ABSTRACT
The aim of this study is to evaluate the effectiveness of an eccentric viewing training program that combines biofeedback training using micro-perimetry with home exercises on multiple visual function parameters and to explore potential relationships between post-treatment visual function parameters. A retrospective observational review of 27 participants who underwent the training program was performed. Eligible participants were diagnosed with bilateral central scotomas secondary to age-related macular degeneration. All participants undertook up to 15 visual and acoustic biofeedback training sessions and were required to partake in traditional home exercises between sessions. The biofeedback training was conducted in the better eye using the Macular Integrity Assessment microperimeter (MAIA). Distance and near acuity, contrast sensitivity and fixation stability quantified by the P1 and P2 values and the 63% and 95% bivariate contour ellipse area (BCEA) before and after the rehabilitation program were recorded. Significant improvement was noted post-training for distance visual acuity (t(26) = 4938 p = .000), near visual acuity (Z = −4.461 p = .000), contrast sensitivity (Z = −3.647 p = .000) and fixation stability for all measures, including P1 (t(26) = −9.490 p = .000), P2 (t(26) = −7.338 p = 0.000), 63% BCEA (Z = 3.569 p = .000) and 95% BCEA (t(26) = 4.687 p = .000). Significant medium-to-large correlations were also found between most visual function variables. Visual and acoustic biofeedback in conjunction with home exercises has the potential to improve visual function parameters in patients with age-related macular degeneration and irreversible central vision loss.
Introduction
Macular disorders remain one of the most prevalent causes of vision impairment across the world, with 196 million people globally impacted by age-related macular degeneration (AMD).Citation1 AMD can lead to central vision loss which impairs various visual functions including visual acuity, contrast sensitivity, color vision, depth perception and fixation stability.Citation2,Citation3 Additionally, macular dysfunction can create a significant impact on quality of life by hindering independence for activities of daily living (ADL) and impeding social inclusion.Citation4,Citation5
Whilst anti-VEGF agents have been effective in preserving the vision of those with neovascular AMD, there are many individuals who do not respond to treatment or do not maintain stable vision.Citation6 In particular, patients with geographic atrophy, a late-stage dry form of AMD, do not respond to treatment and develop bilateral central scotomas which can lead to a significant loss of vision. Despite this, it has been suggested that 90% of individuals with AMD-related vision impairment have useful residual vision which is associated with the preservation of the peripheral retina, highlighting the need for effective low-vision rehabilitation programs to maximize visual functioning and improve quality of life across various domains of daily living.Citation4,Citation7
At present, low vision intervention is dominated by the prescription of magnification devices, either optical or electronic.Citation4,Citation8 This is likely due to the fact that the most prevalent complaint of people with macular dysfunction who seek low vision services is reduced reading ability.Citation9 However, there are other rehabilitation strategies that have scope to enhance the general performance of ADLs, including eccentric viewing training (EVT). Indeed, EVT has been reported to have greater potential than magnification to maximize visual performance in those with bilateral macular loss or reduced foveal function.Citation3 Studies have reported that participants who undergo a structured EVT program not only show an improvement in their acuity and reading ability but also in contrast sensitivity and fixation stability.Citation3,Citation10,Citation11
The foundation of EVT is to optimize visual capability by utilizing an alternative retinal focal point with better retinal sensitivity to that of the affected macula. There are multiple methods used to train eccentric viewing; however, all involve a re-fixation movement to a preferred retinal locus (PRL) or a trained retinal locus (TRL). A PRL is determined intuitively, whereby the patient attempts to improve their vision by fixing with a peripheral retinal area to compensate for the loss of central fixation, whilst a TRL is an area of the retina specifically identified and selected by a low vision specialist to optimize vision and function. The use of a TRL is favored, as when eccentric viewing is intuitive, it can result in one or multiple eccentric points being utilized for viewing.Citation12–14 Additionally, it is estimated that a PRL can result in approximately 25% of cases using an unfavorable, ineffective retinal area.Citation2
In recent years, motor neurorehabilitation by means of biofeedback technology has gained popularity as a method of EVT.Citation2,Citation10,Citation15 This treatment incorporates microperimetry and a combination of visual and auditory feedback to reinforce the TRL and improve fixation stability. When there is damage to the macular region, fixation stability degrades, which further compounds the vision loss. As such, improving fixation stability can play a vital role in the success of optimizing visual function.Citation11,Citation15–17
To date, several papers have shown that biofeedback training in AMD can lead to improvements in visual acuity,Citation15,Citation18–25 fixation stability,Citation16,Citation18,Citation20–23,Citation26,Citation27 and reading.Citation18,Citation20,Citation23 However, there is limited research that has investigated the real-world effectiveness of biofeedback training combined with traditional home exercises or that has explored the effectiveness of this treatment across multiple visual function parameters. The aim of this retrospective study was to investigate the effectiveness of an EVT program delivered in a real-world setting that combines a traditional EVT technique with biofeedback training using microperimetry. The study also aimed to investigate potential relationships between visual function parameters post-training.
Methodology
Study design
This study was a retrospective observational review. Written consent was obtained from all patients and the study adhered to the tenets of the Declaration of Helsinki and was approved by La Trobe University, Human Research Ethics Committee.
Participants
Patients over the age of 18 with bilateral central vision loss secondary to geographic macular atrophy were included in the study. The diagnosis of bilateral geographic macular atrophy was provided by the referring eye care professional and confirmed on fundus imaging at presentation. All patients had undergone combined visual and acoustic biofeedback training using Macular Integrity Assessment (MAIA) microperimetry, in conjunction with traditional eccentric viewing training at a private orthoptic vision rehabilitation practice in Melbourne, Australia.
Patients were excluded from the study if they had previously undergone any formal EVT, had media opacities, were diagnosed with a unilateral central scotoma, had residual foveal function in either eye or if they were unable to comprehend instructions or provide informed consent.
All participants underwent an identical process for establishing eligibility for treatment and enrollment in the rehabilitation program.
Macular integrity assessment (MAIA)
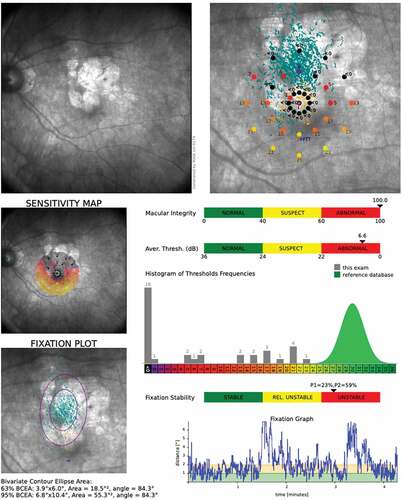
The MAIA microperimetric technology (MAIA, Centervue, Padova, Italy) incorporates analysis of retinal morphology, alongside a retinal function assessment using Scanning Laser Ophthalmoscope (SLO) and can be used for biofeedback training. During a standard automated perimetry (SAP) assessment, the microperimeter concurrently incorporates fundus imaging, macular sensitivity topography and fixation analysis.Citation10,Citation15 The SAP provides an analysis of retinal sensitivity measured in decibel (dB) within a 10° diameter area and with 37 measurement points using a white LED light stimulus of varying intensity. This light is projected directly on the retinal surface at each loci and incorporates a Goldmann III stimulus size with a background luminance of 4 apostilbs (asb) and a 36 decibel (dB) dynamic range.Citation28 illustrates MAIA microperimetry results report of a patient with AMD.
Figure 1. Microperimetry results report of an initial MAIA assessment. The top-left image shows SLO of the fundus, and the top-right image shows combined SLO with SAP. The retinal sensitivity is color co-ordinated and measured in dB and the TRL is identified in blue as the Fixation Training Target (FTT). The bottom-left image identifies the 63% BCEA shown as the smaller purple ring and the larger purple ring represents 95% BCEA. Fixation stability P1 and P2 values are identified in along a normative colored scale.
Trained retinal locus (TRL)
Once the participant met the inclusion criteria for treatment, the eye with the better fixation stability success rate was chosen to be trained. The macular integrity assessment was used to identify the TRL of the chosen eye and was planned to become a new fixation location for the patient. The TRL was chosen by considering four fundamental factors: (i) the retinal sensitivity value of the retinal locus and surrounding area, (ii) the morphology of the scotoma and its extension to or from the chosen locus, (iii) the proximity of the TRL to the fovea and the individual’s PRL location and (iv) the bivariate contour ellipse area (BCEA) angle. The BCEA is a statistically calculated ellipse area that shows the fixation pattern and extent of the fixation points.Citation29 The BCEA angle was important to consider as it provided an indication for the preferred direction for refixation. Overall, a TRL with high retinal sensitivity and close proximity to the fovea was considered optimal, as was a scotoma extending away from the chosen locus, and a locus that was neighboring the PRL or along the BCEA angle. If there were two or more TRL options available, a superior or inferior point was chosen to optimize vision for ADLs such as readingCitation10,Citation30–34
Rehabilitation program
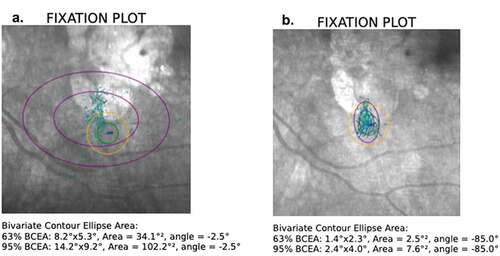
The rehabilitation program consisted of up to 15 biofeedback training sessions, in addition to home exercises. The biofeedback training was conducted in a darkened room using the MAIA and included 3-minute intervals that extended for a total of 9 minutes as described by Frennesson and Nilsson.Citation32 There was a brief pause in between intervals to allow the patient to rest. The interval approach was preferred as the patients started to tire toward the third minute, as observed on the MAIA fixation graph. During the biofeedback session, the patients were provided with verbal instructions to move their eyes to locate the TRL. Simultaneously, the patients were listening to audio feedback (interval beeps) which prompted them as to whether their fixation was closer (shorter interval beeps) or further away (longer interval beeps) from the allocated TRL. Once the patient’s eye was positioned to stimulate the TRL, a stationary light would turn on and the audio stimulus became constant. The patient was then instructed to steady their eye at this fixation point to keep the light on and audio constant. Patient’s progression was monitored using the MAIA fixation measures including P1 and P2, the 95% BCEA value and the fixation graph ().
Figure 2. Progression of fixation training. The patient’s fixation parameters are identified as P1 (green circle), P2 (yellow circle), 63% BCEA (smaller purple circle) and 95% BCEA (larger purple circle). Image a represents fixation at the start of training and image b demonstrates the fixation progress toward the end of the training. Also note the TRL location is highly reproducible throughout the training.
Following the biofeedback session, the participants undertook home exercises which included a reading task using their habitual reading glasses and other related tasks. Patients were instructed to read aloud without skipping words. The reading material contained high-frequency and non-technical words and the sentence structure included correct grammar and punctuation. The font size chosen was based on the patient’s ability to read single words or a sentence expressed in electronic point. The selection was also based on the patient's ability to read most of the words presented, with the number of errors and reading speed considered. The size of print was adapted to a smaller size when the patient was able to read the training material with accuracy and fluency. Threshold was reached when the patient was unable to improve their reading accuracy or fluency at the allocated print size. Trainees were given reading material for homework to be completed daily along with individualized tasks (such as watching TV or recognizing faces during a social event) to enable them to practice their technique in their natural environment.
Outcome measures
The patient’s visual function was measured at baseline, at the conclusion of the program and one-month post-treatment. The baseline measures were assessed with the patient’s PRL as the TRL was yet to be determined. The TRL was employed to assess the outcomes measures at the conclusion of treatment and one-month post-treatment. Visual function included best corrected visual acuity (VA) with both eyes open (distance and near), contrast sensitivity and fixation stability. Patients wore their most recent habitual prescription to assess acuity and contrast. Distance visual acuity was assessed with the Early Treatment Diabetic Retinopathy Study (ETDRS) chart, and the logMAR unit of measure was used to document the outcome. Near visual acuity was assessed using the Near Logarithm of the Minimum Angle of Resolution (LogMAR) chart, and the N-point notation was used to report near visual acuity. Contrast sensitivity was assessed by the Low Contrast Flip Chart 10 M Optotypes with Lea Symbols, and the number of symbols seen was recorded. Up to 5 symbols represented 25% contrast, 10 indicated 10% contrast, 15 was 5% contrast, 20 was 2.5% contrast and up to 25 symbols indicated 1.25% contrast.
The MAIA fixation stability success rate (P1 and P2) and the BCEA for 63% and 95% were used to evaluate fixation stability. The P1 and P2 circle indexes represent the percentage of fixation points located within the 2° and 4° of diameter, respectively, whilst the BCEA margins describe the statistical distribution of 63% and 95% of all fixation points from the TRL, respectively.
Statistical analysis
Data extracted from the medical histories was transferred into SPSS version 27 (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.) for statistical analysis. A paired sample t-test was used to analyze the difference between pre- and post-scores for distance visual acuity, P1 value, P2 value and 95% BCEA value. For data that were not normally distributed (Near visual acuity, contrast sensitivity and 63% BCEA value) the Wilcoxon Signed Rank Test was used.
Pearson’s r or Spearman’s rho 9 (ρ) was used for correlation between two variables, not controlling for any other factors. Strength of relationship for correlations was interpreted as 0 (no strength) to 1 (large) with a small relationship equating to 0.1–0.29; medium 0.3–0.49 and large = 0.5–1.Citation35
Results
Participants
Twenty-seven participants with a mean age of 79.7 ± SD 12.2 (range 45–95) were included in the study. Seventeen (63%) were females and 10 males.
Rehabilitation
Participants received an average of 6.85 (SD 3.11) in clinic biofeedback sessions ranging from 3 to 15 sessions. The mean dB trained was 20.44 (SD 4.492) with a range between 13 and 8 db. The eye with the better fixation stability was chosen, 16 (59.3%) of the participants had the right eye selected for training and 11 (40.7%) the left eye.
Distance visual acuity
Distance VA improved from 0.80 logMAR (6/38) pre-training to 0.59 logMAR (6/19–6/24) post-training t(26) = 4.94, p = .000 with a mean improvement of 0.23 logMAR which equates to approximately 10 letters or 2 lines of improvement (). The eta squared statistic of 0.47 indicated a large effect size.
Table 1. Mean, SD and statistical outcome of visual function parameters.
Near visual acuity
Near vision improved from a mean of N29.15 to N10.44 (0.95 to 0.52 logMAR) post-training and this was statistically significant, z = −4.46, p = .00, with a large effect size of 0.8 ().
Contrast sensitivity
Contrast sensitivity showed a statistically significant improvement after training from 16.89 (2.5% contrast) to 20.85 (1.25% contrast) z = −3.65, p = .00 with a large effect size of 0.7 ().
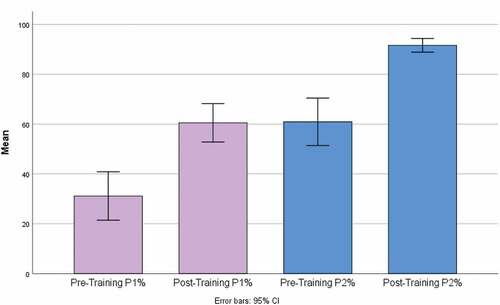
Fixation stability: success rate
The P1 value improved from 31.15 to 60.52 with a mean improvement of 29.37 post-training t(26) = −9.5, p = .00. The eta squared statistic of 0.77 indicated a large effect size. The P2 value improved from 60.93 to 91.63 post-training with a mean improvement of 30.7, t(26) = −7.34, p = .00 (two tailed). The eta squared statistic of 0.67 indicated a large effect size ( and ).
A large correlation was noted between P1 and distance visual acuity (ρ = −0.56, p = .002) and contrast sensitivity (ρ = 0.70, p = .000) and a medium correlation with near visual acuity (ρ = −0.39, p = .046). A large correlation was found between P2 and distance visual acuity ρ = −0.57, p = .002 and contrast sensitivity (ρ = 0.62, p = .001).
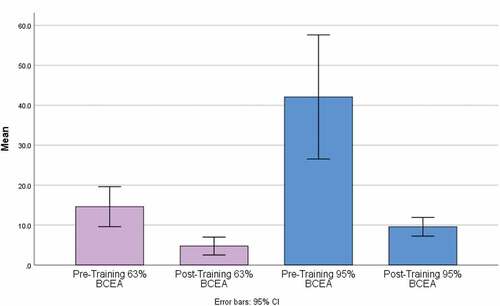
Fixation stability: bivariate contour ellipse area (BCEA)
The 63% BCEA value improved from 14.60 pre-training to 4.73 post training, with a mean improvement of 9.87 which was statistically significant (z = −3.57, p = .00) with a large effect size of 0.7. The 95% BCEA value improved from 42.08 pre-training to 9.58 post training, with a mean improvement of 32.51, t(26) = 4.69, p = .00 (two tailed). The eta squared statistic of 0.46 indicated a large effect size ( and ).
A large correlation was noted between 95% BCEA and distance visual acuity (ρ = 0.50, p = .008) and contrast sensitivity (ρ= −0.54, p = .004) and a medium correlation with near visual acuity (ρ = 0.40, p = .041). No correlations were noted between 63% BCEA and other visual function parameters ().
Table 2. Correlations between visual function parameters.
Discussion
There is a paucity of research investigating the real-world effectiveness of combined biofeedback eccentric viewing training and home exercises.Citation36 The current study provides evidence that the use of visual and acoustic biofeedback, combined with structured home exercises, is effective in improving distance and near acuity, contrast sensitivity and fixation stability parameters in patients with irreversible bilateral central field loss. The study also found medium-to-large correlations between near and distance acuity and contrast sensitivity with most fixation stability measures. It is postulated that the use of the biofeedback technique allows for an accurate refixation to the TRL with improved oculomotor stability during eccentric fixation, whilst the home exercises reinforce the application of eccentric fixation for activities of daily living.
The utility of microperimetry for visual rehabilitation, and particularly with the use of the MP-1 microperimeter and MAIA,Citation2,Citation10,Citation15,Citation16,Citation18–21 has been widely documented. The results of our work are comparable with other studies that have employed biofeedback; however, the outcomes reported in the current study showed a greater effect of the training as compared with most biofeedback EVT studies.Citation15,Citation18,Citation20 This could be attributed to utilizing a TRL location, instead of the patient’s PRL, the differences in the method of biofeedback training and/or the use of structured home-exercises to compliment the biofeedback training program.
Researchers have identified that the location of the eccentric fixation locus and fixation stability are the essential keystones to the effectiveness of EVT.Citation16,Citation25 In this study, a TRL was chosen as compared with other studies that have utilized the patients’ naturally occurring PRL.Citation25 The rationale for selecting a TRL was founded on the emerging consensus showing that an individual’s self-selected PRL does not always produce optimum visual outcomes.Citation2,Citation9,Citation10,Citation16,Citation25 For instance, a comparative study by Morales and colleaguesCitation16 investigating the effectiveness of biofeedback EVT showed better visual function outcomes in participants trained using a selectively chosen TRL compared to participants utilizing a PRL. The selection criteria for choosing a TRL in our study were also consistent with evidence provided by previous research.Citation9,Citation10,Citation16,Citation25 The criteria included identifying a locus with the highest sensitivity closest in proximity to the estimated fovea, whilst considering the scotoma morphology extension away from the TRL and an area surrounded by the largest span. It is noteworthy, however, that while there is general consensus regarding the selection of the TRL, the underlying reasons for the optimal eccentric location are not clearly understood,Citation16,Citation25,Citation37 and little consideration has been given to the BCEA when choosing a location. In our study, the angle of the BCEA was considered when selecting the location of the TRL. This appears to be a novel approach as other studies have not reported the use of the BCEA angle in their selection criterion. The BCEA angle was considered as it may enable a more intuitive saccadic refixation movement to the TRL during training. A paper by Whittaker, Cummings and SwiezonCitation36 reported that saccadic velocity and frequency deteriorate in eccentric fixation. Therefore, selecting a TRL along the BCEA axis could potentially support the participant locating and subsequently adapting to the TRL more efficiently. Our study, however, did not specifically look at the effect of the BCEA angle on visual function. Further research is warranted to evaluate whether the authors’ assumptions regarding the BCEA angle hold merit and to investigate whether a TRL within the axis of the BCEA should be prioritized as part of the TRL selection criterion.
Whilst a significant differentiating feature of our study was the conjugate use of structured home training exercises, the biofeedback program itself was relatively consistent with previous research using microperimetry rehabilitation alone.Citation16,Citation18,Citation19 Most biofeedback studies have utilized biofeedback sessions of 9–10 minutes,Citation15,Citation16,Citation18,Citation21 although we included an interval approach with breaks every 3 minutes, similar to one other study.Citation21 Additionally, it is worth noting that within the literature there is variability in the frequency of training, the type of stimulus used and the eye trained. Some researchers have offered daily sessions, whilst others conducted 1–4 sessions per week,Citation24,Citation25 some have used a visual stimulus alone, whilst others have used both auditory and visual stimuli,Citation15,Citation23,Citation24,Citation38,Citation39 and some have used monocular training of the eye with better vision, whilst others have trained both eyes.Citation19,Citation24,Citation25,Citation40 These inconsistencies could potentially contribute to the differences noted in the outcomes of our study compared to others.
Overall, although our biofeedback program was consistent with the literature, the optimum program for EVT is yet to be determined. Whilst 10–12 sessions, with no interval breaks, are frequently employed for training, it is unclear if this is the most effective approach. This is of particular interest given that in real-world settings patients are often unable to attend all scheduled appointments and easily fatigue during training. Whilst in our study we aimed to implement weekly training involving a 10–12 session program per patient, the mean number of sessions engaged was 6.85 (range 3–15). Some patients chose to cease their training program due to various factors, including general health illness, reliance and cost of transport to the clinic or they could no longer see the benefit of training and felt they could continue without assistance. Further research is warranted to establish the optimal training structure and the minimum sessions required to achieve a successful outcome for patients. Clinical guidelines regarding this will enable clearer parameters for clinicians and has the potential to improve patient engagement and compliance.
In addition to establishing clinical guidelines for biofeedback training, the effectiveness of complimentary structured home exercises on clinical outcomes requires further investigation. To date, only one other study by Limoli and colleaguesCitation34 has used a combined treatment approach. This study used Augmented Reality Eyewear (ARE) to perform home-based eccentric viewing exercises following biofeedback training using the MAIA. The home exercise involved a reading task whereby participants were asked to read 5-letter words projected against the ARE monitor seen in the eyewear. Findings suggested improved fixation stability in those that completed the home exercise as compared to those that only underwent biofeedback EVT. Although we did not use a control group in our study to objectively evaluate the effectiveness of the home-based exercises, we similarly found improved fixation stability using a combined treatment program. The home-based structured reading exercises in our study, using decreasing font sizes along with tailored activities of daily living exercises (such as watching TV, recognizing faces and eating meals), enabled the application of eccentric viewing in real-world scenarios outside of the in-clinic training. Given that our study did not include a control group, it is unknown whether the improvements found in the visual function parameters were influenced by this program. However, the improvements were greater than those reported by other biofeedback EVT studies.Citation15,Citation18,Citation20 Additionally, we found that many of the fixation stability parameters of the MAIA (P1, P2 and 95% BCEA) correlated with visual acuity and contrast sensitivity. This suggests that combined EVT programs could potentially have a significant, positive impact on activities of daily living and could even potentially reduce the need for low vision devices. Further research is needed to investigate the effect of EVT programs on activities of daily living and to explore the influence of combined treatment methods.
Conclusion
Biofeedback EVT has modernized low vision rehabilitation to provide more targeted methods to improve visual function in those with bilateral macular dysfunction. This retrospective study reflects the nuances of the clinical application of biofeedback eccentric viewing training. Despite the limitations of the real-world clinical implementation of the program, this study showed that visual and acoustic biofeedback eccentric viewing training in conjunction with home exercises can be effective in improving visual function parameters in patients with age-related macular degeneration and irreversible central vision loss. Further research is necessary to explore the optimal parameters of EVT programs and the development of clinical guidelines that will enhance patient outcomes.
Acknowledgment
The authors would like to thank Vision Matters (low-vision practice) and the participants.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–16. doi:10.1016/S2214-109X(13)70145-1.
- Markowitz SN, Reyes SV. Microperimetry and clinical practice: an evidence-based review. Can J Ophthalmol. 2013;48(5):350–357. doi:10.1016/j.jcjo.2012.03.004.
- Vukicevic M, Fitzmaurice K. Eccentric viewing training in the home environment: can it improve the performance of activities of daily living? J Visual Impairment Blindness. 2009;103(5):277–290. doi:10.1177/0145482X0910300506.
- Lamoureux EL, Pallant JF, Pesudovs K, Rees G, Hassell JB, Keeffe JE. The effectiveness of low-vision rehabilitation on participation in daily living and quality of life. Invest Ophthalmol Vis Sci. 2007;48(4):1476–1482. doi:10.1167/iovs.06-0610.
- Hassell JB, Lamoureux EL, Keeffe JE. Impact of age related macular degeneration on quality of life. Br J Ophthalmol. 2006;90(5):593–596. doi:10.1136/bjo.2005.086595.
- Fleckenstein M, Keenan TDL, Guymer RH, et al. Age-related macular degeneration. Nat Rev Dis Primers. 2021;7(1):31. doi:10.1038/s41572-021-00265-2.
- Hinds A, Sinclair A, Park J, et al. Impact of an interdisciplinary low vision service on the quality of life of low vision patients. Br J Ophthalmol. 2003;87(11):1391–1396. doi:10.1136/bjo.87.11.1391.
- Chung STL. Reading in the presence of macular disease: a mini-review. Ophthalmic Physiol Opt. 2020;40(2):171–186. doi:10.1111/opo.12664.
- Markowitz M, Daibert-Nido M, Markowitz SN. Rehabilitation of reading skills in patients with age-related macular degeneration. Can J Ophthalmol. 2018;53(1):3–8. doi:10.1016/j.jcjo.2017.10.042.
- Vingolo EM, Napolitano G, Fragiotta S. Microperimetric biofeedback training: fundamentals, strategies and perspectives. Front Biosci (Schol Ed). 2018;10:48–64. doi:10.2741/s500.
- Falkenberg HK, Rubin GS, Bex PJ. Acuity, crowding, reading and fixation stability. Vision Res. 2007;47(1):126–135. doi:10.1016/j.visres.2006.09.014.
- Vukicevic M, Fitzmaurice K. Impact of eccentric viewing and magnification interventions on the performance of activities of daily living. Int Congr Ser. 2005;1282:544–548. doi:10.1016/j.ics.2005.04.024.
- Crossland MD, Engel SA, Legge GE. The preferred retinal locus in macular disease: toward a consensus definition. Retina. 2011;31(10):2109–2114. doi:10.1097/IAE.0b013e31820d3fba.
- Goodrich GL, Mehr EB. Eccentric viewing training and low vision aids: current practice and implications of peripheral retinal research. Am J Optom Physiol Opt. 1986;63(2):119–126. doi:10.1097/00006324-198602000-00007.
- Vingolo EM, Salvatore S, Cavarretta S. Low-vision rehabilitation by means of MP-1 biofeedback examination in patients with different macular diseases: a pilot study. Appl Psychophysiol Biofeedback. 2009;34(2):127–133. doi:10.1007/s10484-009-9083-4.
- Morales MU, Saker S, Wilde C, Rubinstein M, Limoli P, Amoaku WM. Biofeedback fixation training method for improving eccentric vision in patients with loss of foveal function secondary to different maculopathies. Int Ophthalmol. 2020;40(2):305–312. doi:10.1007/s10792-019-01180-y.
- Mandelcorn MS, Podbielski DW, Mandelcorn ED. Fixation stability as a goal in the treatment of macular disease. Can J Ophthalmol. 2013;48(5):364–367. doi:10.1016/j.jcjo.2013.05.006.
- Ramírez Estudillo JA, León Higuera MI, Rojas Juárez S, Ordaz Vera MDL, Pablo Santana Y, Celis Suazo B. Visual rehabilitation via microperimetry in patients with geographic atrophy: a pilot study. Int J Retina Vitreous. 2017;3(1):21. doi:10.1186/s40942-017-0071-1.
- Daibert-Nido M, Patino B, Markowitz M, Markowitz SN. Rehabilitation with biofeedback training in age-related macular degeneration for improving distance vision. Can J Ophthalmol. 2019;54(3):328–334. doi:10.1016/j.jcjo.2018.10.016.
- Nido MD, Markowitz SN. Vision rehabilitation with biofeedback training. Can J Ophthalmol. 2018;53(3):e83–4. doi:10.1016/j.jcjo.2017.11.003.
- Pacella E, Pacella F, Mazzeo F, et al. Effectiveness of vision rehabilitation treatment through MP-1 microperimeter in patients with visual loss due to macular disease. Clin Ter. 2012;163(6):e423–8.
- Ratra D, Gopalakrishnan S, Dalan D, Ratra V, Damkondwar D, Laxmi G. Visual rehabilitation using microperimetric acoustic biofeedback training in individuals with central scotoma. Clin Exp Optom. 2019;102(2):172–179. doi:10.1111/cxo.12834.
- Vingolo EM, Cavarretta S, Domanico D, Parisi F, Malagola R. Microperimetric biofeedback in AMD patients. Appl Psychophysiol Biofeedback. 2007;32(3–4):185–189. doi:10.1007/s10484-007-9038-6.
- Gaffney AJ, Margrain TH, Bunce CV, Binns AM. How effective is eccentric viewing training? A systematic literature review. Ophthalmic Physiol Opt. 2014;34(4):427–437. doi:10.1111/opo.12132.
- Silvestri V, Turco S, Piscopo P, et al. Biofeedback stimulation in the visually impaired: a systematic review of literature. Ophthalmic Physiol Opt. 2021;41(2):342–364. doi:10.1111/opo.12787.
- Amore FM, Paliotta S, Silvestri V, Piscopo P, Turco S, Reibaldi A. Biofeedback stimulation in patients with age-related macular degeneration: comparison between 2 different methods. Can J Ophthalmol. 2013;48(5):431–437. doi:10.1016/j.jcjo.2013.07.013.
- Tarita-Nistor L, González EG, Markowitz SN, Steinbach MJ. Plasticity of fixation in patients with central vision loss. Vis Neurosci. 2009;26(5–6):487–494. doi:10.1017/S0952523809990265.
- Centervue. MAIA: Microperimetry Handbook. Padova: Italy Centervue; n.d.
- Molina-Martín A, Piñero DP, Pérez-Cambrodí RJ. Normal values for microperimetry with the MAIA microperimeter: sensitivity and fixation analysis in healthy adults and children. Eur J Ophthalmol. 2017;27(5):607–613. doi:10.5301/ejo.5000930.
- Riss-Jayle M, Giorgi R, Barthes A. Setting the preferential retinal locus. Part 1. Analysis of the rehabilitation results as a function of positioning. J Fr Ophtalmol. 2008;31(3):249–255. doi:10.1016/S0181-5512(08)74801-0.
- Riss-Jayle M, Giorgi R, Barthes A. Setting the preferential retinal locus. Part 2. When, where, and how does it become established? J Fr Ophtalmol. 2008;31(4):379–385. doi:10.1016/S0181-5512(08)71432-3.
- Frennesson C, Nilsson SE. The superior retina performs better than the inferior retina when reading with eccentric viewing: a comparison in normal volunteers. Acta Ophthalmol Scand. 2007;85(8):868–870. doi:10.1111/j.1600-0420.2007.00984.x.
- Palmer S, Logan D, Nabili S, Dutton GN. Effective rehabilitation of reading by training in the technique of eccentric viewing: evaluation of a 4-year programme of service delivery. Br J Ophthalmol. 2010;94(4):494–497. doi:10.1136/bjo.2008.152231.
- Limoli P, Morales M, Costanzo P, et al. Augmented Reality Eyewear (ARE) for home-based vision training after biofeedback rehabilitation of eccentric viewing. Optometry Visual Perform. 2017;5(1):15–20.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale (NJ): Erlbaum; 1988.
- Morales MU, Limoli PG, Limoli C. Augmented reality eyewear for home-based vision training after biofeedback rehabilitation of eccentric fixation. Invest Ophthalmol Visual Sci. 2015;56:548–.
- Lombardo M, Serrao S, Ducoli P, Lombardo G. Eccentricity dependent changes of density, spacing and packing arrangement of parafoveal cones. Ophthalmic Physiol Opt. 2013;33(4):516–526. doi:10.1111/opo.12053.
- Verdina T, Giacomelli G, Sodi A, et al. Biofeedback rehabilitation of eccentric fixation in patients with Stargardt disease. Eur J Ophthalmol. 2013;23(5):723–731. doi:10.5301/ejo.5000291.
- Vingolo EM, Salvatore S, Limoli PG. MP-1 biofeedback: luminous pattern stimulus versus acoustic biofeedback in age related macular degeneration (AMD). Appl Psychophysiol Biofeedback. 2013;38(1):11–16. doi:10.1007/s10484-012-9203-4.
- Vingolo EM, Salvatore S, Domanico D, Spadea L, Nebbioso M. Visual rehabilitation in patients with myopic maculopathy: our experience. Can J Ophthalmol. 2013;48(5):438–442. doi:10.1016/j.jcjo.2013.08.004.