and Novartis. The following authors have no financial disclosures: HT, YT, KY, HT.
Additional information
Funding
References
- Kumar P, Elston R, Black D, et al. Allergic rhinoconjunctivitis and contact lens intolerance. CLAO J. 1991;17(1):31–34.
- Butrus SI, Abelson MB. Contact lenses and the allergic patient. Int Ophthalmol Clin. 1986;26(1):73–81. doi:10.1097/00004397-198602610-00011.
- Ackerman S, Smith LM, Gomes PJ. Ocular itch associated with allergic conjunctivitis: latest evidence and clinical management. Ther Adv Chronic Dis. 2016;7(1):52–67. doi:10.1177/2040622315612745.
- Garg SJD, Meyer D, eds. Step by Step Clinical Diagnosis and Management of Ocular Allergy. New Delhi: Jaypee Brothers; 2007.
- Pall B, Gomes P, Yi F, Torkildsen G. Management of ocular allergy itch with ocular allergy itch with an antihistamine-releasing contact lens.antihistamine-releasing contact lens. Cornea. 2019;38(6):713–716. doi:10.1097/ICO.0000000000001911.
- Miyazaki D, Takamura E, Uchio E, et al. Japanese guidelines for allergic conjunctival diseases 2020. Allergol Int. 2020;69(3):346–355. doi:10.1016/j.alit.2020.03.005.
- Polse KA. Tear flow under hydrogel contact lenses. Invest Ophthalmol Vis Sci. 1979 Apr;18(4):409-13.–413. PMID: 429114.
- Jones LW, Byrne M, Ciolino JB, et al. Revolutionary future uses of contact lenses. Optom Vis Sci. 2016;93(4):325–327. doi:10.1097/OPX.0000000000000847.
- Phan CM, Weber S, Mueller J, et al. A rapid extraction method to quantify drug uptake in contact lenses. Transl Vis Sci Technol. 2018;7(2):11. doi:10.1167/tvst.7.2.11.
