ABSTRACT
Background
The aim of this systematic review is to identify cases of neurogenic ocular palsy in the presence of COVID-19 and to document patient characteristics, type of palsy and possible aetiologies.
Methods
A systematic search of PubMed, Medline and CINAHL databases was conducted on the 6th of January 2023 to identify cases of neurogenic ocular palsy in patients with current or previous COVID-19 infection. Data were pooled to summarise the neurogenic palsy, patient clinical characteristics and proposed palsy mechanisms.
Results
The combined database search yielded 1197 articles. Of these, 23 publications consisting of 25 patients met the inclusion criteria. Most patients were male (68%) and ranged in age from 2 to 71 years (median=32.7, SD=21.4). Seven patients (28%) were children aged 2 to 10 years old. Abducens palsies were most common (68%) and the most common ocular presentation was diplopia (76%) with an average time of onset 15 days from testing positive to COVID-19 or having symptoms of the virus. Proposed mechanism of development of a neurogenic palsy secondary to COVID-19 infection was classified into one of three categories: vascular/thrombotic, a viral neuro-invasive or inflammatory virus-mediated immune response.
Discussion
This study suggests that COVID-19 infection may be linked to oculomotor, trochlear and abducens nerve palsies and the underlying mechanisms may vary but are difficult to definitively establish. Further studies investigating the onset of neurogenic palsy secondary to COVID-19 infection is required.
Introduction
The coronavirus disease 2019 (COVID-19) resulting from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a respiratory virus that was declared a pandemic in March 2020.Citation1 It most commonly presents with symptoms of fever, dry cough and shortness of breath and can be detected by a Rapid Antigen Test (RAT) or Reverse Transcription Polymerase Chain Reaction (RT-PCR) test.Citation2 Whilst the respiratory manifestations of COVID-19 are commonly studied, less is known about the ocular presentation of the virus. Conjunctivitis, dry eyes, foreign body sensation, redness, itching and epiphora seem to be the most common associated symptoms.Citation3,Citation4 The down-regulation of angiotensin-converting enzyme (ACE-2) receptors, which are proteins found on the surface of several cells in the body, is implicated in both ocular manifestations and multiple-organ injury secondary to the virus.Citation5 There is a reported link between COVID-19 and peripheral nervous system complications such as neuroinflammation, vasodilation and thrombotic events; however, the underlying pathophysiology is not well established but may be caused by the neurotrophic and neuroinvasive nature of the coronavirus.Citation3,Citation6
Given the nervous system complications that can occur due to COVID-19, there have also been reports of sudden-onset-acquired ocular neurogenic palsies as a result of the virus.Citation7–10 Acquired neurogenic palsies result in weakened ocular muscle strength and limitation of ocular movement and, of the three cranial nerve (CN) types involved with eye movement (oculomotor, trochlear and abducens), abducens nerve palsies have been reported as the most common.Citation8 Patients generally present with an initial complaint of sudden-onset diplopia and this symptom typically resolves within 1 to 3 months, with full recovery.Citation8
The underlying cause of an ocular neurogenic palsy secondary to COVID-19 is uncertain; however, based on the literature, there appear to be three broad causes: 1) a vascular/thrombotic, 2) neuro-invasive or 3) inflammatory immune response.Citation7,Citation9,Citation11,Citation12 The vascular/thrombotic cause is linked to immune modulated thrombosis caused directly by the COVID-19 virus. The virus suppresses ACE-2 receptors that would normally act as an anti-coagulant. Dysfunctional microvasculature occurs due to the coagulated blood and this in turn causes the neurogenic palsy.Citation7,Citation13,Citation14 The ACE-2 receptors are also implicated in the neuro-invasive cause. It is thought that the COVID-19 virus can enter the brain via these receptors (or directly via the olfactory bulb) and bind to neurons, thereby inducing the CN palsy.Citation9,Citation15 It is also possible that COVID-19 can cause dysfunctional nerve conduction via an excessive immune response post-infection. The dysregulated immune response leads to inflammation and an increase in cytokine levels. Cytokines, the small proteins involved in immune response signaling, create a “cytokine storm” and high levels of these proteins cause neurodegeneration and de-myelination leading to the nerve palsy.Citation3,Citation9,Citation16
The aim of this systematic review was to identify cases of neurogenic palsy in the presence of COVID-19 and to document the patient characteristics, type of palsy and possible etiologies. Recognizing any links between COVID-19 and neurogenic palsies will facilitate more efficient diagnosis and add to the body of literature in this emerging area.
Methods
Search strategy
A systematic search of three electronic databases (PubMed, Medline (1946-) on Ovid, and CINAHL) was conducted on 6 January 2023. Search results were limited to human subjects and those published in English. The search terms included SARS-CoV-2, COVID-19, coronavirus, palsy, diplopia, neurogenic, third nerve, oculomotor nerve, fourth nerve, trochlear nerve, sixth nerve and abducens nerve with Boolean operators used.
Eligibility criteria
Case reports and case series of patients, irrespective of age, positive for SARS-CoV-2 or COVID-19 with a diagnosis of ocular neurogenic palsy within 28 days of infection were included. The time to onset of the palsy of 28 days was set by the authors based on the findings of a systematic review of all ocular manifestations of COVID-19.Citation4 This period of time also limits other systemic complications as the cause of the palsy.
Case reports or case series had to contain prior medical history and indicate whether there were preexisting comorbidities. Reports of patients with comorbidities including a history of stroke, diabetes mellitus, cancer and dementia were excluded.
Study selection
Endnote X9 (Clarivate, Philadelphia PA, USA) was used to import the search results and duplicates were automatically removed. The titles and abstracts of the articles were independently screened by two authors (RS and SB). Articles not meeting the inclusion criteria were removed, and the full text of the remaining articles were obtained and reviewed in full by authors RS and SB.
Data extraction, critical appraisal and data synthesis
All articles included in this study were independently appraised by authors RS and SB using the Joanna Briggs Institute (JBI) checklist for case reportsCitation17 or case series.Citation17 The JBI appraisal tool was modified to provide a numerical score for quality where a “yes” received 2 points, “unclear” received 1 point and “no” received 0 points with a maximum of 16 points for case reports and 20 points for case series.Citation18 Articles were graded by author MV using this method. Data were extracted using a self-designed data extraction table. Data collected included patient age and sex; whether they were symptomatic to COVID-19; neurogenic palsy classification; ocular symptoms; time to development of ocular symptoms and time to improvement or resolution of symptoms; treatment and possible palsy mechanism.
Due to inconsistent and heterogeneous patient results it was not possible to conduct a meta-analysis. Therefore, data were synthesized in a narrative summary.
Results
Search results
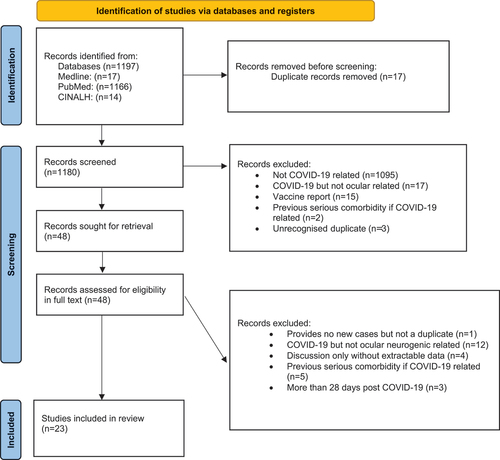
A combined search of the three electronic databases yielded 1197 articles and 17 were recognized as duplicates and removed through the Endnote X9 software. Using the title and abstract, 1180 articles were independently screened by two authors (RS and SB). The selection process is documented in a PRiSMA flow diagram (). Both authors read the full text of the remaining 48 articles. Twenty-three published reportsCitation7,Citation9–12,Citation19–36 met the inclusion criteria, and all patients presented with COVID-19 infection and a neurogenic palsy.
Study quality
The JBI tool for case reports was used for 20 publications, and the tool for case series was used for three publications. None were excluded through the critical appraisal process. Reduction in points for quality was due to lack of information required for data extraction ().
Table 1. Summary of patient characteristics and critical appraisal score (* denotes a case series and ^ denotes a case study).
Patient demographics
The data of 25 patients were available from the 23 reports included in this systematic review (). There were 17 males (68%) and 8 females (32%) with an age range of 2–71 years (mean = 32, SD = 21.4, median = 32.7). Seven patients (28%) in this study were children aged 2–10 years old. All patients had a history of COVID-19 infection of which 16 (64%) were symptomatic. Seven patients (28%) were from the United States of America, 4 (16%) were from Brazil, 3 (12%) were from France, 2 (8%) from Turkey and the remaining patients were each from French Guiana, Greece, Israel, Japan, Morocco and the United Kingdom ().
Clinical presentation
Seventeen patients (68%) presented with a right abducens nerve palsy (CN VI), seven (28%) with an oculomotor palsy (CN III) and one (4%) with a trochlear nerve palsy (CN IV). All patients, except one, had a palsy isolated to a single cranial nerve. The most common ocular presentation was diplopia (n = 16, 64%), diplopia with blurred vision (n = 2, 8%) or diplopia with eyelid pain (n = 1, 4%). The time from onset of COVID-19 symptoms or a positive test and ocular symptoms ranged from 2 days to 21 days (mean = 14.9, SD = 4.2) and the time to improvement or resolution of ocular symptoms ranged from 2 days to 240 days (mean = 41.1, SD = 59.7).
Proposed mechanism
The proposed causal mechanisms of the neurogenic palsies extracted from the reports were broadly classified as vascular/thrombotic, viral neuro-invasion or an inflammatory virus-mediated immune response. The most postulated mechanism was inflammatory virus-mediated immune response (n = 10, 40%) and of these, 3 (12%) were children diagnosed with pediatric multi-system inflammatory syndrome. Viral neuro-invasion was proposed as a mechanism for six patients (24%) and a vascular/thrombotic cause was suggested for three patients (12%). The most frequent causal mechanism for patients with an abducens palsy was an inflammatory virus-mediated response (n = 9) whilst those with an oculomotor palsy either had a vascular/thrombotic (n = 2) or viral neuro-invasive (n = 2) mechanism reported ().
Discussion
COVID-19 respiratory manifestations are now well known, as are some of the common ocular presentations, namely conjunctivitis, dry eyes, foreign body sensation, redness, itching and epiphora.Citation3,Citation4 The findings of this systematic review suggest that, although uncommon, COVID-19 is associated with sudden-onset neurogenic palsy.
Based on the findings of this review, patients with ocular neurogenic palsy associated with COVID-19 are likely to be male and present with diplopia secondary to an abducens nerve palsy within 15 days of the onset of the virus. The overall age of the patients in this study varied greatly, as did the time to improvement or resolution of the diplopia.
Whilst the proposed mechanism of development of a neurogenic palsy secondary to COVID-19 infection has not been established, based on the literature, we classified the cases into one of three broad categories: vascular/thrombotic cause, viral neuro-invasive event or an inflammatory virus-mediated immune response.Citation7,Citation9,Citation11,Citation12 The underlying cause for most of the patients with oculomotor nerve palsy was postulated to be viral neuro-invasive or vascular/thrombotic. In contrast, patients presenting with an abducens nerve palsy were more likely to be classified as having an inflammatory cause. Despite the prevalence of a proposed inflammatory virus-mediated immune response in those with abducens nerve palsy, inferences as to mechanisms cannot be made. In particular, the mechanisms were documented for each case as a proposed causal factor based on clinical presentation and investigation. Further research to establish more definite underlying causal mechanisms is required.
Given that this systematic review only included case reports or case series, there are limitations with respect to what conclusions can be drawn. There was much inconsistency between the cases in terms of reporting of symptoms, duration, time to resolution and investigations. Also, proposed mechanisms as to the cause of neurogenic palsies were postulated by the published authors, and for the purposes of this current review, subsequently grouped into three categories. The robustness of these hypotheses has not been unequivocally established, and other mechanisms may need to be considered. However, despite the paucity of literature and the only recent human exposure to SARS-CoV-2, the link between COVID-19 and neurogenic palsies appears strong. Further studies investigating the onset and pathogenesis of neurogenic palsy secondary to COVID-19 infection are required.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Veritti D, Sarao V, Bandello F, Lanzetta P. Infection control measures in ophthalmology during the COVID-19 outbreak: a narrative review from an early experience in Italy. Eur J Ophthalmol. 2020;30(4):621–628. doi:10.1177/1120672120927865.
- Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57(6):365–388. doi:10.1080/10408363.2020.1783198.
- Luís ME, Hipólito-Fernandes D, Mota C, et al. A review of neuro-ophthalmological manifestations of human coronavirus infection. Eye Brain. 2020;12:129–137. doi:10.2147/EB.S268828.
- Nasiri N, Sharifi H, Bazrafshan A, Noori A, Karamouzian M, Sharifi A. Ocular manifestations of COVID-19: a systematic review and meta-analysis. J Ophthalmic Vis Res. 2021;16(1):103–112. doi:10.18502/jovr.v16i1.8256.
- Ni W, Yang X, Yang D, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):422. doi:10.1186/s13054-020-03120-0.
- Andalib S, Biller J, Di Napoli M, et al. Peripheral nervous system manifestations associated with COVID-19. Curr Neurol Neurosci Rep. 2021;21(3):9. doi:10.1007/s11910-021-01102-5.
- Anilkumar A, Tan E, Cleaver J, Morrison HD. Isolated abducens nerve palsy in a patient with asymptomatic SARS-CoV-2 infection. J Clin Neurosci. 2021;89:65–67. doi:10.1016/j.jocn.2021.04.011.
- Choi KD, Choi SY, Kim JS, et al. Acquired ocular motor nerve palsy in neurology clinics: a prospective multicenter study. J Clin Neurol. 2019;15(2):221–227. doi:10.3988/jcn.2019.15.2.221.
- Dinkin M, Gao V, Kahan J, et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020;95(5):221–223. doi:10.1212/WNL.0000000000009700.
- Falcone MM, Rong AJ, Salazar H, Redick DW, Falcone S, Cavuoto KM. Acute abducens nerve palsy in a patient with the novel coronavirus disease (COVID-19). J Aapos. 2020;24(4):216–217. doi:10.1016/j.jaapos.2020.06.001.
- Belghmaidi S, Nassih H, Boutgayout S, et al. Third cranial nerve palsy presenting with unilateral diplopia and strabismus in a 24-year-old woman with COVID-19. Am J Case Rep. 2020;21:e925897. doi:10.12659/AJCR.925897.
- Faucher A, Rey PA, Aguadisch E, Degos B. Isolated post SARS-CoV-2 diplopia. J Neurol. 2020;267(11):3128–3129. doi:10.1007/s00415-020-09987-x.
- Henry B, Vikse J, Benoit S, Favaloro E, Lippi G. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clinica Chimica Acta. 2020;507:167–173. doi:10.1016/j.cca.2020.04.027.
- McFadyen JD, Stevens H, Peter K. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res. 2020;127(4):571–587. doi:10.1161/CIRCRESAHA.120.317447.
- Zhou L, Zhang M, Wang J, Gao J. Sars-Cov-2: underestimated damage to nervous system. Travel Med Infect Dis. 2020;36:101642. doi:10.1016/j.tmaid.2020.101642.
- Riva N, Russo T, Falzone YM, et al. Post-infectious Guillain-Barré syndrome related to SARS-CoV-2 infection: a case report. J Neurol. 2020;267(9):2492–2494. doi:10.1007/s00415-020-09907-z.
- Institue. TJB. The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews checklist for case series. 2022. https://jbi.global/critical-appraisal-tools.
- Bartolo C, Koklanis K, Vukicevic M. ‘Poppers Maculopathy’ and the adverse ophthalmic outcomes from the recreational use of alkyl nitrate inhalants: a systematic review. Semin Ophthalmol. 2022;38(4):1–9. doi:10.1080/08820538.2022.2108717.
- Baccarella A, Linder A, Spencer R, et al. Increased Intracranial Pressure in the Setting of Multisystem Inflammatory Syndrome in Children, Associated with COVID-19. New York, NY: Elsevier B.V.; 2021:48–49.
- Ben-David GS, Halachmi-Eyal O, Shyriaiev H, Brikman S, Dori G, Briscoe D. Diplopia from abducens nerve paresis as a presenting symptom of COVID-19: a case report and review of literature. Arq Bras Oftalmol. 2021;85:182–185.
- Bingol Kiziltunc P, Seven MY, Atilla H. Isolated abducens nerve palsy due to COVID-19. Strabismus. 2022;30(1):35–37. doi:10.1080/09273972.2021.2022718.
- Börü ÜT, Bölük C, Toksoy CK, Demirbaş H. Acute cerebellitis, transverse myelitis and polyradiculoneuritis related to post-COVID-19 infection. J Spinal Cord Med. 2022;45(5):765–768. doi:10.1080/10790268.2021.1969502.
- Capponi M, Cinicola BL, Brindisi G, et al. COVID-19 and abducens nerve palsy in a 9-year-old girl—case report. Ital J Pediatr. 2022;48(1):1–4. doi:10.1186/s13052-022-01298-3.
- Corrêa DG, Hygino da Cruz LC Jr., Lopes FCR, et al. Magnetic resonance imaging features of COVID-19-related cranial nerve lesions. J Neurovirol. 2021;27(1):171–177. doi:10.1007/s13365-020-00934-0.
- de Oliveira MR, Lucena A, Higino TMM, Ventura CV. Oculomotor nerve palsy in an asymptomatic child with COVID-19. J Aapos. 2021;25(3):169–170. doi:10.1016/j.jaapos.2021.02.001.
- Elenga N, Martin E, Gerard M, Osei L, Rasouly N. Unilateral diplopia and ptosis in a child with COVID-19 revealing third cranial nerve palsy. J Infect Public Health. 2021;14(9):1198–1200. doi:10.1016/j.jiph.2021.08.007.
- Fitzpatrick JC, Comstock JM, Longmuir RA, Donahue SP, Fitzpatrick JM, Bond JB. Cranial Nerve III Palsy in the setting of COVID-19 infection. J Neuroophthalmol. 2021;41(3):e286–e7. doi:10.1097/WNO.0000000000001160.
- Hernandez-Garcia E, Arriola-Villalobos P, Burgos-Blasco B, Morales-Fernandez L, Gomez-de-Liano R. Sixth nerve palsy in pediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2 infection. J Neuroophthalmol. 2022;42(1):e406–e7. doi:10.1097/WNO.0000000000001292.
- Kubota T, Sugeno N, Sano H, et al. The immediate onset of isolated and unilateral abducens nerve palsy associated with COVID-19 infection: a case report and literature review. Internal Medicine. 2022;61(11):1761–1765. doi:10.2169/internalmedicine.9308-22.
- Manolopoulos A, Katsoulas G, Kintos V, et al. Isolated abducens nerve palsy in a patient with COVID-19: a case report and literature review. Neurologist. 2022;27(3):139–142. doi:10.1097/NRL.0000000000000382.
- Medeiros AL, Martins T, Kattah M, et al. Isolated abducens nerve palsy associated with coronavirus disease: an 8-month follow-up. Arq Bras Oftalmol. 2022;85(5):517–519. doi:10.5935/0004-2749.20220063.
- Oliveira RMC, Santos DH, Olivetti BC, Takahashi JT. Bilateral trochlear nerve palsy due to cerebral vasculitis related to COVID-19 infection. Arq NeuroPsiquiatr. 2020;78(6):385–386. doi:10.1590/0004-282x20200052.
- Ordás CM, Villacieros-Álvarez J, Pastor-Vivas AI, Corrales-Benítez Á. Concurrent tonic pupil and trochlear nerve palsy in COVID-19. J Neurovirol. 2020;26(6):970–972. doi:10.1007/s13365-020-00909-1.
- Piazza F, Bozzali M, Morana G, et al. Early reversible leukoencephalopathy and unilateral sixth cranial nerve palsy in mild COVID‑19 infection. Neurol Sci. 2021;42(12):4899–4902. doi:10.1007/s10072-021-05545-z.
- Prajwal S, Ikechukwu A, Bharosa S, Benjamin M. Superior divisional palsy of the oculomotor nerve as a presenting sign of SARS-CoV-2 (COVID-19). J Investig Med High Impact Case Rep. 2022;10:23247096211058490. doi:10.1177/23247096211058490.
- Soto Insuga V, Cantarín-Extremera V, Solís-Muñoz I, et al. Pseudotumor cerebri caused by SARS-CoV-2 infection in a boy. J Pediatr Neurol. 2021;19(3):207–209. doi:10.1055/s-0040-1715857.