ABSTRACT
To review and evaluate the surgical outcomes of the Fells-modified Harada-Ito procedure using a dosage scale approach with long-term follow up in patients with torsional diplopia. The records of patients who underwent the modified Harada-Ito procedure by the same surgeon during 2012–2019 were retrospectively reviewed regarding pre- and post-operative data and individual dose-scale used for the surgery. The modified Harada-Ito procedure involved advancing the anterior half of the superior oblique tendon toward the inferior edge of the lateral rectus muscle by a distance determined using a five-graded scale. A total of 27 patients (mean age 57.6 years, range, 22–81 years; 10 female) were included. Evaluating surgical outcome showed a significant difference in pre- to post-operative cyclodeviation (p = <0.001). Pre-operative mean extorsion was −10.4° and mean torsional correction achieved was 7.7°. The dose-effect relationship showed a wide spread effect, yet yielded a high success rate. All but two patients were symptom free from their torsional diplopia at the last post-operative evaluation, on average 24 months after surgery. Post-operative results and the dose-effect of the modified Harada-Ito corresponded with the aimed-for correction of torsional diplopia.. Fusion evaluation and individually based pre-operative assessments proved essential in determining individual doses for successful surgical outcomes.
Introduction
Torsional diplopia occurs due to an increase and/or a decompensation in cyclodeviation. Fusional reserves become inadequate and fusion disruptions occur, leaving patients symptomatic. The most common cause of torsional diplopia is superior oblique palsy.Citation1 Patients display extorsional diplopia and require corrective surgery to alleviate symptoms and regain fusion. The Harada-Ito procedure is frequently the surgical method of choice, and was first described in 1964.Citation2 It involves the anterior part of the superior oblique tendon being pulled laterally in the direction of action. In 1974, Fells introduced a modification to the procedure, whereby the anterior half of the superior oblique tendon is disinserted and split from the posterior portion, followed by an anterolateral transposition to the lateral rectus (LR) muscle.Citation3 Metz and Learner further developed the procedure in 1981 by adding an adjustable suture technique,Citation4 and Boergen modified the method in 1987 (reported by Ehrt and Boergen in 2004), using a loop of non-resorbable suture to pull the anterior part of the tendon.Citation5
The Harada-Ito procedure is well described in the literatureCitation3,Citation6,Citation7 as an effective method of treatment for torsional diplopiaCitation8–10 and successfully reduces excyclodeviation and decreases symptoms.Citation11 However, there are still few published data on exact surgical measures versus outcomes, and quantitative data on the pre-operative angle and effect of the operation as well as long-term results are lacking.
The aim of this study was to review the surgical outcomes of the Fells-modified Harada-Ito procedure using a dosage scale approach with long-term follow-up. How much reduction in cyclodeviation is required to make the patient asymptomatic from torsional diplopia, and what can be deemed a successful surgical result in this patient group? Moreover, the purpose was also to evaluate the relationship between pre-operative factors and the final outcome.
Materials and methods
The medical records of patients who underwent the modified Harada-Ito procedure at the Sahlgrenska University hospital using a dosage scale approach were retrospectively reviewed from 2012, when the technique was introduced, to 2019. All patients had undergone a full orthoptic and ophthalmological assessment and were found to have superior oblique palsies (SOPs) through various etiologies. The patients were selected for a Harada-Ito surgery rather than an inferior oblique recession as they all displayed torsion as the main issue. Data reviewed included etiology, ocular motility assessment, pre- and post-operative measurements, pre-operative fusion, details of surgical choice, post-operative outcomes, and time elapsed from surgery to the last post-operative assessment. The efficacy of the procedure was evaluated by comparing pre-operative with long-term post-operative torsion and reviewing how much effect was aimed to be achieved versus how much effect was attained. Success was defined as being free from torsional diplopia. All patients were examined and treated by the same orthoptist and surgeon during this 7-year period.
The study was approved by the Ethical Committee, and followed the tenets of the Declaration of Helsinki.
Pre-operative assessment
Torsion was primarily measured in straight ahead gaze or primary position (pp) and down using the single Maddox rod test (SMR) and the Clement Clarke synoptophore model 2003 (Haag-Streit UK Ltd, Harlow, UK) with Maddox slides (slide series A 17/18). A detailed description of the exact technique for the SMR test can be found in a previous publication,Citation12 which compares the two different methods. The SMR test is adequate for screening and monitoring torsion in clinic, but for surgical planning, subjective fusional information is required and the synoptophore is the more suitable method to assess torsion with preoperatively. In presence of a horizontal or vertical deviation, this was optically corrected in the synoptophore before measuring the cyclodeviation, which was recorded as the total amount, in degrees, of cyclotorsion present between both eyes. Fusion and cyclofusion were assessed using the synoptophore with slide series F fusion slides (F 9/10 House).
Surgery
The surgical technique used was the Fells-modified Harada-Ito procedure, but with a graded approach. The surgeon (PK) consistently used half the width of the anterior tendon of the superior oblique (SO) muscle for transposition. The new insertion of the SO tendon was according to the 5-graded scale, and the reinsertion was placed within the distance between the original insertion of the SO and 7–8 mm posterior of the LR muscle upper border. In the cases of the enhanced surgery, the SO tendon was reattached under the LR. shows the procedure and predicted effect. Thus, each surgery was “made to fit” individual anatomy rather than using the same mm measurement for each patient.
Figure 1. The graded modified Harada-Ito procedure in a left eye when transposing and reinserting the anterior segment of the superior oblique (SO) tendon, the dosage scale for the advancement position and the estimated effect, in degrees, on cyclodeviation is shown in enlargement (S.Flodin).
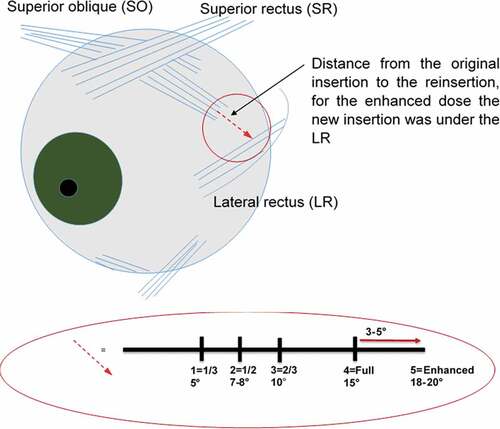
The aimed for correction and surgical dose were decided based on the amount of cyclodeviation present, the subjective comfort within the cyclofusion range, the subjective perception of tilted image in front of which eye, ocular motility restrictions and fixation preference.
Statistical analysis
As torsion was the barrier to fusion, only these measurements were statistically analyzed. For the SMR, the subjective torsion measurements of the operated eye pre- and postoperatively in straight-ahead gaze were assessed for surgical outcomes. Alignment data are presented as means, standard deviations (SD), medians, ranges, 95% CI and inter quartile ranges (IQRs); shown as first quartile and third quartile (Q1:Q3). The change in alignment from pre-op to final post-op was evaluated using the paired samples t-test and the Wilcoxon signed-rank test as implemented in the SPSS Statistics program, version 24 (IBM Corporation) and for comparison within groups the Fisher´s Non-Parametric Permutation test for paired observations was used. The effect of surgical-dose was estimated from a mixed model adjusted by within patient correlation and the number of eyes operated at each visit. In order to study the agreement between the SMR and synoptophore measurements the distribution of the differences of the changes, limits of agreement, tests of systematic differences and IntraClass correlation coefficient (ICC) were given. Bland Altman plot is also presented. Bivariate (Pearson) correlation and multivariate regression analysis were performed to investigate relationships between variables. Multiple regression analysis was performed for each independent variable predictor to determine which variables may have influenced the outcome of final amount of cyclodeviation postoperatively.
As there are few patients in the material and the data proved to be quite complex, a combination of parametric and non-parametric statistical analysis was undertaken. We used mixed models, which is a parametric test to estimate the surgical effect while taking into account the individual dependence that arises from repeated measurements.
Results
A total of 27 patients had undergone the modified Harada-Ito graded surgical procedure (mean age, 57.6 years; range, 22‒81 years; 17 men). Twenty-one patients underwent unilateral surgery (13 male, 8 female) while six needed bilateral procedures (4 male and 2 female). Etiology of the torsional diplopia included: head trauma (n = 12) most commonly caused by a road traffic accident (RTA) or a fall; idiopathic (n = 9); cerebrovascular incident (n = 2); post-operative retinal detachment (n = 1); brain tumor (n = 2) and a craniofacial deformity (n = 1). shows an overview of the basic characteristics of each individual. Although the majority of cases were severe due to head trauma, they had isolated SOPs and only one patient had a combined fourth and third nerve palsy (no 26).
Table 1. Basic characteristics of all the patients operated using a dosage scale approach to the modified Harada-Ito procedure
Three patients had additional horizontal and vertical surgery combined, one patient had horizontal surgery and six patients had vertical surgical procedures performed either before or after their surgical correction for cyclodeviation. The mean duration of post-operative follow-up was 25 months (range 3–89 months).
Effect of surgery on torsion in all 27 patients
Pre-operative mean extorsion of the operated eye as measured with the SMR for 27 patients was −10.4° and ranged from −30° to −0°. At the last post-operative evaluation, mean extorsion was −2.7° with a range from −10° to 0°. The mean torsional correction achieved with the graded modified Harada-Ito procedure for all the unilateral cases and the first surgery of the bilateral cases was 7.7° (95% CI 6.27; 9.21) and the change following surgery was significant (p < .001, Fisher´s Non-Parametric Permutation test for matched pairs). There were only ten patients measured both pre- and post-operatively with the synoptophore, and for these patients the mean pre-operative excyclodeviation was −10° and ranged from −30° to −0°. The change in deviation/correction was 7.6° (95% CI 2.00; 13.50) which was significant (p = .020). The relationship between the pre- and post-operative cyclodeviation measurements had a strong positive correlation, (r = 0.84, p < .001) the larger the deviation the greater the change after surgery.
Effect of surgery on torsion in unilateral and bilateral patients
The unilateral cases (n = 21) had a mean extorsion of −9.8° pre-operatively, reducing to −2.8° post-operatively, displaying a change of 7.0°. There was a significant improvement in torsion following surgery (95% CI −9.04; −5.10, p < .001, paired samples t-test) and within the individual dose scales with enough patients in each, to allow statistical analysis, dose-scale 3 (95% CI −8.39; −2.75, p = .003, n = 7) and dose-scale 4 (95% CI −11.96; −4.94, p < .001, n = 10). The bilateral cases (n = 6) displayed a pre-operative mean extorsion of −13.7°, reducing to −5.4° post-operatively, a change of 8.3°. The change after surgery was significant (95% CI −11.14; −5.53, p < .001) for all cases, and within dose scale 3 with enough patients in for statistical analysis (95% CI −14.72; −2.88, p = .014). There was a strong positive correlation between the pre- and post-operative torsion (r = 0.65, p = .002).
The mean extorsion for all operated eyes (n = 36) was −11.5° pre-operatively and −3.9° post-operatively, giving a mean reduction of 7.6°, which was significant (95% CI −9.16; −6.03, p < .001). The responses and outcomes per dose for the unilateral surgical procedures are shown in . The pre- and post-operative values and effect after surgery for the bilateral procedures and all eyes operated on are shown in .
Table 2. Torsion as measured in degrees using the single Maddox rod test (SMR) in unilateral surgeries (n = 21), showing surgical procedures performed, pre-and post-operative values and the change/effect per surgical dose
Table 3. Torsion as measured in degrees using the single Maddox rod test (SMR) in Bilateral cases (n = 6), Uni- and bilateral cases (n = 27) and all surgeries/eyes operated on (n = 36) showing pre-and post-operative values and the change/effect after surgery
Surgical outcomes long-term and the relationship of pre-operative factors
Post-operative results were rated as successful if there was a reduction of the extorsion to within the cyclofusion range, abolishing torsional diplopia in pp and downgaze. A failure was classified as having a remaining disabling torsional diplopia, leaving the patient unable to fuse. Overall, 25 patients regained cyclofusion after surgery at follow-up. The two patients classified as failure include one female (no 22, ) who measured no cyclodeviation post-operatively, but still perceived subjective intorsion as an overcorrection. The other patient (no 21, ) had remaining torsional diplopia post-operatively, and remains under treatment, needing additional surgery. One patient (no 8, ) had the planned dose changed from scale 3 to 1 during surgery due to finding an anatomical anomaly. Based on the last post-operative measurements from the 26 patients who have completed treatment, cyclodeviation should be within the span of ˗10° to 0° (IQR: −5.50; 0) in order to reach symptom relief. Two patients required several Harada-Ito surgeries before reaching target of becoming asymptomatic from torsional diplopia (no 23 and no 24 in .). These patients were classed as severe in terms of etiology and restricted ocular motility, having suffered severe head trauma and subarachnoid hemorrhage.
Two patients have incorporated vertical prisms for small angles of vertical deviations disrupting vertical fusion, and have full binocularity with glasses. These are still included as a success, as they have no disturbances from cyclodeviation. One elderly patient wears partial occlusion because of mechanical restriction in elevation. There were no other cases of post-surgical complications.
In the multiple linear regression analysis, the overall model explained a significant amount of variance in the outcome variable (R = 0.818). The individual effects of the predictors in the model showed that etiology was a significant predictor of surgical outcome (Beta = −0.435, SE = 1.470, p = .022). Age and gender as well as surgical procedure (unilateral or bilateral) were not significant predictors of surgical outcomes and efficacy. The overall model fit (the proportion of variation accounted for by the regression model) was 38% (R2 = 0.383.).
Agreement of change pre-operatively to post-operatively between SMR and synoptophore
The average difference between the change in the SMR and the synoptophore method showed a mean of −0.400 (95% CI −9.877; 9.077, SD = 4.84, p = .77, Wilcoxon Signed Rank test). This was not significant. The Bland–Altman plot of the Limits of Agreement () shows the interval within which we can expect that the difference for a new measurement of both methods will be in 95% of the cases.
Discussion
Symptomatic cyclodeviation is a troublesome condition. Patients are unable to regain cyclofusion unless the cyclodeviation is reduced through surgery. Data were retrospectively reviewed to evaluate the results of a dose-scale approach to the modified Harada-Ito procedure, the influence of our pre-operative assessments, etiology and what constitutes a successful surgical result in this group. Surgical success was achieved in 25 out of the 27 patients (93%). Our study shows a high success rate in terms of symptom relief, which remains at the last evaluation on average 24 months post-operatively. By comparison, previous studies in the field have reported success in 43% to 73% of patientsCitation9,Citation11,Citation13,Citation14. The modified Harada-Ito procedure has also been reported to have an effect in reducing vertical incomitance of horizontal deviation.Citation14 Post-surgical complications described from previous publications have included iatrogenic Brown syndrome, restrictive esotropia, and restricted motility.Citation5,Citation9,Citation13 We found none of these problems in our material. However, one elderly patient suffered a residual mechanical restriction in elevation post-surgery. The superior rectus muscle was extremely flaccid, and so the muscle function was affected by the Harada-Ito surgical procedure.
The results showed a post-operative extorsion mean of −2.6°. However, the results also demonstrate that some individuals with as much as −10° of residual excyclodeviation are satisfied with the outcome. Illustrating the range and variants of cyclofusional reserves in cyclodeviation, which may to some part depend on etiology. Normative cyclofusion has been found to have a total mean amplitude of 16°.Citation15 Furthermore, the results display a significant reduction in extorsion after surgery. The dose-scale evaluation of the graded surgical approach demonstrated a wide spread effect ( and .). Before reviewing the results, we assumed that we could develop a standard dose scale corresponding to the amount of cyclodeviation present (). However, this study has shown otherwise. The same amount of surgery for the same angle of deviation may yield different results in different patients.
Figure 3. Scatterplot showing the outcome effect of surgery on torsion per dose in 21 individuals after unilateral surgery.
Cyclofusion was a determining factor with regard to the dose of surgery. Once cyclodeviation in degrees was measured, the amount of reduction in deviation required to regain and maintain comfortable fusion was defined by mapping minimal and maximal thresholds (cyclofusion range and capacity). This in turn determined the dose of surgical correction deemed to give the desired effect. Other factors taken into consideration and influencing the choice of surgery were the subjective perception of the tilted image in front of each eye, and/or the paretic eye, ocular motility and the fixation pattern due to refraction. The dose scale gives a varied response as each dose is customized according to each patient’s fusional ability and need. Measuring out the repositioning of the tendon from the original insertion is dependent upon the distance and appearance of the eye bulb, and its motility. Individuals with large excyclodeviation or weak fusion showed less effect per dose, and required more stretch on the fibers to achieve more torsional elimination. Consequently, we cannot establish a standard measurement scale. The essence of achieving a successful result lies in the individually based pre-operative assessment, with the core being the cyclofusional evaluation. We therefore base our assessments for surgery on the amount of cyclodeviation present at the pre-operative assessment and the amount of compensatory image rotation in the synoptophore required to achieve cyclofusion. Patients rarely specifically complain of torsional symptoms unless prompted.Citation1 Therefore, it is essential to perform correct sensory and motor evaluations during pre-operative assessments in surgical management of strabismus patients in order to reach ultimate post-operative results.Citation16
A previous study exploring dose-response in esotropia surgery found that the surgical response was explained more by the pre-operative deviation than by the amount of surgery.Citation17 It has been described that assessing fusion using the synoptophore pre-operatively may give a better outcomeCitation11,Citation13,Citation18 and the orthoptist’s role in treatment of paralytic strabismus has been outlined since the 1960s.Citation19 This study demonstrates that a reliable orthoptic pre-operative assessment mapping the patient’s fusional capacities is just as important as the surgical technique in management of cyclodeviation, and that a dose scale needs to be very individual. It also highlights the importance of working closely together as a team in order to achieve the best results.
Previous studies have observed an excyclodrift in patients treated surgically for cyclodeviation,Citation14,Citation20,Citation21 which resulted in a preference of setting torsional alignment to an intorsional overcorrection.Citation20 Initial large overcorrection may reduce symptomatic extorsion reoccurrence in the long term.Citation22 This long-term decrease of the effect of the oblique-muscle surgery on the torsional angle was observed and hyopthesized to be caused by reversal of pre-operative adaptive changes.Citation23 The adjustable Harada-Ito advancement has a reported dose response of 1.3° per millimeter,Citation24 but this effect regresses over time and therefore an overcorrection of 7–10° intorsion should be aimed for.Citation21 Other studies report no evidence of the effects of surgery wearing offCitation8 or if it does, this occurs within six months of surgery.Citation11 The present study has a mean post-operative follow-up of 24 months, with the longest follow-up in one patient being 89 months. None of the patients in this cohort required additional surgery once the treatment plan was completed, nor did we aim for overcorrection. The pre-operative information regarding each patient’s fusion requirements governed the amount of correction aimed for and therefore the post-operative angle of cyclodeviation. Our dose response cannot transcribe to degrees per millimeter. Residual extorsion does not necessarily have to be a decreasing effect of the surgery; it may, instead, be due to strong and individual fusional abilities and amplitudes.
There are several limitations to this study. The SMR method is not an established method for measuring subjective torsion and the measurements are both greater and more variable than the synoptophore measurements, due to the dissociative nature of the SMR test. The discrepancy between measurements with the SMR and the synoptophore methods has been raised in a previous publication,Citation12 but has been found to give repeatable results and can be relied upon measuring torsion within the same subject. The SMR measurements are used in clinic for diagnosis and monitoring torsion and the more precise synoptophore measurements are used for fusion assessment pre-operatively. The goal of strabismus surgery is to treat torsional diplopia by regaining fusion. However, this is a retrospective study. The majority of patients no longer experienced torsional diplopia post-surgery, so unfortunately, several cases lacked synoptophore measurements post-operatively. Nevertheless, the SMR method will still give an evaluation of surgical outcome in the same subjects, hence we analyzed the SMR measurements for the operated eye pre- and post-operatively for comparison and change. The evaluated torsion only includes pp measurements. Ideally, downgaze deviation should also be evaluated, but there were too few entries post-operatively to do any statistical comparison. Retrospective reviews allow reflection and leads to further advancement of treatment plans and our assessments have become more comprehensive over time.
Moreover, our study had a small sample of subjects, and there were few patients in each dose category, which increases the likelihood of a Type II error, which decreases the power of the study. The severity of some cases increased the number of surgeries performed on an individual, and affected the response and evaluation of the dose scale. It was only possible to assess the dose effect in the unilateral cases and the bilateral cases receiving the same dose at the same time. More observations are needed to find if the scales give a linear significant effect overall.
Due to the rarity of cyclodeviation, a multicentre approach could be considered in the future to boost numbers. Patients requiring a higher surgical dose had the most severe etiology – serious head trauma. Hence, they had weaker fusional abilities and therefore required more surgery to reach the desired outcome of regaining fusion. Paresis versus paralysis mattered, as fusion was then affected by other influencing factors such as ocular motility restrictions and a combination of other ocular nerve palsies as well as SOPs. Initial overcorrection may aid in long-term success, but none of the patients remained overcorrected for any considerable length of time.
Patients in this study were treated based on clinical findings only, and other medical conditions were not considered. However, etiology may also be of interest in surgical planning.
Conclusion
A graded approach to the modified Harada-Ito procedure is considered useful as it successfully resolved torsional diplopia and relieved visual symptoms in all but two patients. The results of this retrospective study stress that several factors are involved in the final outcome, but emphasizes the role of the pre-operative individual assessments, specifically mapping cyclofusional abilities using a synoptophore.
Consultancy work
Christopher Backström and Nils-Gunnar Pehrsson from the Statistical Consulting Group (Statistika Konsultgruppen) for help with statistical analysis.
Acknowledgments
Presented in part at the 40th meeting of the European Strabismological Association (ESA) meeting, Helsinki June 6th, 2019.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Miller AM. Torsional diplopia. Am Orthopt J. 2015;65(1):21–25. doi:10.3368/aoj.65.1.21.
- Harada M, Ito Y. Surgical correction of cyclotropia. Jpn J Ophthalmol. 1964;8:88–96.
- Fells P. Management of paralytic strabismus. Br J Ophthalmol. 1974 Mar;58(3):255–265. doi:10.1136/bjo.58.3.255.
- Metz HS, Lerner H. The adjustable Harada-Ito procedure. Arch Ophthalmol. 1981 Apr;99(4):624–626. doi:10.1001/archopht.1981.03930010624006.
- Ehrt O, Boergen KP. A concept for the surgical treatment of trochlear palsy. Strabismus. 2004 Jun;12(2):75–83. doi:10.1080/09273970490515883.
- Helveston EM, Lipsky SN, Plager DA, Sprunger DT. Surgical treatment of superior oblique palsy. Trans Am Ophthalmol Soc. 1996;94(3):315–334. doi:10.1016/S0002-9394(14)70166-7.
- Mitchell PR, Parks MM. Surgery of bilateral superior oblique palsy. Ophthalmology. 1982 May;89(5):484–488. doi:10.1016/S0161-6420(82)34765-X.
- Price NC, Vickers S, Lee JP, Fells P. The diagnosis and surgical management of acquired bilateral superior oblique palsy. Eye (Lond). 1987;1(Pt 1):78–85. doi:10.1038/eye.1987.12.
- Nishimura JK, Rosenbaum AL. The long-term torsion effect of the adjustable Harada-Ito procedure. J AAPOS. 2002 Jun;6(3):141–144. doi:10.1067/mpa.2002.123429.
- Younis M, Vivian A, Lee JP. Unilateral modified Harada-lto procedure for excyclotorsion secondary to unilateral superior oblique palsy. Strabismus. 1995;3(2):85–88. doi:10.3109/09273979509063839.
- Roberts C, Dawson E, Lee J. Modified Harada-Ito procedure in bilateral superior oblique paresis. Strabismus. 2002 Sep;10(3):211–214. doi:10.1076/stra.10.3.211.8123.
- Flodin S, Karlsson P, Gronlund MA. Cyclotorsion measured in a patient population using three different methods: A comparative study. Strabismus. 2016;24(1):28–36. doi:10.3109/09273972.2015.1135967.
- Bradfield YS, Struck MC, Kushner BJ, Neely DE, Plager DA, Gangnon RE. Outcomes of Harada-Ito surgery for acquired torsional diplopia. J AAPOS. 2012 Oct;16(5):453–457. doi:10.1016/j.jaapos.2012.06.007.
- Murray C, Marsh I, Newsham D. Outcomes of the Harada-Ito Procedure. J Binocul Vis Ocul Motil. 2021;71(3):97–103. doi:10.1080/2576117X.2021.1915728.
- Flodin S, Pansell T, Rydberg A, Andersson Grönlund M. Clinical measurements of normative subjective cyclotorsion and cyclofusion in a healthy adult population. Acta Ophthalmol (Copenh). 2020;98(2):177–181. doi:10.1111/aos.14201.
- Fray KJ. Functional benefits of sensory and motor evaluation before strabismus surgery. Am Orthopt J. 2010;60(1):33–42. doi:10.3368/aoj.60.1.33.
- Archer SM. Why strabismus surgery works: the legend of the dose–response curve. J AAPOS. 2018;22(1):1.e1–1.e6. doi:10.1016/j.jaapos.2017.12.001.
- Pratt-Johnson JA, Tillson G. The investigation and management of torsion preventing fusion in bilateral superior oblique palsies. J Pediatr Ophthalmol Strabismus. 1987;24(3):145–150. May-Jun. doi:10.3928/0191-3913-19870501-11.
- Pop AE. The role of the orthoptist in the management of acquired paralytic strabismus. Am Orthopt J. 1966;16(1):73–79. doi:10.1080/0065955X.1966.11981525.
- Bata BM, Leske DA, Holmes JM. Adjustable bilateral superior oblique tendon advancement for bilateral fourth nerve palsy. Am J Ophthalmol. 2017 Jun;178:115–121. doi:10.1016/j.ajo.2017.03.028.
- Liebermann L, Leske DA, Hatt SR, Bata B, Holmes JM. Unwinding of cyclodeviation after an adjustable Harada-Ito procedure. J AAPOS. 2018;22(4):e11. doi:10.1016/j.jaapos.2018.07.032.
- Griffiths HJ, Burke JP. Temporary incyclotorsion following surgical correction of bilateral superior oblique palsy. J AAPOS. 2007 Feb;11(1):65–67. doi:10.1016/j.jaapos.2006.09.013.
- S HJ. The Mechanics of Squint Surgery, Length ‒ Tension Measurements of Human Eye Muscles, Their Implementation in a Computerized Model, and Analysis of Squint Surgery with the Model. Humanmedizin: University of Amsterdam/ University of Giessen; 1990.
- Liebermann L, Leske DA, Hatt SR, Bata BM, Holmes JM. Dose effect and stability of postoperative cyclodeviation after adjustable Harada-Ito surgery. Am J Ophthalmol. 2018 Dec;196:91–95. doi:10.1016/j.ajo.2018.08.036.