ABSTRACT
Purpose
This study aims to understand the practice patterns among ophthalmologists in North America who manage patients with acute, non-infectious anterior uveitis.
Methods
An eight-question survey was designed to elucidate the practice patterns of ophthalmologists across various geographic locations and practice settings regarding the management of anterior uveitis. This survey was distributed via the American Uveitis Society and Young Uveitis Specialists email listserv to ophthalmologists who self-identify as uveitis specialists and have a patient population that is at least 30% uveitis.
Results
A total of 102 responses were received and analyzed (37% response rate). Respondents practiced predominantly in North America, and 40% had received subspecialty training in uveitis. All respondents chose topical corticosteroid therapy as first-line treatment for acute, unilateral, or bilateral non-infectious idiopathic anterior uveitis. The most common initial frequency for prednisolone acetate administration was six times/day while the patient was awake (29.7%) and patients are typically seen in follow-up within a week (75% of respondents). If there is a lack of treatment response within 2–3 weeks with the initial topical treatment, 42 respondents (41.2%) chose to switch to difluprednate eye drops and 29 (28.4%) recommended switching to oral prednisone.
Conclusion
Our results show that topical corticosteroid, most frequently prednisolone acetate 1%, is the treatment of choice for patients with acute noninfectious anterior uveitis. Reported initial medication dosing and follow-up care approaches are highly variable, which suggests heterogeneity in practice patterns. Further research on the optimal initial dosing is needed.
Anterior uveitis is the most common type of ocular inflammatory disease, seen in 81% of total uveitis. Population-based studies in various regions of the United States have found the prevalence of uveitis to vary from 57.5 to 115.3 cases per 100,000 persons.Citation1–3 A large retrospective cohort study utilizing the Systemic Immunosuppressive Therapy for Eye disease cohort study (SITE) database followed 102 patients with a first episode of anterior uveitis who were seen within three months of disease onset.Citation4 Forty patients (40%) had a recurrence of anterior uveitis at some point in the 165 person-year follow-up period. The incidence of relapse was 24% per person-year (95% confidence interval [CI], 17%–33%). At 1.5 years after remission, 61% (95% CI, 48%–71%) remained in remission.Citation4
The exact pathophysiology of non-infectious anterior uveitis remains unclear. It is commonly thought to involve both environmental and genetic factors, and it has been found to be associated with multiple systemic inflammatory diseases and MHC alleles in recent genetic analysis.Citation5,Citation6
A common approach for initial management is to use topical corticosteroid drops. If unresponsive, management often is escalated to regional or systemic treatment with prednisone. Current literature lacks clear evidence-based guidelines on the optimal drop frequency that best controls non-infectious acute anterior uveitis and subsequent tapering regimens. These decisions may vary based on the clinician’s experience and training. Additionally, the use of chronic, suppressive topical corticosteroids requires close monitoring of patients for treatment response and side effects, which may contribute to the complexity and variability of follow-up visits.Citation7 More recently, two non-inferiority trials showed that difluprednate drops used four times daily were non-inferior to prednisolone acetate every two hours for two weeks.Citation8,Citation9 Notably, these studies only found one case of treatment failure with difluprednate therapy as compared to 10.6% in those treated with prednisolone acetate. However, in practice, the usage of prednisolone acetate and difluprednate vary widely, probably based on clinician decision, cost, insurance coverage, and the presumed need for difluprednate for more severe inflammation.
Most patients (60%) will remain in remission following adequate initial treatment of acute anterior uveitis, and many treatment variations exist in actual practice.Citation4 To understand the distribution of approaches in disease management, we undertook a survey of uveitis specialists who were members of the American Uveitis Society as to their preferred approach in treating typical acute anterior uveitis.
Materials and methods
This survey received an exemption from the Institution Review Board of Vanderbilt University Medical Center. An eight-question survey (Supplement 1) was designed to include a mixture of single-choice and multiple-selection questions with space to input additional specifications when applicable. Study data were collected and managed using REDCap (Research Electronic Data Capture) – a secure, web-based software platform supporting data capture for research studies hosted at Vanderbilt University Medical Center.Citation10,Citation11
This survey was shared via email to the American Uveitis Society (AUS) and Young Uveitis Specialists (YUS) email listserv. Where there was an overlap with the YUS listserv, as the majority are AUS members; participants were permitted to submit only a single survey response. Responses were collected from February 2021 through July 2021. The first six items on the survey gathered background information from participating physicians including practice type, subspecialty area, years of practice, and the frequency of encounters with patients with acute anterior uveitis in the past year (Supplement 1, Q1–6).
Next, the survey asked for the choice of first-line treatment in a hypothetical clinical situation describing a case of unilateral, idiopathic, non-infectious acute anterior uveitis in adults with no prior history of similar episodes or underlying rheumatologic conditions (Supplement 1, Q7). Under topical corticosteroid drops, respondents reported the dosages (frequencies) of the specific medication (prednisolone acetate, difluprednate, fluorometholone, loteprednol, or dexamethasone eye drops) they preferred. For depot corticosteroid injection, respondents selected from a list including subtenon’s injection of triamcinolone acetonide (Kenalog®) or intravitreal injection of preservative-free triamcinolone acetonide, dexamethasone implant, or fluocinolone acetonide intravitreal implant. The dosages were inquired for those who chose systemic medication (oral prednisone or intravenous methylprednisone) as their first-line treatment option. For dosing data interpretation, responses given as a range were counted together with individual dosages (i.e., “6–8×” was counted as one dose of six to eight times/day inclusive). Respondents were then asked to indicate how frequently they monitor patients with active uveitis under treatment.
A follow-up hypothetical scenario described a similar case of primary acute anterior uveitis but with bilateral involvement, and again respondents were required to state their preferred first-line management with dose and frequency of use. Lastly, respondents were queried about how they manage situations where the non-infectious anterior uveitis does not respond to frequent dosing of topical corticosteroid, even after 2–3 weeks of treatment (Supplement 1, Q8), to gauge the respondents’ second-line management regimen.
Results
One hundred and two uveitis specialists responded to the survey (response rate 36.3%), out of 281 uveitis specialists who were included in the AUS directory at the time of the survey. The reported location of practice was predominantly in North America (n = 89, 87.3%). The respondents predominantly practiced in university (n = 38, 37.3%) and private practice (n = 45, 44.1%) settings. Respondents had practiced a median of six to ten years in practice (range: ≤three years to ≥20 years). In the year preceding the survey, the respondents encountered an average of 25.4 patients (median, 5; standard deviation [SD], 76.9) with acute or recurrent acute anterior uveitis seen per month. Additional details of respondent demographics are reported in . Most respondents had received subspecialty training in Uveitis (n = 42) or Retina (n = 44), with 18 having received training in both. A total of 31 (30.4%) respondents reportedly spent more than 50% of combined clinical and surgical time treating uveitis ().
Figure 1. Subspecialty training and primary practice area of survey respondents. *More than one option could be selected.
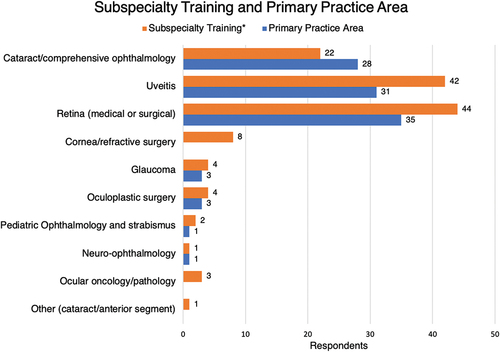
Table 1. Respondent backgrounds.
In response to the description of a hypothetical adult patient with unilateral, non-infectious, acute anterior uveitis, all 102 survey respondents chose to prescribe topical corticosteroid drops as their first-line intervention (). Prednisolone acetate 1% received the highest reporting of dosages (101 responses) with the most common frequency being six times/day while the patient is awake (30 responses, 29.7%). The most common frequency for other medications was four times/day (22 responses) for difluprednate. Seventy-six (74.5%) respondents chose to see the patient back within one week, and the rest of the responses ranged from two weeks to more than four weeks (median: one week or less).
Figure 2. Top bars - survey responses to question 7a (what is your first line treatment for an adult with one week of unilateral right eye pain and redness, visual acuity OD 20/40, IOP 14 and 2+ anterior chamber cell? Rest of the exam is within normal limits with cup-to-disk ratio of 0.3 in the right eye); bottom bars – survey responses to question 7c (what would be your first line treatment if there was bilateral AC cell 2+ or more? The rest of the exam is within normal limits with cup-to-disk ratio of 0.3 in both eyes).
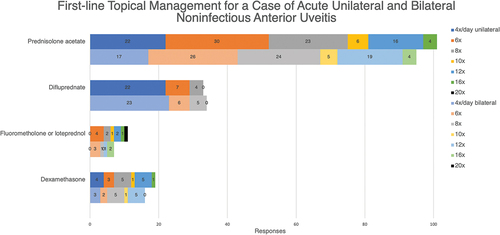
When asked to choose the first-line treatment for a similar patient with bilateral 2 + or more anterior chamber cells, 95 out of 102 respondents (93.1%) selected topical corticosteroid drops (). Six out of 102 respondents chose systemic medication with oral prednisone, and one chose depot corticosteroid injection with subtenon’s injection of triamcinolone acetonide (Kenalog®) 40 mg. Again, prednisolone acetate 1% received the most reporting of dosages (95 responses), with six times/day still being the frequency of choice (26 responses, 27.4%).
Figure 3. Survey responses to question 8 (if a patient continues to have active inflammation (AC cell 1+ or more) after being on every 2 hours prednisolone acetate drops for 2–3 weeks, what would you do? (Non-infectious uveitis)).
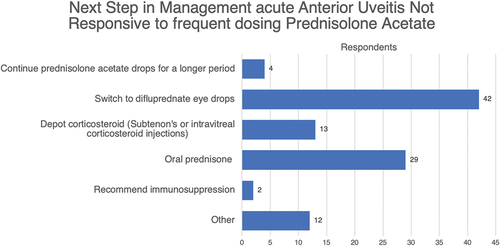
Lastly, among the respondents’ preferences for a patient who continues to have active inflammation after being on every-two-hour prednisolone acetate drops for two to three weeks, only four (3.9%) recommended continuing prednisolone acetate drops for a longer period. Forty-two respondents (41.2%) chose to switch to difluprednate eye drops, 29 (28.4%) recommended switching to oral prednisone, 13 (12.7%) recommended depot corticosteroid injection, and two (2%) chose immunosuppression. Other responses (12, 11.8%) included obtaining a workup for infectious or associated systemic disease etiology and referring to a retina or uveitis specialist (response chosen by those not trained in uveitis). Five respondents provided dosing for the oral prednisone therapy in refractory cases of 1.0 mg/kg/day up to 60 mg/day.
Discussion
Corticosteroids exert their anti-inflammatory effects through the activation of glucocorticoid receptors, leading to downstream inhibition of neutrophil migration and tissue proliferation.Citation12 Topical application of corticosteroids, which is followed by quick penetration of the cornea into the anterior chamber, confers a therapeutic advantage by minimizing systemic side effects. The potency of different preparations of topical corticosteroids depends largely on their chemical characteristics (i.e., presence of functional groups). The acetate group in prednisolone and difluprednate allows for substantial corneal penetration, while the ester group in loteprednol potentiates rapid intraocular inactivation and has demonstrated effects on lowering intraocular pressure in animal models.Citation13,Citation14 Furthermore, the prednisolone acetate-derivative difluprednate contains two additional fluorine groups, leading to favorable tissue penetration and theoretically less need for frequent dosing in clinical practice.Citation8,Citation15
In actual practice, selecting the optimal treatment against anterior uveitis often depends on the cost and availability of medication as well as patient-specific factors. Our results revealed topical corticosteroid to be the unanimous first-line treatment of choice for idiopathic, non-infectious acute anterior uveitis. Bilateral involvement of the disease upon initial presentation led a small portion of physicians to opt for systemic medications and depot corticosteroid injection. Regarding corticosteroid dosing, our data support the conjecture that topical prednisolone acetate is often utilized as the first-line agent in the treatment of anterior uveitis. Our findings are consistent with the maxim “hit hard, hit fast” concerning the general pattern of corticosteroid use commonly described in Ophthalmology literature.Citation16,Citation17
Prior literature analyzing the recurrence of anterior uveitis found comparatively higher relapse rates amongst the younger population (<18 and 18–35 years of age), while other factors such as sex, race, and the presence of spondyloarthropathy did not significantly contribute to relapse.Citation4 Our data indicate that patients are typically seen back quickly (one week or less), and persistent inflammation despite a two to three-week course of prednisolone acetate led many ophthalmologists to switch to stronger potency drops such as difluprednate drops. Additionally, many chose to escalate treatment to systemic therapy with oral prednisone and depot corticosteroid injections (Subtenon’s or intravitreal) for patients who do not respond to initial therapy. Our results showed a practice pattern consistent with the current guideline for the initial dose of prednisone: 1.0 mg/kg/day up to a maximum of 60 mg/day.Citation18,Citation19 The step-wise escalation of treatment for chronic uveitis has been well described, and recent consensus guidelines for the management of viral anterior uveitis were published by the TITAN group.Citation19,Citation20 However, guidelines on the management of acute primary anterior uveitis do not yet exist.
The strengths of this study include responses from uveitis-practicing ophthalmologists across various geographic locations, clinician age, and training background, and type of practice – primarily academic or private. Limitations include most responses being from North America, which may skew the results to reflect the landscape of commercial insurance-based practice as most uveitis patients tend to be young adults. The survey was quite specifically directed towards hypothetical first episodes of primary acute non-infectious anterior uveitis that were severe (2+ or more anterior chamber cells) and with no evidence of high intraocular pressure, which may alter the management plan. The heterogeneity of anterior uveitis leads to patients presenting with varied grades of anterior chamber inflammation, and typically the etiology is unknown at the time of the first visit.
In summary, acute noninfectious anterior uveitis is overwhelmingly managed by topical corticosteroids and until specific guidelines are developed, the following guidelines should be followed. First, rule out infectious causes that are prevalent in the community, based on endemicity. Topical drops can begin concurrently while awaiting testing to be completed. Second, do not taper topical corticosteroid until the eye is completely quiet, and then the taper drops completely. Third, do not use topical corticosteroids for prevention of recurrence as chronic use can cause cataracts and glaucoma. Lastly, persistent inflammation warrants transitioning to systemic immunosuppressive medications. Further studies focusing on the correlations between patient demographics and physician preferences for anterior uveitis treatment may elucidate more specific practice patterns regarding disease remission and relapse. Further investigation into the specific tapering regimens of physicians treating refractory uveitis may also help identify trends in the management of severe cases.
Research ethics approval
Human Participants: This was a deidentified survey. IRB was exempted.
Supplemental Material
Download Zip (36 KB)Disclosure statement
Sapna S. Gangaputra: NEI (Grant support); RPB (Grant support)
John H. Kempen: Betaliq (Equity Owner); Tarsier Pharma (Equity Owner).
None of the other authors had any conflicts to disclose.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/09273948.2024.2346819.
Additional information
Funding
References
- Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California epidemiology of uveitis study. Ophthalmology. 2004;111(3):491–500. doi:10.1016/j.ophtha.2003.06.014.
- Suhler EB, Lloyd MJ, Choi D, Rosenbaum JT, Austin DF. Incidence and prevalence of uveitis in Veterans Affairs medical centers of the Pacific Northwest. Am J Ophthalmol. 2008;146(6):890–896. doi:10.1016/j.ajo.2008.09.014.
- Acharya N, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, et al. Incidence and prevalence of uveitis: results from the pacific ocular inflammation study. JAMA Ophthalmol. 2013;131(11):1405–1412. doi:10.1001/jamaophthalmol.2013.4237.
- Grunwald L, Newcomb CW, Daniel E, Kacmaz RO, Jabs DA, Levy-Clarke GA, et al. Risk of relapse in primary acute anterior uveitis. Ophthalmology. 2011;118(10):1911–1915. doi:10.1016/j.ophtha.2011.02.044.
- Takeuchi M, Mizuki N, Ohno S. Pathogenesis of non-infectious uveitis elucidated by recent genetic findings. Front Immunol. 2021;12. doi:10.3389/fimmu.2021.640473.
- Wakefield D, Clarke D, McCluskey P. Recent developments in HLA B27 anterior uveitis. Front Immunol. 2020;11. doi:10.3389/fimmu.2020.608134.
- Oray M, Tuğal-Tutkun İ. Treatment of juvenile idiopathic arthritis-associated uveitis. Turk J Ophthalmol. 2016;46(2):77–82. doi:10.4274/tjo.09581.
- Sheppard JD, Foster CS, Toyos MM, Markwardt K, Vanzo RD, Flynn TE, et al. Difluprednate 0.05% versus prednisolone acetate 1% for endogenous anterior uveitis: pooled efficacy analysis of two phase 3 studies. Ocul Immunol Inflammation. 2019;27(3):484–496. doi:10.1080/09273948.2017.1407433.
- Sheppard JD, Toyos MM, Kempen JH, Kaur P, Foster CS. Difluprednate 0.05% versus prednisolone acetate 1% for endogenous anterior uveitis: a phase III, multicenter, randomized study. Invest Ophthalmol Vis Sci. 2014;55(5):2993–3002. doi:10.1167/iovs.13-12660.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi:10.1016/j.jbi.2008.08.010.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019; 95:03208 doi:10.1016/j.jbi.2019.103208.
- Busillo JM, Cidlowski JA. The five rs of glucocorticoid action during inflammation: ready, reinforce, repress, resolve, and restore. Trends Endocrinol Metab. 2013;24(3):109–119. doi:10.1016/j.tem.2012.11.005.
- Valdes LM, Sobrin L. Uveitis therapy: the corticosteroid options. Drugs. 2020;80(8):765–773. doi:10.1007/s40265-020-01314-y.
- Samudre SS, Lattanzio FA Jr, Williams PB, Sheppard JD Jr. Comparison of topical steroids for acute anterior uveitis. J Ocul Pharmacol Ther. 2004;20(6):533–547. doi:10.1089/jop.2004.20.533.
- Bodor N, Harget AJ, Phillips EW. Structure-activity relationships in the antiinflammatory steroids: a pattern-recognition approach. J Med Chem. 1983;26(3):318–328. doi:10.1021/jm00357a003.
- Dinh R, Do BK. Steroid options for treatment of uveitis. Retinal Physician. 2023;36:32–34.
- Weiner G. Savvy steroid use. EyeNet Magazine. February, 2013.
- Jabs DA. Immunosuppression for the uveitides. Ophthalmology. 2019;125(2):193–202. doi:10.1016/j.ophtha.2017.08.007.
- Jabs DA, Rosenbaum JT, Foster CS, Holland GN, Jaffe GJ, Louie JS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol. 2000;130(4):492–513. doi:10.1016/S0002-9394(00)00659-0.
- Thng ZX, Putera I, Testi I, Chan K, Westcott M, Chee SP, et al. TITAN consensus guidelines group. The infectious uveitis treatment algorithm network (TITAN) report 1-global current practice patterns for the management of herpes simplex virus and varicella zoster virus anterior uveitis. Eye (Lond). 2024;38(1):61–67. doi:10.1038/s41433-023-02630-9.
