ABSTRACT
A fixation preference for the affected eye is uncommon in patients with unilateral Duane retraction syndrome (DRS), and surgery on the fellow eye is rarely advocated. We are presenting a case report of a 9-year-old boy with unilateral DRS type II in the left eye who received lateral rectus muscle recession in his right amblyopic eye. The patient was orthophoric and his face turn was gone 6 months postoperatively. Surgery on the fellow amblyopic eye is a good choice for unilateral DRS where the affected eye dominants the fixation, and the satisfactory outcome suggests that alignment in the primary position can correct the face turn effectively despite the muscle duction deficit in the affected eye and further extend the binocular single visual field.
Introduction
Duane retraction syndrome (DRS) is a rare congenital eye movement disorder caused by hypoplasia or absence of the sixth cranial nerve and nuclei combined with dysinnervation of one or two branches of the oculomotor nerve.Citation1 It is characterized by horizontal ocular motility deficit, ocular deviation in the primary position, retraction of the globe, and narrowing of the palpebral fissure during attempted adduction, which are caused by the simultaneous contraction of the medial and lateral rectus muscles.Citation2,Citation3 Associated in many cases of DRS is an upshoot or downshoot: a “flipping” up or down movement which occurs when the eye moves above or below the horizontal plane in an adducted position. This abnormality is considered to be related to a sudden slippage of the tight lateral rectus muscle over the globe.Citation4 Patients who showed esotropia or exotropia commonly adopt a face turn to maintain binocular single vision and make up for the duction deficit, depending on which duction is maximally affected.Citation5,Citation6 Huber categorized DRS into three types according to electrophysiology, among which type II (4–13%) is the least common presentation and presents with poor eye adduction and exotropia.Citation1
3–25% of patients with DRS suffer from amblyopia, while strabismus and anisometropia were considered as strong reasons among studies.Citation7–9 In a majority of cases, the unaffected eye is the dominant eye for those patients who exhibit fixation preferences with unilateral DRS (80–90% of the cases).Citation7,Citation10 Currently, only a few cases with fixation preference for the affected eye have been reported. But these cases were all DRS type I.Citation7,Citation11,Citation12 In this case, it is DRS type II which is different from the previous reports.
In the treatment of unilateral DRS, surgery on the involved eye is recommended by most authors. For a patient who is exotropic in the primary position, an ipsilateral lateral rectus recession for deviations <20D and a bilateral lateral rectus recession for deviations >20D are widely adopted. In addition, Y-splitting recession of the ipsilateral rectus muscle is considered a reliable surgical option in some patients with significant overshoot.Citation13,Citation14 Surgery restricted on the fellow eye is rarely advocated.Citation15 Here, we present a case report of a child patient with unilateral DRS who received lateral rectus muscle recession in his fellow amblyopic eye and obtained a satisfactory outcome.
Case presentation
A 9-year-old boy was presented to our hospital due to an outward deviation in his right eye for 3 years. He has no history of ocular trauma or ocular surgery, and his birth and development were not affected.
On examination, the patient showed moderate horizontal torticollis, with a right-sided face turn of 40° while reading the distance vision chart. The best-corrected visual acuity was 20/16 in his left eye and 20/32 in the right eye. Cycloplegic refraction manifested anisometropia, +1.00DS/-0.50DC×1 in the left eye and +1.75DS/-3.50DC×5 in the right eye. Anterior segment and retinal examinations were unremarkable. In the primary position of gaze, the patient presented with 15 prism diopters (PD) exotropia, L/R 5PD in primary position measured with prism alternative cover test, and an angle kappa of zero degree in both eyes were noted (). Globe retraction of grade 2 of the left eye in dextroversion was observed.Citation16 Hertel exophthalmometer measurements were 12 mm OD and 12 mm OS in primary gaze, 12 mm OD and 9 mm OS in 30° dextroversion, and 12 mm OD and 12 mm OS in 30° levoversion. Besides, an upshoot of the left eye was noted as the globe adducts (grade 4) and moves above the horizontal plane (grade 3) in adduction, respectively, but no downshoot was present.Citation16 Adduction was mildly limited in the left eye, while the extraocular movement was full in the right eye (). Force duction test revealed no contracture in both eyes. Synoptophore test showed fusion field arranging from −7° to +8°. In diplopia quantification using the cervical range of motion (CROM) method, binocular single vision appeared exclusively in 30° of left gaze and habitual reading gaze, and the score was 84 ().
Figure 1. Head posture and eye position of the patient. Preoperative (a) and postoperative (b) head posture and eye position in the patient with DRS. The patient was orthotropic without abnormal head position after 6-mm lateral rectus recession
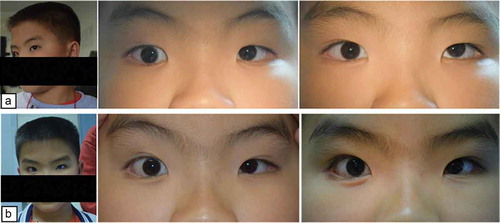
Figure 2. 9-gaze photographs of the patient. (a) 9-gaze preoperative photographs showed mild limitation of adduction with globe retraction, palpebral fissure narrowing, and upshoot on attempted adduction of the left eye. (b) 9-gaze postoperative photographs showed mild-to-moderate limitation of adduction in the right eye with persistent symptoms in the left eye
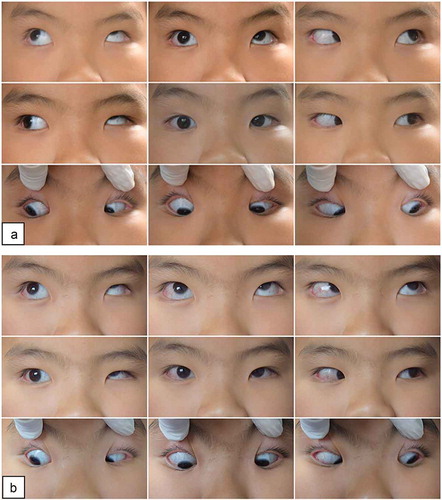
Figure 3. Results of cervical range of motion method. Single vision represented by white point and diplopia by black point. Point below 30° represents habitual reading gaze. (a) Preoperative cervical range of motion diplopia scored 84. (b) Postoperative cervical range of motion diplopia scored 6
He was diagnosed with exotropic DRS in the left eye. A 6-mm right lateral rectus recession was performed in his right eye. No extraocular muscle abnormalities were found. Postoperatively, the patient was orthotropic for distance and near in primary gaze, with resolved face turn in 6 months (). There was mild limitation of abduction in the right eye and adduction in the left eye, but no manifest strabismus in the horizontal gaze position except for the full right gaze, where the upshoot remained in the left eye. Globe retraction and upshoot in right gaze in the left eye remained unchanged (). The score of CROM diplopia examination was 6 as diplopia only appeared in 30° of right gaze ().
Discussion
Single horizontal rectus muscle recession of the affected eye in these cases was proposed by Duane in 1905 and has been widely used due to its simplicity, reliable correction of primary deviation as well as abnormal face turn for deviation less than 20PD.Citation3,Citation14 Moreover, recession of lateral rectus in Duane’s eye can simultaneously diminish globe retraction, palpebral fissure narrowing, and up/down shoot in adduction.Citation11 However, recession of the ipsilateral lateral rectus muscle may worsen the abduction limitation and increase the esotropia in lateral gaze postoperatively, while the small recession in the fellow eye is adequate to realign the eye in primary position without this complication.Citation15
Surgery on the fellow eye is rarely advocated. Several authors declared that weakening of the rectus muscles in the normal eye can balance the duction deficit and thereby expand the binocular single visual (BSV) field.Citation15 In addition, when the unaffected eye is the dominant eye, this procedure can reduce the likelihood of any recontracture in the DRS eyes simultaneously, according to Sherrington’s and Hering’s laws.Citation11,Citation17 However, Duane’s syndrome is a disorder in which Sherrington’s and Hering’s laws do not apply. Thus, this theory, in which “fixation duress” plays a significant role, remains doubtful. As far as we are aware, operation restricted in the fellow eye has not been reported and discussed before in the case that the affected eye is the dominant eye.
Amblyopia in the fellow eye could be due to long-term uncorrected anisometropia in this patient. Based on his examination and his parents’ operation preference on the “bad” eye, we performed a 6-mm lateral rectus recession on the amblyopic right eye. The patient was orthophoric at distance and near, and his face turn was gone 6 months postoperatively. This suggests that alignment in the primary position can correct the face turn effectively despite the muscle duction deficit in the affected eye. Since the primary goal for surgery in DRS is the correction of primary position deviation and torticollis,Citation12 single contralateral rectus recession may be a proper choice for a patient with poor visual acuity in the fellow eye when the affected eye can reach the midline.
Since a precise measurement of BSV field using the Goldmann perimeter was unavailable due to the noncooperation of the child, we adopted the CROM method instead. This method has been recommended as a simple alternative to the Goldmann perimeter for quantifying diplopia.Citation18 In this case, the CROM score dipped significantly from 84 preoperation to 6 postoperation, indicating an extended BSV field with balanced horizontal rotations. Besides, we noticed a disappearance of vertical deviation along with correction of horizontal deviation by recession of the lateral rectus muscle. Further studies are needed to explore the underlying mechanisms.
This case suggests that surgery restricted on the fellow eye is a good choice to obtain alignment in the primary position, correct the face turn, and further extend the BSV field for unilateral DRS where the affected eye dominants the fixation.
Ethics approval and consent to participate
This study followed the tenets set forth in the Declaration of Helsinki, and approval was obtained from the Ethics Committee of the Zhongshan Ophthalmic Center of Sun Yat-sen University.
Consent for publication
Written informed consent was obtained from the guardian for publication of this case report and any accompanying image consent.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KM designed the study and was a major contributor in writing the manuscript. XY and KD analyzed and interpreted the patient data and substantively revised the manuscript. LC collected the data and checked and revised the manuscript and participated in the surgery as the first aider. XL designed the study, performed all the treatments, and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
References
- Huber A. Electrophysiology of the retraction syndromes. Br J Ophthalmol. 1974;58(3):293–300. doi:10.1136/bjo.58.3.293.
- Yuksel D, Orban de Xivry JJ, Lefevre P. Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification. Vision Res. 2010;50(23):2334–2347. doi:10.1016/j.visres.2010.08.019.
- Duane A. Congenital deficiency of abduction, associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. 1905. Arch Ophthalmol. 1996;114(10):1255–1256;discussion 1257. doi:10.1001/archopht.1996.01100140455017.
- Greenberg MF, Pollard ZF. Poor results after recession of both medial rectus muscles in unilateral small-angle Duane’s syndrome, type I. J Aapos. 2003;7(2):142–145. doi:10.1016/S1091-8531(02)42001-0.
- Park WH, Son DH, Yoon SW, Baek SH, Kong SM. The clinical features of Korean patients with Duane’s retraction syndrome. Korean J Ophthalmol. 2005;19(2):132–135. doi:10.3341/kjo.2005.19.2.132.
- Kekunnaya R, Negalur M. Duane retraction syndrome: causes, effects and management strategies. Clin Ophthalmol. 2017;11:1917–1930. doi:10.2147/OPTH.S127481.
- DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane’s retraction syndrome. Surv Ophthalmol. 1993;38(3):257–288. doi:10.1016/0039-6257(93)90077-K.
- Mohan K, Sharma A, Pandav SS. Differences in epidemiological and clinical characteristics between various types of Duane retraction syndrome in 331 patients. J Aapos. 2008;12(6):576–580. doi:10.1016/j.jaapos.2008.04.015.
- Kekunnaya R, Gupta A, Sachdeva V, et al. Duane retraction syndrome: series of 441 cases. J Pediatr Ophthalmol Strabismus. 2012;49(3):164–169. doi:10.3928/01913913-20111101-01.
- Raab EL. Clinical features of Duane’s syndrome. J Pediatr Ophthalmol Strabismus. 1986;23:64–68.
- Jampolsky A. Strategies in strabismus surgery. Trans New Orleans Acad Ophthalmol. 1986;34:363–398.
- Khan AO, Oystreck DT. Fixation preference for the affected eye in patients with unilateral Duane syndrome. J Aapos. 2006;10(3):275–276. doi:10.1016/j.jaapos.2006.01.009.
- Kekunnaya R, Kraft S, Rao VB, Velez FG, Sachdeva V, Hunter DG. Surgical management of strabismus in Duane retraction syndrome. J Aapos. 2015;19(1):63–69. doi:10.1016/j.jaapos.2014.10.019.
- Akbari MR, Manouchehri V, Mirmohammadsadeghi A. Surgical treatment of Duane retraction syndrome. J Curr Ophthalmol. 2017;29(4):248–257. doi:10.1016/j.joco.2017.08.008.
- Saunders RA, Wilson ME, Bluestein EC, Sinatra RB. Surgery on the normal eye in Duane retraction syndrome. J Pediatr Ophthalmol Strabismus. 1994;31:162–169;discussion 170–161.
- Kekunnaya R, Moharana R, Tibrewal S, Chhablani PP, Sachdeva V. A simple and novel grading method for retraction and overshoot in Duane retraction syndrome. Br J Ophthalmol. 2016;100(11):1451–1454. doi:10.1136/bjophthalmol-2016-309194.
- Kraft SP. A surgical approach for Duane syndrome. J Pediatr Ophthalmol Strabismus. 1988;25:119–130.
- Hatt SR, Leske DA, Holmes JM. Comparing methods of quantifying diplopia. Ophthalmology. 2007;114(12):2316–2322. doi:10.1016/j.ophtha.2007.01.033.
